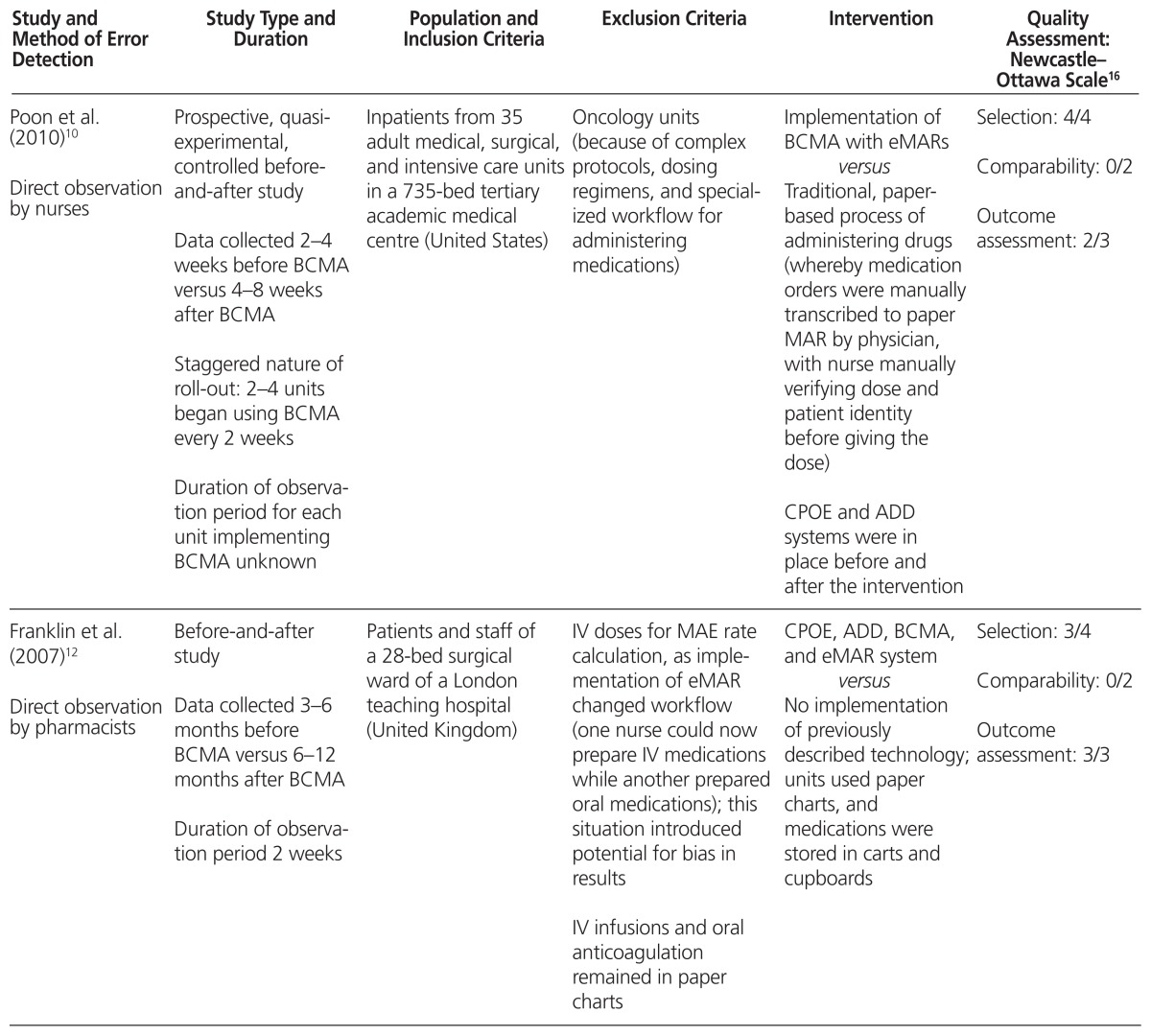
Table 1.
Characteristics of Included Studies
| Study and Method of Error Detection | Study Type and Duration | Population and Inclusion Criteria | Exclusion Criteria | Intervention | Quality Assessment: Newcastle–Ottawa Scale16 |
|---|---|---|---|---|---|
| Poon et al. (2010)10 Direct observation by nurses |
Prospective, quasi-experimental, controlled before- and-after study Data collected 2–4 weeks before BCMA versus 4–8 weeks after BCMA Staggered nature of roll-out: 2–4 units began using BCMA every 2 weeks Duration of observation period for each unit implementing BCMA unknown |
Inpatients from 35 adult medical, surgical, and intensive care units in a 735-bed tertiary academic medical centre (United States) | Oncology units (because of complex protocols, dosing regimens, and specialized workflow for administering medications) | Implementation of BCMA with eMARs versus Traditional, paper-based process of administering drugs (whereby medication orders were manually transcribed to paper MAR by physician, with nurse manually verifying dose and patient identity before giving the dose) CPOE and ADD systems were in place before and after the intervention |
Selection: 4/4 Comparability: 0/2 Outcome assessment: 2/3 |
| Franklin et al. (2007)12 Direct observation by pharmacists |
Before-and-after study Data collected 3–6 months before BCMA versus 6–12 months after BCMA Duration of observation period 2 weeks |
Patients and staff of a 28-bed surgical ward of a London teaching hospital (United Kingdom) | IV doses for MAE rate calculation, as implementation of eMAR changed workflow (one nurse could now prepare IV medications while another prepared oral medications); this situation introduced potential for bias in results IV infusions and oral anticoagulation remained in paper charts |
CPOE, ADD, BCMA, and eMAR system versus No implementation of previously described technology; units used paper charts, and medications were stored in carts and cupboards |
Selection: 3/4 Comparability: 0/2 Outcome assessment: 3/3 |
| Helmons et al. (2009)11 Direct observation by pharmacists and pharmacy students |
Prospective, before-and-after observational study Data collected 1 month before BCMA versus 3 months after BCMA Staggered roll-out over 1 year Duration of observation period for each unit implementing BCMA unknown |
Patients in 2 medical-surgical units and 2 ICUs of a 386-bed academic teaching hospital (United States) | Medication administration during emergencies | BCMA technology (medication administration checked with software system) interfaced with CPOE and pharmacy information system versus MAR printed once daily serving as a paper reference for medications to be delivered to patients and completed that day; hospital CPOE system that was already implemented had to be regularly checked for new or modified medication orders, and any changes had to be transcribed onto the MAR |
Selection: 4/4 Comparability: 0/2 Outcome assessment: 2/3 |
| Richardson et al. (2012)14 Self-reporting |
Medication error rates recorded on the basis of a before- and-after approach Study focused on key steps guiding clinical nurse specialists to improve safety of medication administration by implementing BCMA, with phased-in approach over 3 years; scanning rates were recorded in 3 phases (months 6–13, months 14–24, and months 25–36) |
Not stated (United States) | Not stated | Implementation of eMAR and BCMA, followed by implementation of CPOE versus Traditional paper system with ADDs already in place |
Selection: 4/4 Comparability: 0/2 Outcome assessment: 2/3 |
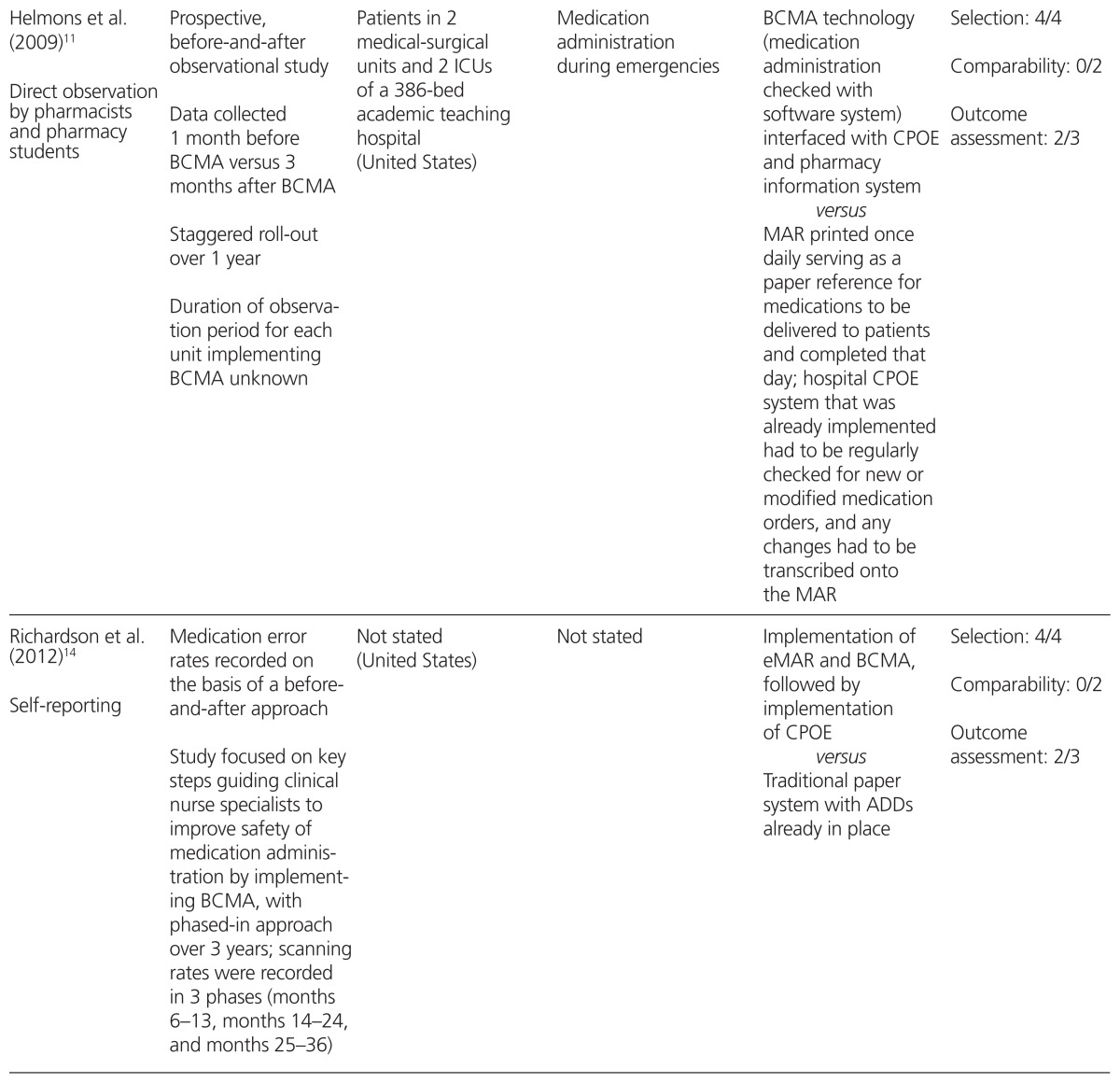
| Higgins et al. (2010)13 Self-reporting |
Before-and-after study in a large teaching hospital with retrospective analysis; pre-implementation data collected from 2007 to April 2008; post-implementation data collected from April 2008 to 2009 | Administration of medication to patients from the Baystate Medical Center, a 655-bed general acute tertiary care teaching hospital (United States) | Medication administration errors in the emergency department (which did not have BCMA) | Implementation of bar code scanning for positive identification of patient versus No bar code administration system CPOE and ADD already in place |
Selection: 4/4 Comparability: 0/2 Outcome assessment: 2/3 |
ADD = automated dispensing device, BCMA = bar code medication administration, CPOE = computerized prescriber order entry, eMAR = electronic medication administration record, ICU = intensive care unit, MAE = medication administration error, MAR = medication administration record.