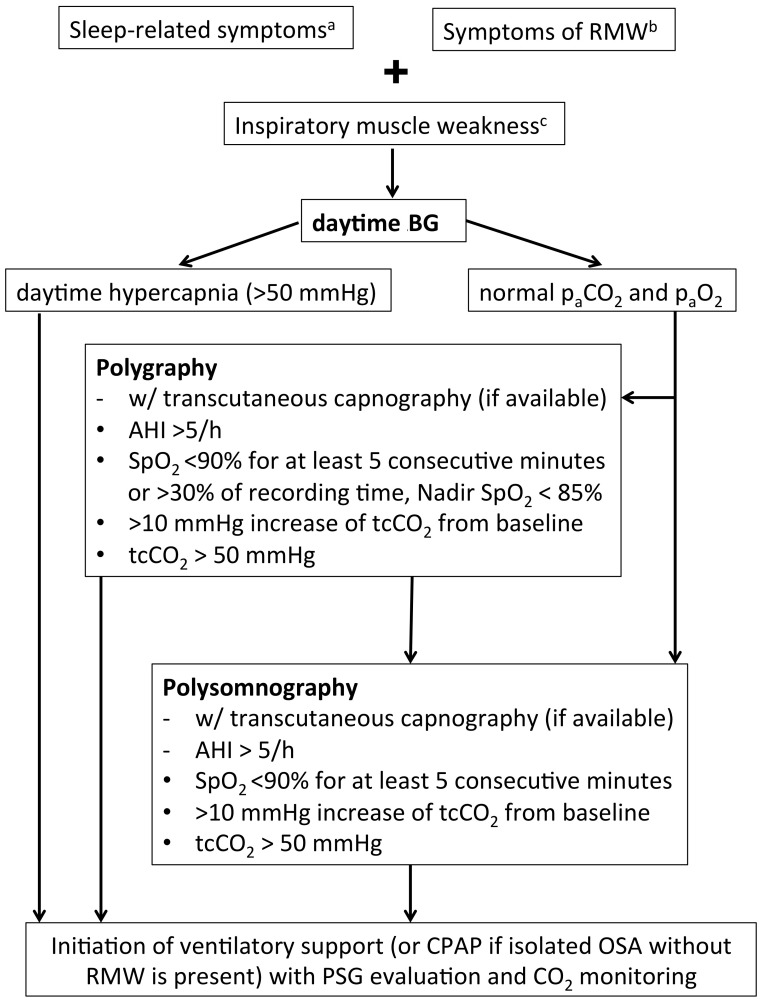
Figure 1.
Recommendations for sleep studies in patients with LOPD. Isolated nocturnal tachypnea or lone increase of base excess on early-morning blood gas analysis may both be indicative of nocturnal hypoventilation but do not justify ventilatory support. However, both scenarios should give rise to monitor patients in shorter intervals. a sleep disruption, morning headache, daytime hypersomnolence; b dyspnea, orthopnea; c VC < 50% predicted, VC postural drop > 40%, MIP < 60 cm H2O, SNIP < 40 cm H2O. VC, vital capacity; RMW, respiratory muscle weakness; paCO2, carbon dioxide tension; paO2, oxygen tension; AHI, apnea hypopnea index; SpO2, oxygen saturation; tcCO2, transcutaneous carbon dioxide tension; CPAP, continuous positive airway pressure; OSA, obstructive sleep apnea; PSG, polysomnography; SNIP, sniff nasal inspiratory pressure; MIP maximum inspiratory pressure.