Abstract
Background
Mobile phone Short Message Service (SMS) is a tool now used by the health research community, providing the capability for instant communication between patients and health professionals. Greater understanding of how to best utilize SMS as a means to improve healthcare delivery and outcomes will foster innovation in research and provide an opportunity to progress as a public health community.
Purpose
The purposes of this systematic review were two-fold: (1) to provide insight on the most utilized mobile phone SMS practices and characteristics in hypertension (HTN) outcome-focused publications, and (2) to critically evaluate empirical evidence associated with SMS utilization and blood pressure (BP) outcomes.
Methods
Two independent systematic literature searches were completed. The final selected studies each then underwent data extraction and quality-rating assessment, followed by an evaluation for a meta-analysis to measure mean difference of the change in BP.
Results
A total of 6 studies meeting the inclusion criteria were included in the review. Feasibility assessment for a meta-analysis was found unfavorable due to the variation among studies. SMS interventions focused on BP management were most effective in studies featuring two-way communication and individual patient-tailored content, and guided by evidence-based HTN management practices.
Implications
SMS interventions for HTN management were supported through evidence provided by the studies reviewed. SMS holds strong potential to bring greater innovation to HTN management and care, especially in racial/ethnic minority populations that face psychosocial and structural barriers in health care access and utilization.
Keywords: Short messaging system, hypertension, mHealth
Background
Cardiovascular disease (CVD) continues to be the leading cause of death in the United States (US), accounting for approximately 1 in every 4 deaths.1 Hypertension (HTN) is a major risk factor for CVD, affecting 33% or 80 million of US adults (20+ years old) in 2012.2 Globally, it is estimated that nearly 22% of all adults aged 18 and older had high blood pressure (BP) in 2014.3 In 2010, uncontrolled HTN alone contributed to an estimated 9.4 million deaths worldwide.3 Additionally, the economic costs associated with HTN management and care are substantial. According to the American Heart Association, in 2011, HTN accounted for an astounding 46.4 billion dollars in direct and indirect costs to the US healthcare system.2 Varying types of non-pharmacological interventions have been developed and tested with aims to improve BP control4; one of the more recent approaches is the use of mobile phone short message service (SMS) communication.
Entering the 21st century, SMS has quickly become a ubiquitous communication method for many individuals worldwide. Within the US, SMS continues to be the topmost used mobile phone feature, even among Smartphone owners.5 SMS is commonly described as “text messaging,” or a “short alphanumeric communication sent from one mobile phone user to another with messaging applications.”6 This recent yet overwhelmingly popular technological innovation falls within the domain of mobile health (mHealth). The World Health Organization defines mHealth as “a medical and public health practice supported by mobile devices,” including mobile phones.7 The opportunity that SMS can provide as an effective health communication and data-tracking tool in health management has already been demonstrated for a number of diseases and health topics.8 This opportunity may be related to global availability and access to mobile phones – the United Nations’ International Communication Union reported that at the end of 2014, mobile phone subscriptions globally approached an astounding 7 billion, drawing near to the entire human population.9 Specifically within the US, recent studies indicate that in 2013 91% of all adults owned and used a mobile phone and of those, 81% used SMS.10
SMS is becoming a transformational tool for the public health community to utilize in the delivery of better quality care and health promotion, including within the realms of prevention and management of chronic diseases such as HTN. Consequently, identifying the most effective uses of SMS for any particular health issue or target population is essential to future mHealth research programming. Systematic reviews and meta-analysis on SMS-based interventions provide researchers useful insight on the most promising uses of SMS in supporting healthcare and disease prevention and management. While much of the literature focused on CVD prevention that utilizes SMS has been on diabetes mellitus (DM) management,11 there is limited study of BP outcomes,12 despite the fact that HTN and DM are both recognized as significant CVD risk factors that require chronic management.2 To our knowledge, this review is the first specifically focused on SMS use for HTN management. This study was designed to systematically review and conduct a meta-analysis of interventions that utilized SMS to improve BP control among their participants, and to provide recommendations for SMS utilization within HTN care.
Methods
This study used guidelines for primary process and reporting methods outlined by The Cochrane handbook for systematic reviews of interventions13 and The Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement.14 Supplemental information pertaining to the intital steps that were carried out for a meta-analysis was also reported to provide further insight into the overall state of the research literature to date.
Eligibility criteria
The following inclusion and exclusion criteria were set for the search and selection of literature to systematically review and assess for meta-analysis. Publications had to (a) describe either a quasi-experimental or randomized controlled trial (RCT), (b) target an adult population (18+ years old), (c) integrate HTN prevention or management, (d) evaluate BP as outcome measures, and (e) utilize SMS as an intervention component. To avoid discrepancy, we defined SMS as a mobile phone’s text message service with sending and receiving message capability, typically under 160 alphanumeric characters in length, to either another mobile phone or a web-based system; this designation excluded mobile-phone communication using applications or email. SMS also did not need to be the primary component used in a study to be included. Publications had to be available in (f) full-text, and (g) English, Korean, or Spanish, the languages fluently spoken by our author team. There were no limits on year published, as SMS is a relatively new technology with earliest publication involving a health intervention appearing in 2002.14 Studies utilizing SMS that primarily addressed CVD such as stroke, metabolic syndrome, kidney disease, heart failure, or acute coronary syndrome were excluded, regardless of whether BP was an outcome measure, as these diseases can independently impact BP outcomes.
Sources of information and search strategy
Two reviewers (EW and MC) conducted independent systematic literature searches using PubMed, CINAHL, Embase, Cochrane, Scopus, and PsycINFO for articles that were published as of July 2015. A medical librarian assisted in the creation of database search terms. The following Mesh terms were used in multiple combinations: text messaging, text message, text messages, texts, texted, texting, SMS, short message service, short messaging service, hypertension, high blood pressure, essential hypertension, diabetes mellitus, diabetes mellitus, cholesterol, tobacco smoking, passive smoking, smoking, smoker, smokers, diet, obesity, motor activity, physical activity, exercise, aerobic exercise, weight lifting, yoga (see Appendix for a full electronic search strategy). To reinforce search quality, the team completed two additional unique searches. A review of previously published mHealth or SMS-focused systematic review articles was completed to follow a cross-reference search for articles that fit our review’s inclusion criteria. Finally, a search on ClinicalTrials.gov for relevant completed studies pending publication was completed. If a study fit the inclusion criteria, its respective Principal Investigator (PI) was contacted for a copy of the study methods and results.
Screening, data extraction, and critical appraisal
Upon finalization of the articles for this systematic review, the data extraction and quality ratings were performed. The following items were extracted from each article: author, year, country, target behavior, study design, aims, intervention, duration, sample size, and evaluation method and outcome measures. SMS-specific intervention collected separately, including SMS type, dosage, frequency, transmission, examples, and any relevant evaluation. A quality rating assessment using a bias rating tool13 was then completed for each study. EW and MC independently assessed and rated each study based on the quality criteria. Any discrepancies were reconciled by a team consensus.
Statistical analysis
We worked toward completing a meta-analysis to assess the pooled effect size of the selected studies. The primary outcome was the mean difference in the change in BP measurement from baseline at the final time point between the intervention and control groups. In the case of any unreported data required for the meta-analysis, communicating efforts with the study’s corresponding author were made. Afterward, any data that was not able to be obtained was estimated using conservative calculation recommended in a report by the Agency for Healthcare Research and Quality (US).16 Meta-analysis calculations were completed using STATA 11 (College Station, TX) with the metan command. The forest plots of the pooled mean differences of changes in systolic and diastolic BP from baseline were presented using 95% confidence intervals. Using the I2 statistic, the clinical and methodological heterogeneity (e.g., participants, interventions, designs, outcomes, or quality ratings) among the studies was assessed to determine the feasibility of meta-analysis.13 If substantial variances resulted (i.e., I2 values greater than 50%), studies could not be pooled and each study would have to be separately reviewed and summarized.13
Results
Search results
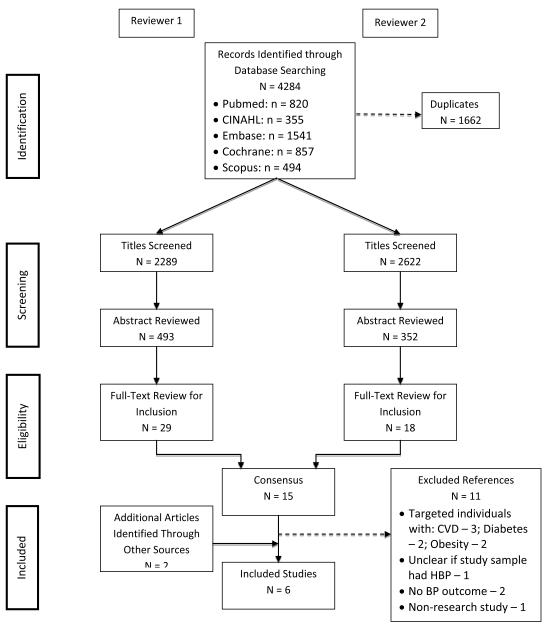
The initial independent database searches identified over 3,000 related articles for each reviewer. After duplicates were removed and article titles were screened, EW and MC examined abstracts for 493 and 352 articles, respectively. From these articles, the full-text review for inclusion criteria yielded EW with 29 articles and MC with 18 articles. The whole team then conducted full-text reviews of these 47 articles and met to discuss any selection discrepancies among the eligible articles. The result was 32 removals from the eligible articles due to failure to meet all inclusion criteria during more thorough text examinations, such as having targeted individuals with CVD, lacked clarity whether the study included participants with CVD, failed to measure BP outcomes, or been labeled a non-research study. A cross-reference search on 17 SMS-focused systematic reviews yielded 1 additional eligible article. Similarly, the search on ClinicalTrials.gov resulted in 1 additional clinical trial study that met the inclusion criteria. Figure 1 provides a search tree describing the steps taken to reach final consensus of the total studies selected.
Figure 1.
Search Tree
Summary of studies
A total of 6 studies were included to complete a systematic review and be assessed for meta-analysis. A summary of the studies’ characteristics can be found Table 1. Five studies identified as RCT, one as quasi-experimental. All studies took place internationally, more specifically two in Spain,17, 18 one in Russia,19 one in China,20 one in South Korea,21 and one in the Philippines.22 The studies’ targeted behaviors included a partial or sole focus on HTN management, while two of the studies also focused on weight loss.20,21 Each study’s intervention and control groups’ SBP and DBP outcomes were collected, and reported in Table 1 using the baseline and difference from baseline at final point measurements. Intervention duration ranged from 2 to 12 months. A total of 1,466 study participants (949 after attrition) were included in this review. The target population was limited to patients, though one study also chose to enroll general providers (GP).17 Participants were recruited based on the presence of a specific disease (i.e., HTN) or health behavior (i.e., weight loss). The average age of the patient-participants was 53.6 years, and 55.3% were female.
Table 1.
Study Characteristics
| 1st Author (Year), Country |
Target Behavior |
Study Design & Duration |
Sample N=baseline→evaluation |
Intervention | Outcome Measures & Evaluation |
Principal Findings |
|---|---|---|---|---|---|---|
| Carrasco (2008), Spain |
HTN | RCT 6 months |
Sample Size: N= 285→273 (IG: 142→131, CG: 143→142) Mean age: IG: 62.1 years, CG: 62.8 years Female: IG: 39.7%, CG: 40.8% |
IG: reported BP, HR, and weight to their GP weekly via SMS + (GP feedback optional) CG: self- measured BP, HR, and weight weekly + reported their measures in- person during routine visits |
Primary: degree of HTN control and uncontrolled HTN at 6 months Secondary: BP, HR, quality of life, anxiety survey scores, number of consultation visits, and hospital admissions Evaluation: baseline and 6 months |
|
| Kiselev (2012), Russia |
HTN | RCT 12 months |
Sample Size: N= 199→164 (IG: 97→62, CG: 102) Mean age: IG: 49 years, CG: 51 years Female: IG: 45%, CG: 50% |
IG & CG (at baseline): prescribed medication, encouraged to measured BP at home, and received informational brochures IG: daily/weekly SMS for 12 months CG: standard care |
Primary: BP goal of 135/85 mmHg Secondary: weight loss and smoking cessation Evaluation: baseline, 6, and 12 months |
|
| Lin (2014), China |
Weight loss |
RCT 6 months SMS component was supplemental |
Sample Size: N=123→110 (IG: 63→56, CG: 60→54) Mean age: IG: 38.35 years, CG: 38.07 years Female: IG: 60.32%, CG: 60% |
IG: daily SMS + goal setting + 3 group education sessions + 5 coaching calls CG: brief education information at baseline |
Primary: weight change Secondary: BP, BMI, waist circumference, body fat (%), dietary intake, physical activity, and psychosocial factors Evaluation: baseline and 6 months |
|
| Márquez- Contreras (2014), Spain |
HTN | RCT 6 months |
Sample Size: N= 104→67 (IG: 52→34, CG: 52→33) Mean age: IG: 56.3 years, CG: 59.4 years Female: IG: 47.1%, CG: 42.4% |
IG & CG (at baseline): printed HTN information and prescribed medication IG: weekly SMS for 4 months CG: standard of care |
Primary: Patient percentage compliance score, based on medication adherence Secondary: BP and weight Evaluation: baseline, 1, 3, and 6 months |
|
| Palileo- Villanueva* (reference 16), Philippines |
HTN | RCT 3 months |
Sample Size: N= 700→286 (IG: 350→151, CG: 350→135) Mean age: IG: 59 years, CG: 59.6 years Female: IG: 66.1%, CG: 64.4% |
IG: weekly medication adherence reminders via SMS CG: standard of care |
Primary: SBP and DBP Secondary: medication adherence (self- report) and SMS acceptability survey Evaluation: baseline and 3 months |
|
| Park (2009), South Korea |
HTN, Weight loss |
Quasi- experimental 2 months |
Sample Size: N= 55→49 (IG: 30→28, CG: 25→21) Mean ages: IG: 53.2 years, CG: 54.6 years Female: IG: 39.3%, CG: 57.1% |
IG: reported BP, weight, and medication information weekly via SMS or web- based diary + tailored feedback from study staff CG: provided with study information only |
Primary: BP, weight, waist circumference, and serum lipids Evaluation: baseline and 2 months |
|
Data available from https://clinicaltrials.gov
Abbreviations Key: Blood Pressure (BP), Body Mass Index (BMI), Cardiovascular disease (CVD), General Provider (GP), Heart Rate (HR), High blood pressure (HBP), Hypertension (HTN), Intervention Group (IG), Randomized Controlled Trial (RTC)
SMS characteristics
The studies’ SMS characteristics are summarized in Table 2. The SMS component of each study was classified as either the main or a supplemental component of the intervention. Only one study integrated SMS into its intervention as a supplemental component,20 while the other five used SMS as the main component, with18,19 or without17, 21,22 non-SMS supplemental components. For example, the Lin study integrated a supplemental SMS component, sending patient-participants daily SMS to track their weight loss goal progress, with supporting education sessions and telephone coaching call components. Two studies18,22 restricted SMS transmission to one-way communication (only the study team sending the SMS). The other four studies17,19-21 allowed for two-way communication, with the study teams always initiating the SMS communication with participants. SMS communication frequency also varied, with SMS being sent daily by two studies,19,20 weekly by four studies,17,18,21,22 and specific event-initiated (e.g., unstable BP measurements were noted) by one study.19 Of the studies that sent SMS daily, only one study sent multiple SMS per day.20
Table 2.
SMS utilization and characteristics
| 1st Author (Year) |
Content & Topics | Transmission | Frequency | SMS Examples* |
|---|---|---|---|---|
| Carrasco (2008) |
Self-report measurements & progress: BP, HR, and weight data Feedback & commentary (optional): GP’s HTN management feedback |
2-way (SMS feedback from GP was optional) |
Weekly, 4× per week (BP), 1× per week (HR and weight) |
None available |
| Kiselev (2012) |
Medication reminders: BP home monitoring, HTN medication, weight loss and smoking cessation support reminders Self-report measurements & progress: BP, weight, and number of cigarettes smoked data Feedback & commentary: emphasized specific HTN management recommendations based on each participant’s self- reported data Appointment scheduling: prompted by a drastic change in participant’s self-reported BP data |
2-way | Daily (medication), weekly (weight, number of cigarettes smoked) Feedback Algorithm: (Daily) – initiation of new BP med/missing BP reading/increase of 20mmHG in SBP from last visit (Weekly) – change in BP med / increase of <20mmHg in SBP from last visit (Monthly) – constant or decrease in SBP from last visit (Semi-annually) – constant or decrease in SBP during the last 6 months |
None available |
| Lin (2014) |
Self-report measurements & progress: weight loss assigned goal progress data from the previous day Feedback & Commentary: tailored feedback based on each participant’s self-reported goal progress |
2-way | Daily (weight loss progress) | Goal progress requests:
|
| Márquez- Contreras (2014) |
Educational information: HTN information, and good health and diet habits Medication reminders: HTN medication |
1-way (study team → participant) |
Weekly | “Always take your BP pill when you get up in the morning” “Remember that the effect of BP pills wears off after 24 hrs. Some patients have serious problems because they don’t take their pill every day” “Try to take your pills exactly as your doctor advised you. This ensures that your treatment will be useful” |
| Palileo- Villanueva (reference 16) |
Educational information: target BP and benefits of HTN treatment Medication reminders: HTN medication |
1-way (study team → participant) |
Weekly | None available |
| Park, M. (2009) |
Self-report measurements & progress: BP, weight, diet and exercise, and medication information data Feedback & commentary: HTN management feedback that was based on each participant’s self- reported data |
2-way | Weekly | “The frequency of the fast food intake was five times last week, please decrease the frequency in two times” “Your exercise duration was 20 minutes last week, you need 10 minutes more” |
Original SMS used did not use abbreviated wording
Abbreviations Key: Blood Pressure (BP), General Provider (GP), Heart Rate (HR), Hypertension (HTN)
The SMS types used among the studies varied both within and between the studies and were sorted into 5 categories: (1) SMS that provided medication reminders were used in three studies,18,19,22 sent daily in one study17 and two days per week in the two other studies;18,22 (2) SMS to schedule clinic appointments were used in one study19, sent during specific events such as when a participant had unstable self-reported BP; (3) SMS to disseminate educational information (e.g., good health and dietary habits) were sent two days per week in two studies;18,22 (4) SMS to provide self-report measurements and progress to the research team, sent by the participants themselves, were used in four studies.17, 19 –21 The types of self-reported information sent by participants included BP,16,18,20 heart rate,16 weight,16,18,20 number of cigarettes smoked,19 medication intake record,21 and behavioral goal progress.20 SMS to self-report information were sent by participants on a daily basis in one study,20 and on a weekly basis in three studies;17,19,21 finally, (5) all four studies using SMS to self-report information also used SMS to provide individualized feedback and commentary on behalf of the research teams or GPs17 and were sent in response to the SMS with self-report information provided by participants.
Effects of SMS intervention
Evaluation of the effects of SMS was primarily based on the studies’ BP outcomes and then supported by other clinical and behavioral outcome measures. BP measurements used to calculate outcomes were collected in clinical settings and by trained researchers. The BP data that was self-reported by participants (via SMS) was only used to develop the individualized feedback and commentary content, and/or evaluated as a secondary outcome. The six studies’ evaluation content identified that only three studies19 –21 reported improved BP outcomes in their SMS interventions and expressed overall positive outlooks on SMS usage in HTN management care. No significant BP outcome results were reported by the authors of three SMS interventions.17,19,22 However, the unpublished Palileo-Villanueva study had not yet completed discussion on their outcome results. One study that found no significant results in their SMS intervention evaluated medication adherence as a behavioral outcome.18 Per request at various time points, participants brought in their HTN medication(s) and the study team proceeded to discreetly count the individual pills to calculate medication adherence. The use of SMS for medication reminders alone demonstrated no significant improvements in adherence.19
Process evaluations of participants’ responses to SMS and their level of utilization were completed in five studies.17,19 –22 In two studies,19,21 participants were withdrawn if non-compliant in corresponding to SMS after one month. Reasons cited for non-compliance included “loss of interest in the intervention” and “technical difficulties with the SMS” in the Kiselev study. Participants’ experiences and receptiveness to utilizing SMS were documented at the end in two studies,20,22 and both indicated overall favorable responses. One study reported that 95% of participants felt SMS was helpful in achieving their weight loss goals,20 while 99% of participants from the second study reported that “receiving health information through text is helpful.”22 Lastly, one study measured the GP-participants’ SMS utilization by recording the total number of SMS sent to the patient-participant arm.17 50% of the patient-participants failed to receive any SMS, indicating low levels of GP SMS utilization.17
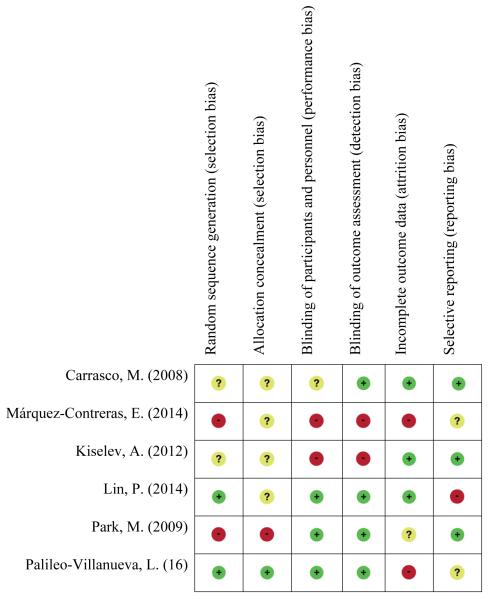
Quality ratings
The quality-rating assessments determined five studies with high risk of bias and one with an unclear risk of bias.17 Overall, studies did not provide sufficient information to assess bias in their randomization of study participants, a critical component of RCTs. High risk for selection bias was found among all six studies. Further, only two studies20, 22 randomly assigned participants, and only one of those also22 used allocation concealment on study personnel. Figure 2 summarizes our quality-rating findings.
Figure 2.
Quality ratings
Meta-analysis
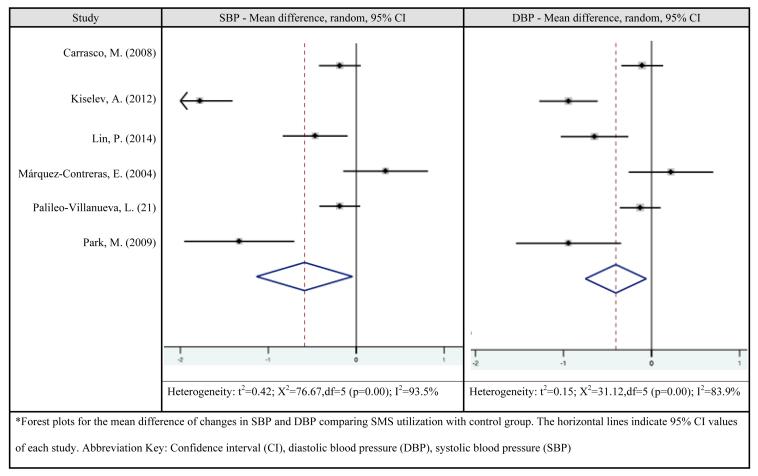
Meta-analysis was attempted using the six studies. We first addressed the issue of unreported data (i.e. standard deviations and mean BP data at baseline and final time point) in three study articles19-21 that were required to assess the primary outcome. The three studies’ corresponding authors were contacted via email to obtain the unreported data, but only one study19 provided the requested data. More than one attempt was made to reach the two other studies’ corresponding authors, but we were unable to obtain the unreported data and therefore used the conservative approaches outlined prior.16 A comparison for similarities in the participants, interventions, and outcomes indicated moderate clinical heterogeneity. A comparison for similarities in the study design and risk of bias suggested slight heterogeneity. Combined, the heterogeneity was on the border of significance and we thus continued with testing the statistical heterogeneity. Mean difference calculations of SBP and DBP resulted in I2 of 93.5% and 89.9%, respectively, indicating that the statistical heterogeneity was substantial (Figure 3 for forest plots). Consequently, no further steps were taken to complete the meta-analysis.
Figure 3.
Forest plot variance
Discussion
Our systematic review reveals that three19 –21 of the six studies had significant improvement in BP outcomes as a result of their SMS component alone or in combination with other components (e.g., telephone coach calls). SMS was most effective in those interventions with: two-way communication, individualized patient-tailored content, and a combination of other evidence-based HTN management support effort practices (e.g., health education group sessions). Of three studies that used medication reminder SMS,18,19,22 the Kiselev study allowed for two-way SMS transmission may contributed considerably to the significant BP outcome exhibited in only the intervention group. Better BP outcomes in the studies with two-way SMS transmission may have stemmed from the increased communication between the patients and study team. It very well may be that HTN patients are more likely to adhere to medication if their health provider is actively monitoring their treatment progress. Moreover, when patients have to routinely self-monitor and report BP for example, an inherent automatic reinforcement about their current BP status is achieved and potentially encourages healthier conscious decision-making. The finding is consistent with other non-SMS studies of HTN in which active and effective communication between healthcare teams and their patients resulted in improved adherence to HTN treatment.23
A comparison between studies using generic versus individualized SMS demonstrates patient-participants were more likely to benefit with individualized SMS. Three studies17,20,21 employed individualized SMS, including study team communication such as feedback to a patient that was based on their most up-to-date self-reported progress; resulting in significantly improved BP levels in two of the studies.20,21 Findings from this review suggest that patients may benefit more from SMS communication that tailors its content to be most relevant to each individual’s own HTN management progress. The adherence to BP self-monitoring at home may become less challenging to patients when there is a scheduled cue to initiate and report the information to a health provider who is actively waiting to review it. Evidence supports the utility of individualized approach (as opposed to generic, non-individualized) communication aimed toward changing specific health behaviors connected to HTN management.24 In consideration of these, future SMS intervention should aim to be individualized to the patient’s profile as much as possible.
Frequency of SMS and study duration varied widely, posing a challenge for a close comparison of results across the studies and limited our ability to infer the frequency and length of time optimal for SMS utilization impact. Daily self-report measurement and progress and feedback and commentary SMS was sent in only the Lin study. While the Kiselev study sent daily medication reminder SMS, and weekly self-report measurement and progress and feedback and commentary SMS. Nevertheless, both studies showed significantly better BP outcomes. Care should be taken to prevent the possibility of overwhelming participants with too many different category SMS on a daily basis, and prioritization of designating the highest frequency to self-report information and progress, and individualized feedback and commentary SMS. Educational information SMS was sent on a weekly basis in two studies,18,22 however, did not show a direct contribution to significant clinical and behavioral outcome results. A comparison of the Park, Link, and Kiselev studies shows noticeable differences in study duration (2, 6, and 12 months, respectively), implying that the content and transmission type of the SMS may have had greater influence on BP outcomes than the study duration alone. Future research is warranted to explore adequate frequency and duration of SMS in addressing the needs of individuals with HTN.
Overall, SMS utilization in HTN management was limited in terms of effectiveness if either party involved was not fully engaged and accepting of SMS. In the Carrasco study for example, the GP exhibited low SMS utilization and infrequently sent feedback and commentary SMS to patients self-reporting BP data. Efforts towards emphasizing the potential benefits and utility of SMS are needed in order to increase receptiveness among HTN patients and the healthcare system. In order to effectively utilize SMS in HTN management, expectations for SMS communication should also be set and clear. The results suggest a need for future research to understand which types of SMS are most helpful or lead to behavioral change in patients. Maintaining high-rigor in methodological qualities remained a challenge for the reviewed studies. For example, only two studies20,22 used an RCT design. Limited sample sizes with predominantly white samples were also notable methodological challenges faced by the studies included in this review. Only three studies had statistical power 80% to address BP outcomes,17,21,22 while the remaining three studies had inconclusive results due to either no statistical power reported18,19 or an unknown sufficient statistical power reference.20 To further improve understanding on how best capitalize on the benefits of SMS, future research that more rigorously evaluates the effect of SMS on HTN management and outcome in a larger, diverse sample of HTN using an RCT is warranted.
There are a number of study limitations. Due to the contrasted nature of studies included in our review, we were unable to complete a meta-analysis. Further, the number of identified studies that met our inclusion criteria was considered too small for any further consideration to separately meta-analyze only a few of the six studies. A close direct comparison of the findings was also limited due to the variation in evaluation methods used by studies. While only three studies in this review reported overall positive feedback with respect to utilizing SMS, strict comparison across these studies remained difficult due to their differences in SMS usage and its evaluation. These observations reinforce and may partly explain the clear variation of the studies in the forest plots. More studies isolating the effects of SMS on HTN management are needed to provide additional insight into the best SMS practices for HTN management. Due to the nature of the primary studies, certain biases could not fully be avoided, such as blinding of research staff (performance bias). However, special consideration should be given to potentially avoidable biases (e.g., ensuring allocation concealment) that can impact the validity of the primary study’s outcome results and degree of statistical heterogeneity when pooling primary studies. In order to enable completion of a meta-analysis and maximize effect size and precision in future reviews subsequent studies should do their best to ensure adequate statistical power and sufficiently large sample size. Nonetheless, the studies reviewed herein have provided multiple factors that are key when designing and pursuing HTN management interventions using mHealth, specifically SMS. Future SMS research addressing BP outcomes should consider a comprehensive assessment of the attitudes and experiences of participants with the SMS component’s utility. Finally, cost effectiveness was also not mentioned in any of the study interventions reviewed, limiting this review’s understanding of their general feasibility going forward.
In summary, our systematic review provides a more comprehensive appreciation to CVD and its risk factors, specifically HTN management and prevention interventions that are supported by SMS. To our knowledge, this review is the first to focus on SMS-specific mHealth research publications surrounding BP management. Our review provides invaluable insight into how SMS can be applied as a tool to support BP control and play a role in addressing the current HTN burden. SMS can provide a pivotal path toward ameliorating the existing disparities surrounding HTN awareness, management, and control experienced by US racial and ethnic communities.25 These disparities are linked to a number of barriers to healthcare that range from a patient’s lack of insurance coverage and limited financial resources to poor communication with their provider and non-adherence to provider instructions. Integrating SMS into health programming appears to represent a viable method of mitigating the negative impact of the latter factors, enabling patients to better and more regularly communicate with health professionals over time. The positive impact of SMS on mitigating racial/ethnic disparities is further enhanced by widespread mobile phone ownership among African Americans/non-Hispanic blacks and Hispanics/Latinos (93% and 88%, respectively).10 Overall, the use of SMS in HTN management is supported by the evidence provided within the six studies reviewed and can become a practical and influential instrument in HTN management and care efforts.
What’s New?
SMS interventions that allowed for two-way communication were most effective in supporting patients achieve their BP goals.
Tailoring the content of the SMS message to each patient and combining SMS with evidence-based HTN management practices helped improve BP outcomes.
Acknowledgements
This study was supported, in part, by a grant from the Centro SOL at the Johns Hopkins University School of Medicine and a training grant from the National Institute of Nursing Research of the National Institutes of Health under award number 5T32NR012704-05. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Additional resources were provided by Center for Cardiovascular and Chronic Care at the Johns Hopkins University School of Nursing.
Appendix. Electronic database search strategy
1.) Pubmed
Simply enter all these in the search bar
(“Text Messaging”[Mesh] OR “text message”[All Fields] OR “text messages”[All Fields] OR “text messaging”[All Fields] OR “texts”[All Fields] OR “texted”[All Fields] OR “texting”[All Fields] OR (SMS[tiab] AND messag* [tiab]) OR “short message service”[All Fields] OR “short messaging service”[All Fields]) AND ((“hypertension”[MeSH Terms] OR “hypertension”[All Fields] OR “high blood pressure” [tw]) OR (“diabetes mellitus”[MeSH Terms] OR (“diabetes”[All Fields] AND “mellitus”[All Fields]) OR “diabetes mellitus”[All Fields]) OR (“cholesterol”[MeSH Terms] OR “cholesterol”[All Fields]) OR (“smoking”[MeSH Terms] OR “smoking”[All Fields] OR smoker [tw] OR smokers [tw]) OR (“diet”[MeSH Terms] OR “diet”[All Fields]) OR (“obesity”[MeSH Terms] OR “obesity”[All Fields]) OR (“motor activity”[MeSH Terms] OR “motor activity”[All Fields] OR (“physical”[All Fields] AND “activity”[All Fields]) OR “physical activity”[All Fields]) OR (“exercise”[MeSH Terms] OR “exercise”[All Fields]))
2.) CINAHL
Enter these search terms in the first search bar:
((MH “Text Messaging”) OR “text messaging” ) OR ( “text message” OR “text messages” OR “text messaging” OR “texts” OR “texted” OR “texting” OR (SMS AND messag*) OR “short message service” OR “short messaging service” )
select AND
Enter these search terms in the second search bar:
((MH “Hypertension”) OR “hypertension” OR “high blood pressure” OR (MH “Diabetes Mellitus+”) OR “diabetes” OR (MH “Physical Activity”) OR “physical activity” OR (MH “Smoking+”) OR “smoking” OR (MH “Cholesterol+”) OR “cholesterol” OR (MH “Diet+”) OR “diet” OR (MH “Obesity+”) OR “obesity” ) OR smoke*
3.) Embase
Simply enter all these in the search bar
(‘text messaging’/exp OR (text* NEAR/3 messag*):ab,ti OR (sms NEAR/3 messag*):ab,ti OR ‘short message service’ OR ‘short messaging service’ OR texts:ab,ti OR texting:ab,ti OR texted:ab,ti) AND (‘hypertension’/exp OR hypertension:ab,ti OR ‘high blood pressure':ab,ti OR ‘diabetes mellitus’/exp OR (diabetes NEAR/3 mellitus):ab,ti OR diabetes:ab,ti OR ‘cholesterol’/exp OR cholesterol:ab,ti OR ‘smoking’/exp OR smoking:ab,ti OR smoke*:ab,ti OR ‘physical activity’/exp OR ((physical OR motor) NEAR/3 activity):ab,ti OR ‘diet’/exp OR diet:ab,ti OR ‘obesity’/exp OR obesity:ab,ti)
4.) Cochrane Library
follow the link and run the search http://onlinelibrary.wiley.com/cochranelibrary/search/advanced/shared/searches/8099909565383080553
5.) Scopus
(TITLE-ABS-KEY((text* W/3 messag* OR “texted” OR “texting” OR (SMS W/4 messag*) OR “short message service” OR “short messaging service”))) AND (TITLE-ABS-KEY((hypertension OR “high blood pressure” OR “diabetes mellitus” OR (diabetes W/3 mellitus) OR cholesterol OR “smoking” OR smoker OR smokers OR diet OR obesity OR “motor activity” OR (physical W/3 activity) OR (text* W/3 messag* OR “texted” OR “texting” OR SMS W/4 messag* OR “short message service” OR “short messaging service”) AND (“hypertension” OR “high blood pressure”) OR “diabetes mellitus” OR “diabetes W/3 mellitus” OR “cholesterol” OR “smoking” OR “smoker” OR “smokers” OR “diet” OR “obesity” OR “motor activity” OR “physical W/3 activity” OR “physical activity” OR “exercise”)
6.) Psych INFO
| Search ID# |
Search Terms | Search Options | Last Run Via | Results |
|---|---|---|---|---|
| S4 | S1 AND S2 | Limiters - Publication Year: 1995- 2014 Search modes - Boolean/Phrase |
Interface - EBSCOhost Research Databases Search Screen - Advanced Search Database - PsycINFO |
173 |
| S3 | S1 AND S2 | Search modes - Boolean/Phrase | Interface - EBSCOhost Research Databases Search Screen - Advanced Search Database - PsycINFO |
173 |
| S2 | text* N3 messag* OR (sms N5 messag*) OR “short messaging service” OR ‘short message service” OR texting OR texted |
Search modes - Boolean/Phrase | Interface - EBSCOhost Research Databases Search Screen - Advanced Search Database - PsycINFO |
1,411 |
| S1 | ((((((DE “Hypertension” OR DE “Essential Hypertension”) AND (DE “Diabetes” OR DE “Diabetes Mellitus”)) OR (DE “Tobacco Smoking” OR DE “Passive Smoking”)) OR (DE “Cholesterol”)) AND (DE “Diets” OR DE “Obesity”)) OR (DE “Exercise” OR DE “Aerobic Exercise” OR DE “Weightlifting” OR DE “Yoga”)) OR (DE “Physical Activity” OR DE “Exercise”) OR smoker* OR smoking OR diet OR obesity OR hypertension OR “high blood pressure” OR diabetes OR exercise OR “physical activity” OR “motor activity” OR cholesterol |
Search modes - Boolean/Phrase | Interface - EBSCOhost Research Databases Search Screen - Advanced Search Database - PsycINFO |
167,486 |
References
- 1.Murphy SL, Xu JQ, Kochanek KD. Deaths: Final data for 2010. National vital statistics reports. no.4. Vol. 61. National Center for Health Statistics (US); Hyattsville (MD): 2013. [PubMed] [Google Scholar]
- 2.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization [Accessed January 10, 2016];Global Status Report on noncommunicable diseases. 2014 http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf?ua=1.
- 4.Fletcher BR, Hartmann-Boyce J, Hinton L, McManus RJ. The effect of self-monitoring of blood pressure on medication adherence and lifestyle factors: a systematic review and meta-analysis. Am J Hypertens. 2015 doi: 10.1093/ajh/hpv008. [DOI] [PubMed] [Google Scholar]
- 5.Smith A. [Accessed November 1, 2015];The Smartphone Difference. http://www.pewinternet.org/2015/04/01/us-smartphoneuse-in-2015/
- 6.Acker A. The short message service: standards, infrastructure and innovation. Telematics Inf. 2014;31(4):559–68. [Google Scholar]
- 7.World Health Organization . mHealth: New Horizons for Health through Mobile Technologies: Based on the Findings of the Second Global Survey on eHealth (Global Observatory for eHealth Series, Volume 3) World Health Organization; Geneva, Switzerland: [Accessed December 6, 2014]. 2011. http://www.who.int/goe/publications/goe_mhealth_web.pdf. [Google Scholar]
- 8.de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R. Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Db Syst Rev. 2012;12 doi: 10.1002/14651858.CD007459.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.International Telecommunication Union [Accessed June 3, 2015];Information and communication technologies (ICT) facts and figures – the world in 2015. http://www.itu.int/en/ITUD/Statistics/Documents/facts/ICTFactsFigures2015.pdf.
- 10.Duggan M. Cell phone activities. Pew Research Center; [Accessed April 10, 2015]. 2013. http://www.pewinternet.org/2013/09/19/cell-phone-activities-2013/ [Google Scholar]
- 11.Holtz B, Lauckner C. Diabetes Management via Mobile Phones: A Systematic Review. Telemedicine and e-health. 2012;18(3):175–184. doi: 10.1089/tmj.2011.0119. [DOI] [PubMed] [Google Scholar]
- 12.Hall AK, Cole-Lewis HH, Bernhardt JM. Mobile text messaging for health: a systematic review of reviews. Annu Rev Public Health. 2015;36:393–415. doi: 10.1146/annurev-publhealth-031914-122855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preffered Reporting Items for Systematic Reviews and Meta-analyses: The PRISMA statement. PLoS Med. 2009;6(7):e100097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gomez EJ, Hernando ME, Garcia A, Del Pozo F, Cermeno J, Corcoy R, et al. Telemedicine as a tool for intensive management of diabetes: the DIABTel experience. Comput Methods Prog Bio. 2002;69:163–177. doi: 10.1016/s0169-2607(02)00039-1. [DOI] [PubMed] [Google Scholar]
- 16.Fu R, Vandermeer BW, Shamliyan TA, et al. Methods Guide for Comparative Effectiveness Reviews. Agency for Healthcare Research and Quality; Rockville, MD: 2013. Handling Continuous Outcomes in Quantitative Synthesis. [PubMed] [Google Scholar]
- 17.Carrasco MP, Salvador CH, Sagredo PG, Márquez-Montes J, González de Mingo MA, Fragua JA, et al. Impact of patient-general practitioner short-messages-based interaction on the control of hypertension in a follow-up service for low-to-medium risk hypertensive patients: a randomized controlled trial. IEEE Eng Med Bio. 2008;12(6):780–91. doi: 10.1109/TITB.2008.926429. [DOI] [PubMed] [Google Scholar]
- 18.Márquez-Contreras E, de la Figuera von Wichmann M, Gil Guillén V, Ylla-Catalá A, Figueras M, Balaña M, et al. [Effectiveness of an intervention to provide information to patients with hypertension as short text messages and reminders sent to their mobile phone (HTA-Alert)] Aten Primaria. 2004;34(8):399–405. doi: 10.1016/S0212-6567(04)78922-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kiselev A, Gridnev VI, Shvartz VA, Posnenkova O, Dovgalevsky PY. Active ambulatory care management supported by short message services and mobile phone technology in patients with arterial hypertension. JASH. 2012;6(5):346–55. doi: 10.1016/j.jash.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 20.Lin PH, Wang Y, Levine E, Askew S, Lin S, Chang C, et al. A text messaging-assisted randomized lifestyle weight loss clinical trial among overweight adults in Beijing. Obesity (Silver Spring) 2014;22(5):E29–37. doi: 10.1002/oby.20686. [DOI] [PubMed] [Google Scholar]
- 21.Park MJ, Kim HS. Evaluation of mobile phone and Internet intervention on waist circumference and blood pressure in post-menopausal women with abdominal obesity. Int J Med Inform. 2012;81(6):388–94. doi: 10.1016/j.ijmedinf.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 22.Palileo-Villanueva L. ClinicalTrials.gov [Internet] National Library of Medicine (US); Bethesda (MD): [cited 2014 Dec 22]. 2011. Effectiveness of SMS text reminders to improve blood pressure among patients with hypertension. Available from: https://clinicaltrials.gov/ct2/show/NCT01255436 NLM Identifier: NCT01255436. [Google Scholar]
- 23.Jolles EP, Clark AM, Braam B. Getting the message across: opportunities and obstacles in effective communication in hypertension care. J Hypertens. 2012;30(8):1500–10. doi: 10.1097/HJH.0b013e32835476e1. [DOI] [PubMed] [Google Scholar]
- 24.Noar S, Harrington N, Van Stee S, Aldrich R. Tailored Health Communication to Change Lifestyle Behaviors. Am J Lifestyle Med. 2010;5(2):112–122. doi: 10.1177/1559827610387255. [DOI] [Google Scholar]
- 25.Turner-Lee N, Smedley BD, Miller J. Minorities, mobile broadband and the management of chronic diseases. Joint Center for Political and Economic Studies; Washington DC: 2012. [Google Scholar]