Figure 4. Diagrams illustrating the acute and chronic effects of EO on Ca2+ homeostasis in the heart: roles of α2 Na+ pumps (NKA), NCX1, SERCA2 and ryanodine receptors (RyR) .
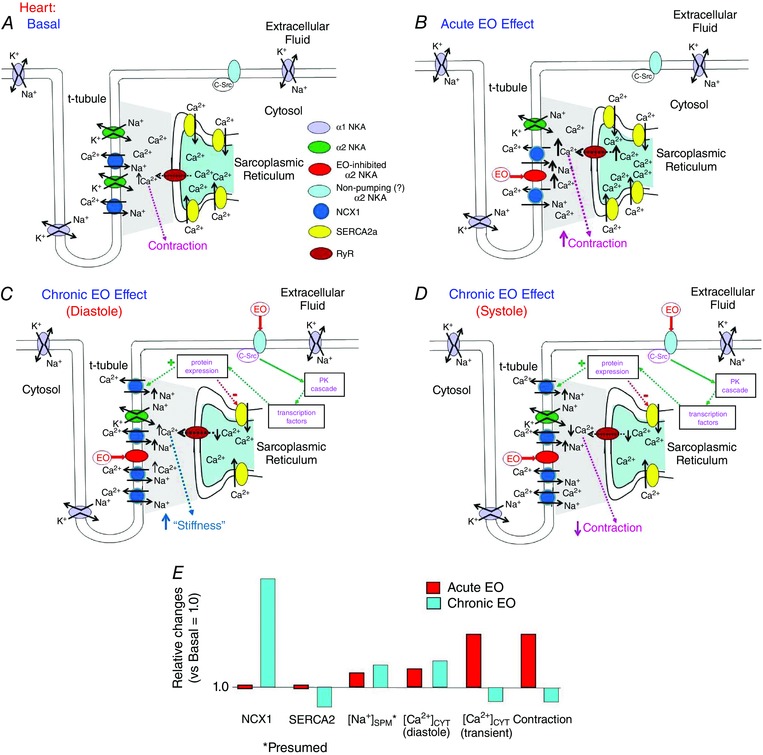
A, basal conditions. In cardiac myocytes, during the major part of the cardiac cycle the NCX1 operates in the Ca2+ exit mode because the diastolic V m, perhaps about −65 to −75 mV, is more negative than E Na/Ca; i.e. the driving force (V m − E Na/Ca) is negative. B, acute exposure of the heart to low dose ouabain or EO inhibits cardiac myocyte α2 Na+ pumps and raises [Na+]SPM. This increases E Na/Ca, but reduces the driving force for Ca2+ extrusion and elevates [Ca2+]SPM. Thus, the net effect, as in arteries, is enhanced Ca2+ signalling and contraction (i.e. the cardiotonic effect). C and D, sustained exposure of cardiac myocytes to low dose ouabain or EO also, as in arteries, activates an α2 Na+ pump‐mediated protein kinase (PK) signalling cascade. In the heart, however, this leads to increased NCX1 expression, but decreased SERCA expression (green and red dotted lines and ‘+’ and ‘−’, respectively). Thus, initially, the cytosolic and SR [Ca2+] are elevated, the cardiotonic effect prevails, increased cardiac contraction is sustained (as in ‘B’), and the heart may hypertrophy from the increased workload. Eventually, however, the sustained Na+ pump inhibition and [Na+]CYT/[Na+]SPM elevation will maintain an elevated diastolic [Ca2+]CYT (C) despite the up‐regulated NCX1. The decreased SERCA2 expression and leakage of Ca2+ from the SR via RyR, however, reduces SR Ca2+ sequestration and [Ca2+]CYT transients (D); thus, cardiac contraction decreases, and the heart fails. E, summary of the acute and chronic EO‐induced approximate relative changes in NCX1 and SERCA2 expression, [Na+]SPM (postulated; see Fig. 3 legend), [Ca2+]CYT and contraction. Note that the acute vasotonic (Fig. 3 B and D) and cardiotonic effects of EO are similar, whereas the chronic effects of EO in the heart (C–E) differ greatly from those in arteries (Fig. 3 C, D).
