Abstract
Background. Despite the increased burden of mental health problem, little is known about knowledge and perception of the public towards mental health problems in Ethiopia. Methods. Community based cross-sectional study was conducted among selected 845 Gimbi town residents from May 28 to June 28, 2014. Results. Out of the total study participants, 304 (37.3%) were found to have poor perception (a score below mean five semantic differential scales for positive questions and above mean for negative questions) of mental illness. Being above 28 years of age (AOR = 0.48 CI (0.23, 0.78)), private workers (AOR = 0.41 CI (0.19, 0.87)), and lack of mental health information were found to be associated with poor perception of mental illness (AOR = 0.133 CI (0.09, 0.20)). Absence of family history of mental illness was also found to be associated with poor perception of mental illness (AOR = 0.37 CI (0.21, 0.66)). Conclusions. Significant proportions of the community in Gimbi town were found to have poor perception of mental illness. Poor perception is common among old aged, less educated, private workers, those unable to access mental health information, and those with no family history of mental illness. Mental health education on possible causes, treatment options, and possible outcome of treatment to the community is required.
1. Background
Mental and behavioral problem exist in all countries, in women and men at all stages of life, among the poor and rich and among rural and urban people. As many as 450 million people worldwide are estimated to be suffering at any given time from some kind of mental or brain disorder, including behavioral and substance related disorders [1]. Worldwide it is estimated that life time prevalence ranges from 12.2% to 48.6% and 12-month prevalence between 8.25% and 29.1% [2].
Community's perception of mental health varies across the culture, and there are various myths and beliefs regarding mental health [3]. The conceptualization and perceived cause of mental illness vary from community to community. Accordingly, people with mental health problem get different names in different societies [4–6].
People tend to have strong beliefs about the mental illness, and many of these concepts are based on prevailing local systems of belief. Most of the society's perception and attitude towards mental illness are far from the scientific view and this may negatively affect treatment seeking and adherence [7, 8].
Several studies show that people's belief regarding mental illness is also the main factor which leads to stigmatization and labeling. Stigma against people with mental illness remains a significant barrier to positive outcomes across cultures and nations, related to the threat value of mental symptoms, intolerance for diversity, and inaccurate conceptions of mental disorder [9, 10].
Community's perception is dynamic and tends to change as the awareness and education changes. Education and social media are the major factors which move the perception of the community to the scientific perspectives [11].
Globally, including developed and developing countries, people held different explanation regarding mental illness, especially its causal and treatment option. A report of the behavioral risk factor surveillance system shows that in USA 80% of the adult population in the state surveyed agree that mental illness treatment is effective. The rest either disagree or have no idea about that and only 35%–67% of the population agreed that people are caring and sympathetic to people with mental illness [12].
Mental health, neglected for far too long, is crucial to the overall well-being of individuals, societies, and countries and must be universally regarded in a new light. Unfortunately, in most parts of the world, mental health and mental disorders are not regarded with anything like the same importance as physical health [13].
Poor perception of mental illness in different community contributed to low treatment seeking and stigmatization of people with mental illness. They often go to hospitals after they have tried all options and after the symptom has got worse and this in turn negatively affects the prognoses of treatment [14].
Hence, assessing community's perception is important to have appropriate plan of health promotion and scaling up publics' utilization of mental health services, particularly in multiethnic and multicultural Ethiopia as the community's view of mental illness varies with culture.
Studies done in different areas have shown that poor perception towards the mentally ill is mainly deep rooted with various sociodemographic and other factors [7, 8, 10, 13–18].
In Ethiopia there are few published studies [18] assessing community perception towards people with mental illness and no studies were done in Gimbi town concerning this topic. Therefore, this study has great value on assessing the perception of the community towards mental illness. Also the result of this study is very important to the mental health strategy developed so far and to other stakeholders as describing the community's deep rooted belief and perception regarding mental illness in West Wellega, particularly Gimbi town.
2. Method and Materials
2.1. Study Design and Period
Community based cross-sectional study design was conducted from May 28 to June 28, 2014, at Gimbi town, West Wellega Zone of Oromia region, Ethiopia. The town is located at a distance of 441 Km from the capital city, Addis Ababa to the west. Gimbi town has got two hospitals and one health center. The town has 4 kebeles and according to the 2007 National Housing and Population Census, the projected population of Gimbi town for the year 2014/15 was about 42,286 and the estimated number of households was 8629 [19].
2.2. Sampling Techniques
Single population proportion with the assumptions of 95% level of confidence, 5% error, and 50% proportion was used to estimate the minimum sample size for the study. Considering the design effect of two (multiplied by 2) and 10% nonresponse rate, the final sample size became 845.
Following purposive selection of the administrative town (Gimbi town), the two kebeles out of four (the smallest administrative level) were selected randomly. Households in the selected kebeles were approached by systematic sampling method with the first household selected randomly. From each selected household, one individual, 18 years of age and older (based on information from household head), was included for the interview. A lottery method was used to select one individual in a house hold where more than one individual, 18 years of age and older, was found.
2.3. Data Collection and Measurements
Data were collected through face to face interview by trained data collectors. A case vignette based standardized questionnaire which explains cases like schizophrenia, major depressive disorder, epilepsy, and generalized anxiety disorder [18] as well as questionnaires adopted from previous studies to assess sociodemographic characteristics and other associated factors was used. Standard 9 items of five semantic deferential scales were also used to assess community perception about mental illness. A score above mean score of five semantic differential scales for positive questions and below mean score for negative questions was considered as having good perception of mental illness. Four trained diploma nurses interviewed the community and were supervised in the field during data collection. Eligible participants not available at home during the first visit of data collection were revisited once on the next day and then registered as nonresponse if not found.
2.4. Data Quality Control
The tool was first developed in English language and translated to Amharic language with back translation to English for consistency. Amharic version questionnaire was used to collect data as Amharic is the national official language that majority of Ethiopians speak.
To assure the quality of data the questionnaire was pretested 1 week before the actual data collection time among 40 people not included in the actual sample and appropriate modification was made. The reliability of the tool was found to be α = 0.73.
Training on objectives of the study, over all data collection procedure and ethics of the study, was given to data collectors and supervised by principal investigators on the actual data collection site. To ensure confidentiality, interview was conducted in private setting. Throughout the course of the data collection, interviewers were supervised at each site; regular meetings were held between the data collectors and the principal investigator. Two more additional visits were made for eligible respondent not accessed in the first visit. The collected data was reviewed and checked for completeness before data entry.
2.5. Data Processing and Analysis
Data clean-up and cross checking were done before analysis. Checked, cleaned, and coded data was entered into EPI info version 7 and exported to SPSS version 20.0 for analysis. Descriptive statistics like frequencies, percentages, mean, and standard deviation were used to present data. Tables and figures were also used to present data. Binary logistic regression was used to see associated factors with the dependent variable. Those variable with p value less than 0.02 were entered to multivariate analysis to identify the independent associated factors after confounders are controlled. Finally the variables which had independent association with community perception were identified on the basis of OR, with 95% CI and p value less than 0.05.
2.6. Ethical Considerations
Ethical clearance was obtained from the Institutional Review Board of University of Gondar and Amanuel mental specialized hospital. Permission letter was obtained from Oromia regional health bureau, West Wellega Zonal health department, and Gimbi town health office hierarchically.
Written informed consent was obtained from each study participant. After reading the consent statement by the data collectors, finger prints were obtained from those participants who could not read and write. The respondents were informed that their inclusion in the study is voluntary and they are free to withdraw from the study if they are not willing to participate.
Also all respondents are informed that they did not have direct payment for their participation in the study. Anonymity was maintained to ensure confidentiality of respondents.
3. Results
A total of 845 selected peoples in Gimbi town were interviewed, out of which 29 responses were excluded for gross incompleteness and considered as nonresponse. Therefore, analysis was made based on 816 questionnaires, yielding a response rate of 96.5%.
3.1. Sociodemographic Characteristics of Respondents
Among the total respondents, 414 (50.73%) were females and the mean age of participants was 33.0 ± 10 SD. The majority, 706 (86.5%), of study participants were Oromo in ethnicity and four hundred and sixty-seven (57.2%) were Orthodox followers by religion. 577 (70.7%) were married, 285 (34.9%) have elementary level education, and 31.4% of the respondents were merchant. Six hundred and fifteen (75.4%) of the respondents had an average family monthly income less than or equal to 651 Ethiopian birr (Table 1).
Table 1.
Sociodemographic characteristics of respondents (n = 816) in Gimbi town, West Wellega Zone, Oromia region, Ethiopia, 2014.
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Age | 18–28 | 313 | 38.4 |
| 29–38 | 301 | 36.9 | |
| ≥39 | 202 | 24.8 | |
|
| |||
| Sex | Male | 402 | 49.3 |
| Female | 414 | 50.7 | |
|
| |||
| Religion | Orthodox | 467 | 57.2 |
| Protestant | 266 | 32.6 | |
| Muslim | 83 | 10.2 | |
|
| |||
| Ethnicity | Oromo | 704 | 86.3 |
| Amhara | 84 | 10.1 | |
| Gurage | 18 | 2.2 | |
| Tigre | 8 | 1.2 | |
| Others | 2 | 0.2 | |
|
| |||
| Educational status | Degree and above | 38 | 4.7 |
| Diploma | 119 | 14.6 | |
| High school | 280 | 34.3 | |
| Elementary | 285 | 34.9 | |
| Uneducated | 94 | 11.5 | |
|
| |||
| Marital status | Single | 221 | 27.1 |
| Married | 577 | 70.7 | |
| Divorced | 18 | 2.2 | |
|
| |||
| Occupational status | Government | 113 | 13.8 |
| Private | 270 | 33.1 | |
| Merchant | 256 | 31.4 | |
| Student | 66 | 8.1 | |
| Housewife | 111 | 13.6 | |
|
| |||
| Family monthly income in Ethiopian birr | ≤450 | 27 | 25.4 |
| 451–650 | 215 | 26.3 | |
| 651–1300 | 193 | 23.7 | |
| ≥1301 | 201 | 24.6 | |
3.2. Mental Health Information
Mental health information refers to information on the types of mental illness, causes, possibility of treatment, treatment options, and magnitude of mental illness. Accordingly, among all study participants, 564 (69.1%) were reported as having mental health information in the past 12 months while the remaining 252 did not receive any information related to mental health illness. Among 564 respondents having information regarding mental illness 21.3%, 12.4%, and 11% believe that mental illnesses are caused by excessive worry, substance use, and evil spirit, respectively. Mental illness are serious problem (18.5%) and stress can cause mental illness (11.3%), which were among the statements frequently mentioned.
3.3. Family History of Mental Illness
Presence of family member/s with any type of mental health problem was considered here. Among the total participants, 100 (12.3%) were reported to have family history of mental illness (Figure 1).
Figure 1.
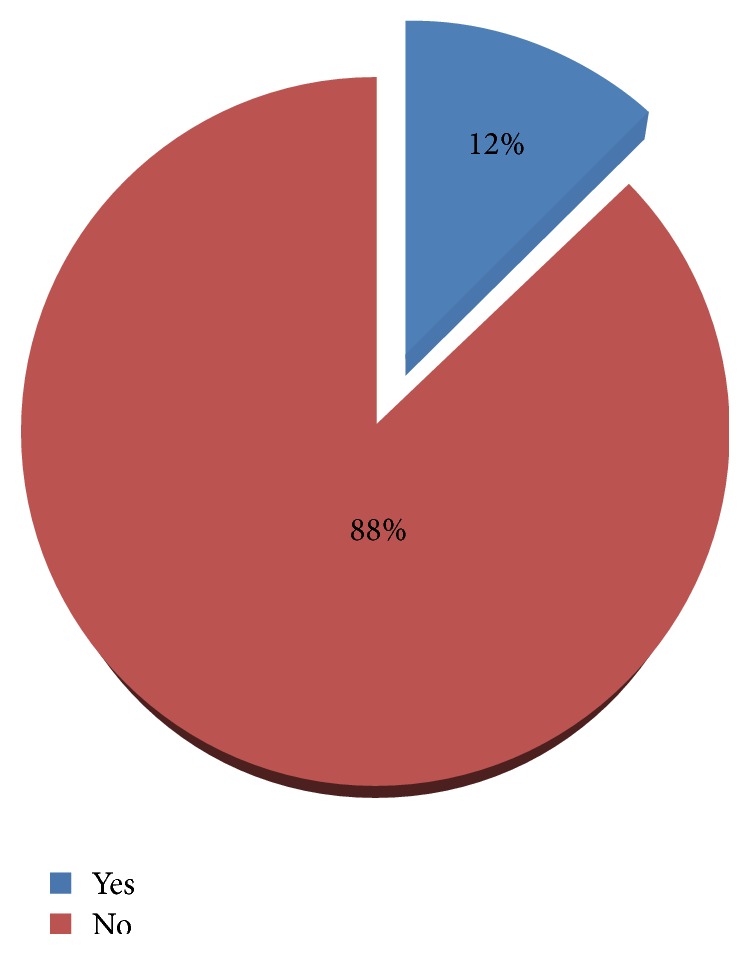
Distribution of family history of mental illness among residents of Gimbi town, 2014.
3.4. Respondents' Perception of Mental Illness
A score below 27 for 9 items of five semantic deferential scales was considered having poor perception towards mental illness in this study. Accordingly (37.3%) respondents were found having poor perception towards mental illness (Table 2).
Table 2.
Distribution of community's perception of mental illness among the residents of Gimbi town, Oromia region, Ethiopia (n = 816), 2014.
| S. number | Questions | 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | ||
| 1 | Do you agree that substance misuse like alcohol or drug could result in mental illness? | 12 | 1.5 | 50 | 6.5 | 106 | 13.0 | 444 | 55.4 | 204 | 25.0 |
| 2 | Do you agree that genetic inheritance could be the cause of mental illness? | 220 | 27.0 | 130 | 15.9 | 150 | 18.4 | 222 | 27.2 | 94 | 11.5 |
| 3 | Do you agree that head injury can be the cause of mental illness? | 52 | 6.4 | 130 | 15.9 | 111 | 13.6 | 308 | 37.7 | 215 | 26.3 |
| 4 | Do you agree that physical illness (like diabetes, HIV/AIDS) can be the cause of mental illness | 54 | 6.6 | 221 | 27.1 | 49 | 6.0 | 273 | 33.5 | 219 | 26.8 |
| 5 | Do you agree that mental illness is treatable? | 12 | 1.5 | 220 | 27.0 | 60 | 7.4 | 304 | 37.3 | 220 | 27.0 |
| 6 | Do you agree that stress in daily life can cause mental Illness? | 19 | 2.3 | 107 | 24.1 | 65 | 8.0 | 270 | 33.1 | 265 | 32.5 |
| 7 | Do you agree that mental illness is contagious? | 435 | 53.3 | 152 | 18.6 | 171 | 21 | 40 | 4.9 | 18 | 2.2 |
| 8 | Do you agree that mental illness is punishment from God? | 38 | 4.7 | 88 | 10.8 | 400 | 49.0 | 226 | 27.7 | 64 | 7.8 |
| 9 | Do you agree that evil sprite can be the cause of mental illness? | 32 | 3.9 | 35 | 4.3 | 221 | 27.0 | 413 | 50.6 | 115 | 14.0 |
1: strongly disagree; 2: disagree; 3: not sure; 4: agree; 5: strongly agree.
3.5. Respondents' Perceived Cause of Mental Illness
Majority of the respondents attributed the cause of mental illness in the case vignette to supernatural causes like evil spirit, God's punishment, and witchcraft. Table 3 shows the distribution of perceived cause of mental illness in the case vignettes (Table 3).
Table 3.
Distribution of respondents' perceived cause of mental illness among residents of Gimbi town, West Wellega Zone, Oromia region, Ethiopia (multiple responses), 2014.
| Causes | Mental illness | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Epilepsy | Schizophrenia | MDD | GAD | ||||||
| N | % | N | % | N | % | N | % | ||
| Evil spirit | No | 262 | 32.1 | 232 | 28.4 | 280 | 34.3 | 334 | 40.9 |
| Yes | 554 | 67.9 | 584 | 71.6 | 536 | 65.7 | 482 | 59.1 | |
| God's punishment | No | 644 | 78.9 | 646 | 79.2 | 706 | 86.5 | 732 | 89.7 |
| Yes | 172 | 21.1 | 170 | 20.8 | 110 | 13.5 | 84 | 10.3 | |
| Witchcraft | No | 648 | 79.4 | 640 | 78.4 | 668 | 81.9 | 684 | 83.8 |
| Yes | 168 | 20.6 | 176 | 21.6 | 148 | 18.1 | 132 | 16.2 | |
| Daily stress | No | 596 | 73.0 | 254 | 31.1 | 774 | 94.9 | 202 | 24.8 |
| Yes | 220 | 27.0 | 562 | 68.9 | 42 | 5.1 | 614 | 75.2 | |
| Biological | No | 736 | 90.2 | 710 | 87.0 | 204 | 25.0 | 185 | 22.7 |
| Yes | 80 | 9.8 | 106 | 13.0 | 612 | 75.0 | 631 | 77.3 | |
| Substance use | No | 630 | 77.2 | 394 | 48.3 | 632 | 77.5 | 696 | 85.3 |
| Yes | 186 | 22.8 | 422 | 51.7 | 184 | 22.5 | 120 | 14.7 | |
| Physical illness | No | 488 | 59.8 | 664 | 81.4 | 632 | 77.5 | 756 | 92.6 |
| Yes | 328 | 40.2 | 152 | 18.6 | 184 | 22.5 | 60 | 7.4 | |
3.6. Respondents' Recognition of the Case Vignette as Mental Illness
Schizophrenia was the case identified as mental illness by the majority of respondents. Seven hundred and seventy-four (94.9%) of the respondents identified schizophrenia as mental illness. General Anxiety Disorder (GAD) was the least case identified as mental illness by the respondents (Figure 2).
Figure 2.
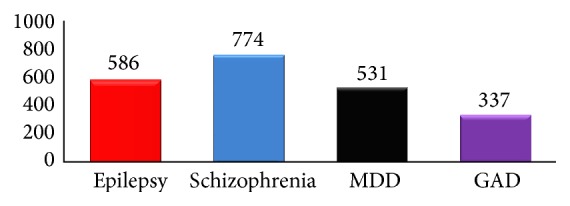
Distribution of respondents' recognition of mental illness among residents of Gimbi town, 2014.
3.7. Perception regarding Possibility of Treatment of Mental Illness on the Case Vignette
Great discrepancy was observed among case vignettes regarding the respondents' view of whether or not they can be treated. Majority of the respondents (784) (96.1%), reported that GAD can be treated while 202 (24.8%) of the respondents reported that schizophrenia is treatable (Figure 3).
Figure 3.
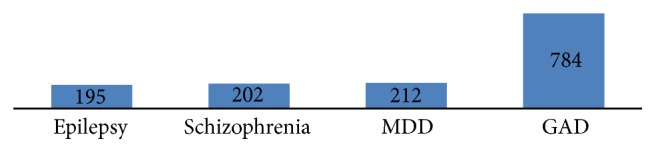
Distribution of respondents' perception regarding possibility of treatment of mental illness (n = 816), Gimbi town, 2014.
3.8. Respondents Preferred Place of Treatment for the Case Vignettes
Regarding preferred place of treatment: 538 (65.9%), 470 (57.6%), 454 (55.6%), and 254 (31.1%) of respondents prefer health institution for epilepsy, schizophrenia, MDD, and GAD, respectively. See Table 4 for the distribution of the respondents' preferred place of treatment.
Table 4.
Distribution of respondents preferred place of treatment mental illness among residents of Gimbi town, West Wellega Zone, Ethiopia, 2014.
| Treatment option | Mental illness | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Epilepsy | Schizophrenia | MDD | GAD | ||||||
| N | % | N | % | N | % | N | % | ||
| Family | No | 808 | 99.0 | 810 | 99.3 | 784 | 96.1 | 612 | 75.0 |
| Yes | 8 | 1.0 | 6 | .7 | 32 | 3.9 | 204 | 25.0 | |
| Hospital/HC | No | 278 | 34.1 | 346 | 42.4 | 362 | 44.4 | 562 | 68.9 |
| Yes | 538 | 65.9 | 470 | 57.6 | 454 | 55.6 | 254 | 31.1 | |
| Holly water | No | 658 | 80.6 | 656 | 80.4 | 658 | 80.6 | 728 | 89.2 |
| Yes | 158 | 19.4 | 160 | 19.6 | 158 | 19.4 | 88 | 10.8 | |
| Traditional healer | No | 772 | 94.6 | 770 | 94.4 | 758 | 92.9 | 796 | 97.5 |
| Yes | 44 | 5.4 | 46 | 5.6 | 58 | 7.1 | 20 | 2.5 | |
| Prayer | No | 572 | 70.1 | 538 | 65.9 | 380 | 46.6 | 334 | 40.9 |
| Yes | 244 | 29.9 | 278 | 34.1 | 436 | 53.4 | 482 | 59.1 | |
| Witchcraft | No | 782 | 95.8 | 790 | 96.8 | 790 | 96.8 | 804 | 98.5 |
| Yes | 34 | 4.2 | 26 | 3.2 | 26 | 3.2 | 12 | 1.5 | |
3.9. Respondents Perceived Severity of Mental Illness
Respondents were asked to rank the case vignette from the most serious to the least. Schizophrenia was seen as the most severe by majority of the respondents. Following schizophrenia, epilepsy, major depressive disorder, and generalized anxiety disorder were seen from the most severe to the least, respectively (Figure 4).
Figure 4.
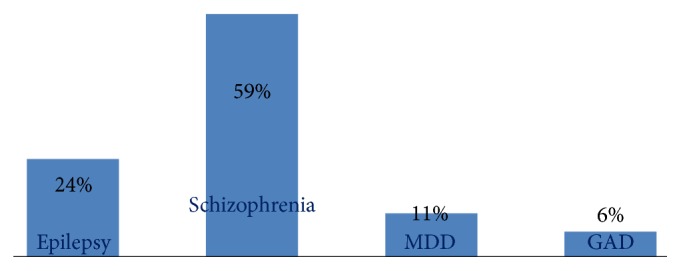
Distribution of respondents' perceived severity of mental illness among residents of Gimbi town, West Wellega Zone, Oromia region, Ethiopia, 2014 (n = 816).
3.10. Factors Associated with the Respondents' Perception of Mental Illness
In bivariate analyses age of respondents, educational status, occupational status, mental health information, and family history of mental illness were found to be significantly associated with perception of mental illness.
Respondent age, educational level, occupation, mental health information, and family history of mental illness were found to be independently associated after multivariate analysis.
The likelihood of having poor perception of mental illness among those above age 39 is higher than those below 28 years old (AOR = 0.5 (0.30, 0.80)). The proportion of poor perception is observed among those who have no formal education (AOR = 0.09 CI (0.02, 0.46)), elementary education (AOR = 0.07 CI (0.02, 0.33)), and high school level (AOR = 0.13 CI (0.03, 0.61)), when compared with those with degree and above. This shows that perception towards mental illness is higher among educated people.
Community's perceptions of mental illness were also found associated with occupational status. Private workers will have poor perception when compared with government employees (AOR = 0.41 CI (0.09, 0.87)). Mental health information is also associated with perception of mental illness. Having mental health information from any sources is more likely associated with good perception of mental illness (AOR = 0.133 CI (0.09, 0.2)).
The likelihood of having good perception among individual with no family history of mental illness is 63% less when compared with those having family history of mental illness (AOR = 0.37 CI (0.21, 0.66)) (Table 5).
Table 5.
Distribution of factors associated with community's perception of mental illness among residents of Gimbi town, West Wellega Zone, Oromia region, Ethiopia, 2014.
| Variable | Perception | Crud OR 95% CI | Adjusted OR | |
|---|---|---|---|---|
| Good (%) | Poor (%) | |||
| Age | ||||
| 18–28 | 215 (68.7) | 98 (31.3) | 1.00 | 1.00 |
| 29–38 | 210 (69.8) | 91 (30.2) | 1.05 (0.7, 1.5) | 1.2 (0.8, 1.9) |
| ≥39 | 87 (43.1) | 115 (56.9) | 0.35 (0.24, 0.50) | 0.5 (0.30, 0.80)∗ |
| Education | ||||
| Illiterate | 40 (42.6) | 54 (57.4) | 0.41 (0.01, 0.18) | 0.09 (0.02, 0.46)∗ |
| Elementary | 138 (48.4) | 147 (51.6) | 0.05 (0.01, 0.22) | 0.07 (0.02, 0.33)∗ |
| High school | 187 (66.8) | 93 (33.2) | 0.11 (0.03, 0.47) | 0.13 (0.03, 0.61)∗ |
| Diploma | 118 (93.3) | 8 (6.7) | 0.77 (0.16, 3.80) | 1.35 (0.25, 7.24) |
| Degree & above | 36 (94.7) | 2 (5.3) | 1.00 | 1.00 |
| Occupation | ||||
| Government | 100 (88.5) | 13 (11.5) | 1.00 | RC |
| Private | 121 (44.8) | 149 (55.2) | 0.11 (0.06, 0.20) | 0.41 (0.19, 0.87)∗ |
| Merchant | 188 (73.4) | 68 (26.6) | 0.36 (0.19, 0.68) | 1.25 (0.60, 2.69) |
| Student | 42 (63.6) | 24 (36.4) | 0.23 (0.11, 0.49) | 0.62 (0.25, 1.56) |
| Housewife | 61 (55.0) | 50 (45.0) | 0.16 (0.08, 0.32) | 0.84 (.36, 1.96) |
| Mental health information | Yes 423 (75.0) | 141 (25.0) | 1.00 | RC |
| No 89 (35.3) | 161 (64.7) | 0.18 (0.13, 0.25) | 0.133 (0.09, 0.2)∗ | |
| Family history of mental illness | Yes 74 (74.0) | 26 (26.0) | 1.00 | RC |
| No 438 (61.2) | 278 (38.8) | 0.14 (0.35, 0.89) | 0.37 (0.21, 0.66)∗ | |
∗ p value < 0.05; RC: reference category.
4. Discussion
This community based cross-sectional study identified important information on community perception towards mental illness. Significant number of the respondents from Gimbi community had poor perception of mental illness. This study is in line with the study conducted in India where 39.4% of the respondents were found to have poor perception about mental illness [14]. But it is not consistent with study done in Iraq where 30% of the respondents were with poor perception of mental illness [13]. The variation might be due to socioeconomic and cultural difference among respondents.
This study demonstrated that there was higher proportion of poor perception of mental illness among those above 39 years of age compared to the youth. The finding is not consistent with a study done in North Western Ethiopia, Agaro town, where younger respondents were more likely to hold socioenvironmental deprivation responsible for mental and physical illnesses than older respondents [18]. This could be due to the difference in educational level between these two groups or may be due to the fact that the younger respondents may have access to information. Also in study done in Iraq and India no significant association was found with age regarding the community's view of mental illness. This could be due to the tool used or sample characteristics as rural and urban community are involved in both studies [13, 14].
Educational level was found to be one of the sociodemographic characteristics significantly affecting perception of mental illness in this study. Respondents who have no formal education are by 90% more likely to have poor perception when compared with degree holders and above. This finding is in agreement with the study done in Agaro town [18]. Study done in Nigeria also found out that perception of mental illness correlates with educational level [20]. Less educated respondents were more likely to attribute mental illnesses to supernatural retribution. This could be due to poor understanding of scientific explanation regarding causation of mental illness.
Occupational status was significantly associated with perception of mental illness. Government employees will have good perception of mental illness compared to private workers, which implies those in government organization may have more access to current policies, directions, and strategies relatively than those in private organizations. However this finding is not clearly observed in other studies. This may be due to the difference of tool used.
In addition, respondents having information about mental illness from any source were of good perception of mental illness compared to those having no information. This finding is in line with the study done in Karfi region of Nigeria [15]. Theory of psychology also supports this fact. According to psychologists' point of view, perception can be deductive or inductive. If perception is deductive, no probabilistic association needs to be added and no cognition is required. Information is sufficient and deductive perception is possible. If however perception is inductive some premises come from cognition and memory [21].
Family history of mental illness is also another factor found associated with perception of mental illness among Gimbi community. Those who do not have family history of mental illness are found more likely to have poor perception of mental illness than those having family history of mental illness. This may be due to the fact that those having family history of mental illness may share experience. This experience may help them to develop good perception. This factor is also supported by psychologists' explanation. According to Bill, perceptual experiences are experiences of mind-independent things and are themselves an account of the way in which they provide peculiarly basic reasons for beliefs about the world around the perceiver [22].
4.1. Conclusion and Recommendation
Significant proportions of community in Gimbi town have poor perception of mental illness. Poor perception of mental illness was common among old age people, those with low educational level, private workers, those who do not have mental health information, and those who do not have family history of mental illness. High level of educational status and access to mental health information strengthen the community's perception of mental illness.
It is important to address the poor perception towards the mentally ill in order to make community based mental health care a reality. The community health professionals should work on awareness creation on mental ill issues at the community level providing relevant information. There is the need to provide more knowledge and increased awareness on the causes of mental illness and also dispel the myths around the causes of the disorders and treatment options.
Acknowledgments
The authors would like to thank Amanuel Mental Specialized Hospital for financial support and providing necessary materials in support of undertaking this research. They would also like to appreciate Gimbi Town Health Office, supervisors, and data collectors who showed the greatest effort in acquiring appropriate information. Finally, they would like to acknowledge the study subjects who have kindly cooperated in providing the required information.
Competing Interests
The authors declare they have no conflict of interests.
Authors' Contributions
Jemal Ebrahim, Misael Benti, Tadesse Awoke, and Zegeye Yohannis designed the study, collected data, and participated in data analysis and interpretation. Jemal Ebrahim and Asres Bedaso prepared the manuscript. All the authors saw and approved the final version of the manuscript.
References
- 1.WHO. Stigmatization and Human Rights Violations Mental Health a Call for Action by World Health Ministers. 2001. [Google Scholar]
- 2.WHO. Scaling Up Care for Mental, Neurological and Substance Use Problem. 2008. (Mental Health Gap Action Program). [PubMed] [Google Scholar]
- 3.Saint Arnault D. Cultural determinants of help seeking: a model for research and practice. Research and Theory for Nursing Practice. 2009;23(4):259–278. doi: 10.1891/1541-6577.23.4.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Teferra S., Shibre T. Perceived causes of severe mental disturbance and preferred interventions by the Borana semi-nomadic population in southern Ethiopia: a qualitative study. BMC Psychiatry. 2012;12, article 79 doi: 10.1186/1471-244x-12-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stolovy T., Levy Y. M., Doron A., Melamed Y. Culturally sensitive mental health care: a study of contemporary psychiatric treatment for ultra-orthodox Jews in Israel. International Journal of Social Psychiatry. 2013;59(8):819–823. doi: 10.1177/0020764012461206. [DOI] [PubMed] [Google Scholar]
- 6.Payne J. S. Influence of race and symptom expression on clinicians’ depressive disorder identification in African American men. Journal of the Society for Social Work and Research. 2012;3(3):162–177. doi: 10.5243/jsswr.2012.11. [DOI] [Google Scholar]
- 7.Nsereko J. R., Kizza D., Kigozi F., et al. Stakeholder's perceptions of help-seeking behaviour among people with mental health problems in Uganda. International Journal of Mental Health Systems. 2011;5, article 5 doi: 10.1186/1752-4458-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ventevogel P., Jordans M., Reis R., De Jong J. Madness or sadness? Local concepts of mental illness in four conflict-affected African communities. Conflict and Health. 2013;7, article 3 doi: 10.1186/1752-1505-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stier A., Hinshaw S. P. Explicit and implicit stigma against individuals with mental illness. Australian Psychologist. 2007;42(2):106–117. doi: 10.1080/00050060701280599. [DOI] [Google Scholar]
- 10.Gureje O., Lasebikan V. O., Ephraim-Oluwanuga O., Olley B. O., Kola L. Community study of knowledge of and attitude to mental illness in Nigeria. British Journal of Psychiatry. 2005;186:436–441. doi: 10.1192/bjp.186.5.436. [DOI] [PubMed] [Google Scholar]
- 11.Pescosolido B. A., Martin J. K., Link B. G., et al. Americans' views of mental health and illness at century's end: continuity and change. Public Report on the MacArthur Mental Health Module, General social survey. Indian Consortium for Mental Health Services Research, 1996.
- 12.BRFSS. BRFSS Mental Illness Stigma Report. Atlanta, Ga, USA: Behavioral Risk Factor Surveillance System; 2012. Attitude toward mental illness. [Google Scholar]
- 13.Sadik S., Bradley M., Al-Hasoon S., Jenkins R. Public perception of mental health in Iraq. International Journal of Mental Health Systems. 2010;4, article 26 doi: 10.1186/1752-4458-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salve H., Goswami K., Sagar R., Nongkynrih B., Sreenivas V. Perception and attitude towards mental illness in an urban community in South Delhi—a community based study. Indian Journal of Psychological Medicine. 2013;35(2):154–158. doi: 10.4103/0253-7176.116244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kabir M., Iliyasu Z., Abubakar I. S., Aliyu M. H. Perception and beliefs about mental illness among adults in Karfi village, northern Nigeria. BMC International Health and Human Rights. 2004;4, article 3 doi: 10.1186/1472-698x-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crabb J., Stewart R. C., Kokota D., Masson N., Chabunya S., Krishnadas R. Attitudes towards mental illness in Malawi: a cross-sectional survey. BMC Public Health. 2012;12(1, article 541) doi: 10.1186/1471-2458-12-541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Girma E., Tesfaye M., Froeschl G., Möller-Leimkühler A. M., Müller N., Dehning S. Public stigma against people with mental illness in the Gilgel Gibe Field Research Center (GGFRC) in Southwest Ethiopia. PLoS ONE. 2013;8(12) doi: 10.1371/journal.pone.0082116.e82116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deribew Y. S. T. How are mental health problems perceived by a community in Agaro town? Ethiopian Journal of Health Development. 2005;9(2):153–159. [Google Scholar]
- 19.CSA (Central Statistical Agency) The 2007 Population and Housing Census of Ethiopia. Statistical Report. Addis Ababa, Ethiopia: CSA; 2008. [Google Scholar]
- 20.Adewuya A. O., Makanjuola R. O. A. Lay beliefs regarding causes of mental illness in Nigeria: pattern and correlates. Social Psychiatry and Psychiatric Epidemiology. 2008;43(4):336–341. doi: 10.1007/s00127-007-0305-x. [DOI] [PubMed] [Google Scholar]
- 21.Cutting J. E. Perception and information. Annual Review of Psychology. 1987:3–30. doi: 10.1146/annurev.ps.38.020187.000425. [DOI] [PubMed] [Google Scholar]
- 22.Bill B. Experience and reason in perception. http://www2.warwick.ac.uk/fac/soc/philosophy/people/brewer/erp.pdf.


