Abstract
Background
To investigate whether very low mammographic breast density (VLD), HER2, and hormone receptor status holds any prognostic significance within the different prognostic categories of the widely used Nottingham Prognostic Index (NPI). We also aimed to see whether these factors could be incorporated into the NPI in an effort to enhance its performance.
Methods
This study included 270 patients with newly diagnosed invasive breast cancer. Patients with mammographic breast density of <10 % were considered as VLD. In this study, we compared the performance of NPI with and without VLD, HER2, ER and PR. Cox multivariate analysis, time-dependent receiver operating characteristic curve (tdROC), concordance index (c-index) and prediction error (0.632+ bootstrap estimator) were used to derive an updated version of NPI.
Results
Both mammographic breast density (VLD) (p < 0.001) and HER2 status (p = 0.049) had a clinically significant effect on the disease free survival of patients in the intermediate and high risk groups of the original NPI classification. The incorporation of both factors (VLD and HER2 status) into the NPI provided improved patient outcome stratification by decreasing the percentage of patients in the intermediate prognostic groups, moving a substantial percentage towards the low and high risk prognostic groups.
Conclusions
Very low density (VLD) and HER2 positivity were prognostically significant factors independent of the NPI. Furthermore, the incorporation of VLD and HER2 to the NPI served to enhance its accuracy, thus offering a readily available and more accurate method for the evaluation of patient prognosis.
Keywords: NPI, Breast density, Prognosis, Prediction, Nottingham prognostic index, HER2
Background
Breast cancer is a heterogeneous disease with differing behaviors and responses to therapy [1, 2]. Therefore, many prognostic models have been proposed for investigating patient outcome in relation to multiple patient and disease characteristics and to support clinical decision making. The Nottingham Prognostic Index (NPI) was first introduced in 1982 and has since been validated in independent large multicenter studies with long term follow up [3–6]. It is based on traditional prognostic factors such as tumor size, lymph node status and histological grade. It gives clinicians the ability to predict both the clinical outcome of tumors and the need for systemic therapies.
Mammographic breast density (MBD) refers to the relative abundance of fibrous and glandular tissues compared to the fat content of the breast as they appear on a normal X-ray mammogram. Increased MBD is considered as an established risk factor for breast cancer development [7], while previous studies reported that in patients with already diagnosed breast cancer tumors originating in breasts with very low density (VLD) were shown to be associated with a poorer prognosis even after correcting for possible confounders [8, 9].
Human Epidermal Growth Factor Receptor 2 (HER2) receptor is a membrane tyrosine kinase and is considered as a major driver of tumor development and progression [10]. Patients overexpressing HER2 historically showed a higher recurrence rates and a generally poorer outcome [11], but since the introduction of HER2-directed therapies significant improvements in patients’ outcomes have occurred. Nowadays, several guideline bodies recommend routine testing of HER2 and also adjuvant treatment with trastutsumab in HER2-positive cases [12, 13]. Estrogen receptor (ER) and progesterone receptor (PR) statuses are also well known prognostic and predictive factors and play a key role in breast cancer outcome and treatment [14]. This indicates that the aforementioned factors that are routinely available may also have a role in prediction accuracy enhancement if successfully incorporated into scoring systems such as the NPI.
In this study we set to examine the associations between very low mammographic breast density (VLD), HER2 status, ER and PR status in a homogenized patient group with matched NPI categories. Our main purpose was to assess whether those variables could be added to the NPI to form a new more accurate scoring system with enhanced prognostic and predictive values in order to better detect patients who are at high risk.
Methods
This study was based on a database of 278 breast carcinoma cases which was prospectively gathered to study the relationship of HER2 status and biological markers. The criteria for patient selection have been described elsewhere [15]. Shortly, 139 consecutive HER2 positive patients who were operated on in our university hospital were collected during the years 2002 – 2008 and matched with an equal amount of HER2 negative breast cancer cases with matching age and time of operation. All pathological, clinical and radiological data were blinded at the time of patient selection with the exception of HER2 status. The permission for this study was provided by the ethics committee of University of Eastern Finland, informed consent for this study was waived by the Finnish National Supervisor Authority for Welfare and Health (VALVIRA).
All available digital mammograms of the patients were then retrospectively collected and the analogue mammograms were digitized and collected into a database. Many of the patients in the study population have been diagnosed and referred from other hospitals and centers from our university hospital’s catchment area which means that multiple mammographic imaging systems have been used to obtain the diagnostic images used in the analyses. The diagnostic mammograms that first revealed the tumors were chosen for the evaluation as described previously [8]. The percentage of the area of the mammogram occupied by radiologically dense breast tissue were assessed using the craniocaudal projections and were determined visually. Eight patients had to be excluded after the initial collection because of unsatisfactory mammograms or missing projections bringing the final number of patients included in the analysis to 270.
All mammograms were first analyzed independently and then in consensus by five trained radiologists (three breast radiology specialists and two residents). The percentage of the area of the mammogram occupied by radiologically dense breast tissue was assessed visually from the craniocaudal projections and then distributed into six different percentile categories (<5, 5–10, 10–25, 25–50, 50–75 or >75 %). For the purpose of this study, density was dichotomized into Very Low Density (VLD; ≤10 %) and Mixed Density (MID; >10 %) to allow the variables to be treated as binary throughout the analysis. The expression of HER2 gene amplification was determined by the chromogenic in situ hybridization test (CISH test) by Zymed SPo-LightTM CISHTM Kit (Zymed 84-0146, San Francisco, CA). Cancers with six or more gene copies were considered as HER2 positive [16].
The NPI was calculated from the available data using the formula: NPI = tumor size (in cm) x 0.2 + histological grade (1–3) + lymph node points (negative node = 1; 1–3 positive node = 2; 4 or more positive node = 3) [17]. NPI was further subdivided into three prognostic categories: 1) -low risk, with NPI equal to or less than 3.4; 2) -medium risk, with NPI between 3.4 and 5.4; 3) -high risk, with NPI over 5.4.
The baseline characteristics of the patients have been presented previously [15] and are presented in (Table 1). The adjuvant treatments were given according to national guidelines which are in accordance with the international guidelines [18–20]. Chemotherapy was provided to 198 patients (73.3 %), hormonal treatment to 172 (63.7 %), while postoperative radiotherapy was given to 240 (88.9 %) patients. Adjuvant trastuzumab was routinely given to all HER2-positive patients from the year 2005 onwards, while before that it was given to select patients participating in a trial [21]. HER2-positive patients received adjuvant trastuzumab in 60 (45.1 %) of the 133 cases. For all events that occurred to patients in our study population, there was no difference in treatment plans between patients according to their dichotomized density profiles (Table 2). Follow up was collected from medical records and is up to date as of October 2014.
Table 1.
Clinicopathological characteristics of the patients
| Characteristic | Number of cases (%) |
|---|---|
| Patient number | 270 |
| Age (Years) | |
| Mean | 58.8 |
| Range | 32–86 |
| Postmenopausal (%) | 66.3 % |
| Mean tumor size (mm) | 22.73 |
| VLD patients | 21.47 (6–60) |
| MID patients | 23.46 (3–90) |
| Mean BMI | 26.70 |
| VLD patients | 25.46 (20.24–46.87) |
| MID patients | 28.84 (17.96–41.53) |
| HER2 positive | 133 (49.3 %) |
| Triple Negative | 17 |
| Tumor Pathological T classification | |
| T1 | 152 (56.3 %) |
| T2 | 95 (35.2 %) |
| T3 | 10 (3.7 %) |
| T4 | 13 (4.8 %) |
| Tumor N classification | |
| N0 | 100 (37.0 %) |
| N1 | 117 (43.3 %) |
| N2 | 34 (12.6 %) |
| N3 | 19 (7.0 %) |
| Definitive histology | |
| Ductal | 223 (82.6) |
| Lobular | 26 (9.6 %) |
| Mucinous | 4 (1.5 %) |
| Other | 17 (6.3 %) |
| Histological grade | |
| 1 | 22 (8.1 %) |
| 2 | 120 (44.4 %) |
| 3 | 128 (47.4 %) |
| Follow up time / years | |
| Mean | 8.03 |
| Range | 0.39–13.22 |
Table 2.
The p values for the differences in treatment options for patients who died or had a relapse (n = 57) according to their dichotomized density profiles
| VLD vs MID* | |
|---|---|
| Adjuvant chemotherapy | 0.398 |
| Herceptin | 0.229 |
| Hormonal Therapy | 0.419 |
| Radiotherapy | 0.762 |
*VLD very low densiy, MID Mixed density
Statistical analysis
Statistical analysis was performed with software (SPSS, version 19; SPSS, Chicago, Ill) and R (version 3.2.0) for Windows. Patients with bilateral disease (n = 8) had both breasts analyzed separately, one patient with bilateral disease and conflicting density readings between the breasts was integrated in the analysis by choosing the side with the worse stage and grade. The relationships between MBD, HER2 and NPI were evaluated using cross tabulation and McNemar’s non-parametric paired proportions test. Survival amongst the different patient groups was compared by the Kaplan-Meier method using log rank (Mantel-Cox) test. Univariate analysis was used on different categorical prognostic factors individually and Hazard Ratios (HR) with 95 % confidence intervals were estimated. Cox Multivariate analysis was then used in a backward stepwise manner to assess the factors combined until the best fit was obtained and HR and 95 % CI were recorded. Survival prediction model for breast cancer patients starting with NPI was followed by adding more variables to it to improve it and analyzed by using Cox multivariate analysis, time-dependent receiver operating characteristic curve (tdROC), concordance index (c-index) and prediction error (i.e. 0.632+ bootstrap estimator).
Results
The average NPI for our patient population was 4.66 (range 2.12–7.40), where 21.5 % (58/270) of patients belonged to the low risk prognostic group, 47.0 % (127/270) belonged to the intermediate risk group and 31.5 % (85/270) to the high risk group. As expected, patients’ disease free survival (DFS) declined with increasing values of NPI ranging from 91.4 % (53/58), 87.4 % (111/127), to 42.4 % (36/85) for patients in the low, intermediate and high risk groups of NPI respectively (p < 0.001).
Mammographic breast density, ER and PR statuses were normally distributed between the different NPI groups (p = 0.211, p = 0.528, p = 0.472, respectively). The percentage of HER2 positive patients progressively increased from the low (29.3 %, 17/58), intermediate (47.2 %, 60/127) and to the high risk (65.9 %, 56/85) prognostic groups of NPI (p < 0.001).
As mentioned earlier, patients in the intermediate risk group of NPI had a DFS of 87.4 % (111/127). The addition of VLD factor alone (HER2 negative patients) reduced survival to 82.6 % (19/23). The addition of both VLD and HER2 positivity at the same time reduced survival in this intermediate risk category to 70.0 % (14/20). The patients in this category who were both negative for HER2 and had MID breasts had a survival of 93.2 % (41/44), (p = 0.02).
In the high risk group of NPI, the DFS was 42.4 % (36/85) as mentioned earlier. The addition of VLD factor alone (HER2 negative patients) reduced survival to 30.0 % (3/10). The addition of both HER2 positivity and VLD simultaneously dropped survival to 10.5 % (2/19). Patients in this high risk category who were both HER2 negative and MID had a relatively better prognosis with a DFS of 63.2 % (12/19), (p = 0.001).
In our database, ER and PR statuses had no significant impact on survival in any of the groups of NPI. Unfortunately, the previously described analyses could not be performed in the low risk group due to the low number of patients in this group and the low number of events that have occurred there.
To assess the prognostic powers of those factors in more detail, we evaluated the survival percentages according to the different prognostic groups of NPI. First, as shown in Fig. 1a and b, the DFS for HER2 negative patients was significantly better than for HER2 positive patients in both the intermediate and the high risk groups respectively (89.6 vs 85.0 % and 51.7 vs 37.5 %; p = 0.049). The similar observation was made for patients according to their mammographic breast density (Fig. 1c and d), as DFS was lower in patients with VLD breasts both in the intermediate and high risk NPI groups respectively (92.9 vs 76.7 %, 55.4 vs 17.2 %; p < 0.001).
Fig. 1.
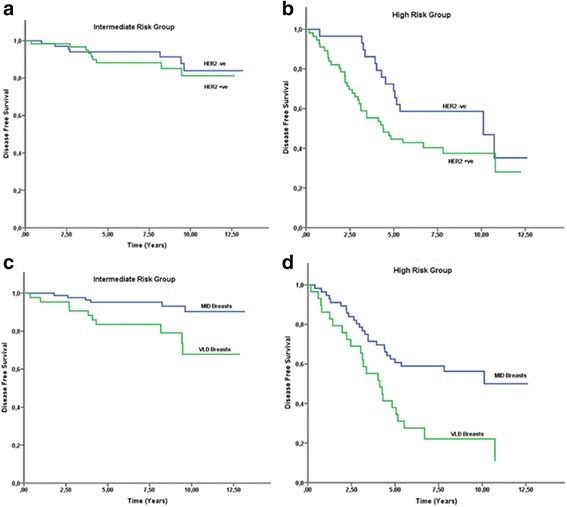
Patients’ Disease free survival graphs according to HER2 status and their MBDs. Graphis depiciting DFS according to patients’ HER2 receptor status (p = 0.049) separately for patients in the (a) intermediate and (b) high risk NPI groups. Disease free survival graphs according to patients’ dichotomized mammographic density values. (p < 0.001) separately for patients in the (c) intermediate and (d) high risk NPI groups
Five known prognostic factors (ER status, PR status, HER2 status, breast density and the NPI) first underwent univariate analysis to assess their prognostic powers on our patient population. Only three HR values turned out to be statistically significant (HER2 status, NPI and VLD). Second, those three factors which retained the significance were put through Cox multivariate analysis. The values for both analyses are shown in (Table 3). Both HER2 and MBD proved to provide prognostic information independent of NPI.
Table 3.
Hazard ratios of the prognostic factors in both the univariate and cox multivariate analysis
| Prognostic factor | HR | P | 95 % CI |
|---|---|---|---|
| Univariate analysis | |||
| HER2 status | 2.325 | 0.001 | 1.415–3.820 |
| MBD (VLD) | 1.986 | 0.004 | 1.238–3.187 |
| NPI | 2.295 | <0.001 | 1.845–2.854 |
| ER Status | 0.995 | 0.986 | 0.596–1.662 |
| PR Status | 1.135 | 0.613 | 0.695–1.851 |
| Multivariate analysis | |||
| HER2 status | 1.673 | 0.046 | 1.010–2.772 |
| NPI | 2.338 | <0.001 | 1.872–2.920 |
| MBD (VLD) | 2.790 | <0.001 | 1.724–4.516 |
Incorporating HER2 and MBD into the NPI
NPI, MBD, and HER2 were selected in a final model to form the Kuopio-Nottingham Prognostic Index (K-NPI) with parameter estimates of 0.89 (SE, 0.113), 1.01 (SE, 0.246) and 0.51 (SE, 0.258), respectively. Since the parameter estimates of NPI and MBD were highly similar, the new model was calculated as the sum of those individual variables, in addition to + 0.5 for HER2 positivity. The optimal new cut-offs, obtained with the 0.632+ bootstrap method, were 5.1 and 5.9, the concordance index of the K-NPI was 0.872 as compared to 0.779 for the original NPI. As a result, patients in the K-NPI were now categorized into low-, intermediate-, and high-risk groups for values below 5.1, between 5.1 and 5.9, and higher than 5.9, respectively.
The classification of patients into the low, intermediate and high risk groups according to the K-NPI is compared to the original NPI in (Table 4) and the DFS of the new groups is illustrated in Fig. 2a and b. The new system managed to classify considerably less patients into the intermediate group (55 as compared to 127 in the original NPI model, p < 0.001) as demonstrated in (Table 5). Out of the 127 patients previously classified as intermediate risk, 66 were now classified as low risk, 16 as high risk and 45 remained as intermediate. With respect to DFS, 92.7 % (115/124), 80.0 % (44/55) and 45.1 % (41/91) were disease free in the low, intermediate and high risk groups according to the KNPI respectively at the end of the follow up period.
Table 4.
Comparison between DFS in risk groups of the newly formed KNPI and the original NPI
| New Classification KNPI | Original NPI | p | |||
|---|---|---|---|---|---|
| Group | Patients (%) | DFS | Patients (%) | DFS | |
| Low risk | 124 (45.9) | 92.7 % (115/124) | 58 (21.5) | 91.4 % (53/58) | <0.001 |
| Intermediate risk | 55 (20.4) | 80.0 % (44/55) | 127 (47.0) | 87.4 % (111/127) | |
| High risk | 91 (33.7) | 45.1 % (41/91) | 85 (31.5) | 42.4 % (36/85) | |
| C Index | 0.872 | 0.779 | |||
The distribution of patients into the newly formed low, intermediate and high risk groups of the Kuopio-Nottingham Prognostic Index with their respective Disease Free Survival, compared to the old categories of the original Nottingham Prognostic Index
Fig. 2.
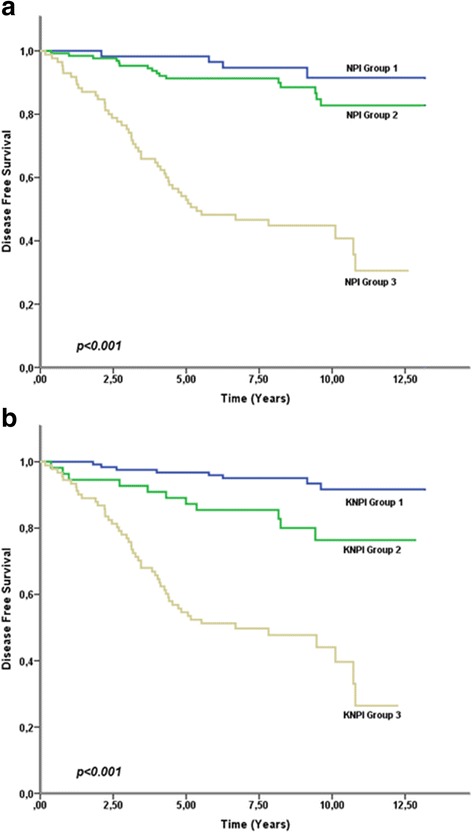
Graphs depicting DFS curves for risk groups of (a) the original NPI and (b) the newly coined KNPI
Table 5.
Distribution of the breast cancer patients (total n = 270) into different prognostic groups
| KNPI | ||||
|---|---|---|---|---|
| Low risk | Intermediate risk | High risk | Total | |
| NPI | ||||
| Low risk | 58 | 0 | 0 | 58 |
| Intermediate risk | 66 | 45 | 16 | 127 |
| High risk | 0 | 10 | 75 | 85 |
| Total | 124 | 55 | 91 | |
Agreement: 0.513, p < 0.001
Comparison of the original Nottingham Prognostic Index with the Kuopio-Nottingham Prognostic Index
Discussion
Breast cancer is a heterogeneous disease with varying phenotypes, genotypes, behaviours and responses to therapy. Adjuvant systemic treatments have helped to significantly decrease patient mortality. However, it is still difficult to evaluate which patients will benefit from adjuvant treatments and which patients will end up suffering from their toxicity [22, 23]. The principle finding of this study was that both HER2 status and very low mammographic breast density (VLD) proved to be independent of the classically used NPI and serve to improve its predictive ability. In our patient population, the original NPI classified a rather high proportion of patients into the intermediate risk group making it challenging to evaluate the need and benefit of adjuvant chemotherapy. With the new K-NPI, a considerable group of patients were moved from the intermediate to the low or high risk groups which might hold clinical significance in terms of adjuvant treatment decisions.
In line with our results, several studies have shown that HER2 status is a predictive factor independent of the NPI [24–26]. Although Van Belle et al. [26] managed to create a new prognostic classification system (dubbed the iNPI) by incorporating both HER2 and Progesterone status into the NPI, our results in contrast indicated that neither ER nor PR statuses were prognostically significant, which is in line with studies proposing that hormone receptors lose their prognostic power in the long term [27].
Previous studies have investigated the addition of several different factors to the NPI and whether those could serve to improve its predictive value in regards to patient prognosis [26, 28–31]. Mammographic breast density however has never been incorporated into a prognostic index before this trial, even though it is a routinely available, cost-free and easily interpreted parameter in patients with newly diagnosed breast cancer. Our results now show that MBD is a predictive factor independent of the NPI. Furthermore, it can be added to NPI simultaneously with HER2 status to give a synergistic advantage to its predictive ability, especially in the ubiquitous intermediate prognostic category of NPI. It can be clearly seen that MBD and HER2 status were major determinants in switching patients from the original NPI intermediate group to the new K-NPI low risk and high risk groups, density as shown in Table 6.
Table 6.
The distribution of density categories and HER2 status in the patients who were in the original intermediate category of the NPI compared to their new distribution in the K-NPI
| Density | HER2 | |
|---|---|---|
| Low risk | VLD 3 (4.5 %) | HER2+ 25 (37.9 %) |
| MID 63 (95.5 %) | HER2– 41 (62.1 %) | |
| Intermediate risk | VLD 24 (53.3 %) | HER2+ 24 (53.3 %) |
| MID 21 (46.7 %) | HER2– 21 (46.7 %) | |
| High risk | VLD 16 (100 %) | HER2+ 11 (68.8 %) |
| MID 0 (0 %) | HER2– 5 (31.3 %) |
Our study is not without limitations. Our patient population is relatively small and we only had a limited number of triple negative cancers. And due to our patient selection criteria, our study had a higher percentage of HER2 positive patients than fully consecutive cohorts. Many of our patients have been treated with adjuvant therapies making it difficult to predict the exact role of the primary prognostic factors and how the treatments have affected the results. However, at the time of patient collection, the national guidelines in Finland were very similar to current guidelines. A notable exception was the addition of trastuzumab as a standard to HER2 positive patients in the year 2005, while before that trastuzumab was offered only for patients participating in the FinHer trial [21]. Furthermore, mammographic density was measured visually which may be considered less accurate by some, but we aimed to select a method that is easily reproducible in clinical practice and does not require the addition of expensive and sometimes complicated programs.
Another commonly used tool to evaluate patient outcome nowadays is the Adjuvant! Online prognostic index. It is an internet based computer programme providing 10-year prognosis predictions for early breast cancer patients. Its use has increased in recent years; however, its validation in different cohorts has not been as successful as its counterpart the NPI with many studies finding wide discrepancies between its reported predictions and actual survivals [32–34].
In the future, prognostic classification may benefit from newer methods such as microarray-based gene expression profiling [35]. Multigene signatures associated with prognosis have recently emerged and some are even commercially available [36]. Drukker et al. [37] showed a prognostic benefit by combining the 70-gene signature with the classical scoring systems. Nevertheless, these gene signatures carry many shortcomings, different multigene tests give different and variating results making their implementation into clinical practice difficult [38, 39]. This may be due to intratumoral genetic variation and heterogeneity in the microenvironment. Although these new markers may provide additional prognostic data, only a very limited number of patients could benefit from them due to the high costs of the tests. Thus, if we consider breast cancer as a global prolem, the classical clinical markers are still needed and new multigene tests should be considered complimentary and not a replacement for traditional parameters [40, 41]. Many breast cancer cases are diagnosed in the developing world where resources are scarce making those disadvantages particularly important, and that’s where the need stems for new, simple and easily available prognostic factors that are easy to interpret and can be easily combined with the classical clinicopathological scoring systems [23, 42]. HER2 status is nowadays measured routinely in most countries, and MBD can be easily acquired from the diagnostic mammograms, hence not requiring any extra time or money.
Conclusions
In conclusion, our results show that for patients with early breast cancer MBD and HER2 status are indeed strong prognostic factors independent of the NPI. Furthermore, we were able to enhance the prognostic ability of NPI by the addition of HER2 status and breast density values into the newly coined K-NPI. This prognostic reclassification managed to significantly decrease the percentage of patients in the intermediate risk group, which serves to more reliably recognize those patients who are in the real higher risk group. Future work with larger patient populations, and with quantitative density measurement methods must be carried out to validate the clinical utility of our observations.
Acknowledgements
Authors are thankful for Tuomas Selander for kindly providing statistical advice for this manuscript.
Funding
Financial support was received from Kuopio University Hospital-VTR funds (RV, PA), EVO funding (grant nos. 5063525, 5063532) (AM, RV, AS), grants from the Instrumentarium foundation (AM), Cancer Center of Eastern Finland (AM), Radiological society of Finland (AM, MS), Finnish Oncological Society (AM), Inkeri and Mauri Vänskä foundation (AM), Finnish Medical Foundation (AM, MS), Northern Savo Cancer association (AM) and the Cancer Society of Finland (AM, RV, MS).
Availability of data and materials
Information about dataset supporting the conclusions of this article is available on request through the corresponding author’s email address.
Authors’ contributions
AM, MS and AS participated in the density measurements and mammographic analysis. PA, MS, VD, OA, AS, SA, VMK, and RV revised the manuscript critically and analysed the data for important intellectual content. PA, SO analysed the histological sections. AM, MS, VD, PA, AS and RV participated in the design of the study. AM, VD, OA, AS, SA, VMK and RV coordinated and helped in drafting the manuscript. All authors read and approved the final draft of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The permission for this study was provided by the ethics committee of University of Eastern Finland. The need for written informed consent for this retrospective study was waived by the Finnish National Supervisor Authority for Welfare and Health (VALVIRA).
Abbreviations
- c-index
Concordance index
- CISH
Chromogenic In situ hybridization test
- DFS
Disease free survival
- ER
Estrogen receptor
- HER2
Human Epidermal Growth Factor Receptor 2
- K-NPI
Kuopio-Nottingham Prognostic Index
- MBD
Mammographic breast density
- MID
Mixed density
- NPI
Nottingham Prognostic Index
- PR
Progesterone receptor
- SE
Standard error
- tdROC
Time-dependent receiver operating characteristic curve
- VLD
Very low density
Contributor Information
Amro Masarwah, Phone: +35845808964, Email: amro.masarwah@kuh.fi.
Päivi Auvinen, Email: paivi.auvinen@kuh.fi.
Mazen Sudah, Email: mazen.sudah@kuh.fi.
Vaiva Dabravolskaite, Email: vaivadabravolskaite@gmail.com.
Otso Arponen, Email: otso.arponen@kuh.fi.
Anna Sutela, Email: anna.sutela@kuh.fi.
Sanna Oikari, Email: sanna.oikari@uef.fi.
Veli-Matti Kosma, Email: veli-matti.kosma@uef.fi.
Ritva Vanninen, Email: ritva.vanninen@kuh.fi.
References
- 1.Almendro V, Fuster G. Heterogeneity of breast cancer: etiology and clinical relevance. Clin Transl Oncol. 2011;13(11):767–73. doi: 10.1007/s12094-011-0731-9. [DOI] [PubMed] [Google Scholar]
- 2.Polyak K. Heterogeneity in breast cancer. J Clin Invest. 2011;121(10):3786–8. doi: 10.1172/JCI60534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balslev I, Axelsson CK, Zedeler K, Rasmussen BB, Carstensen B, Mouridsen HT. The Nottingham Prognostic Index applied to 9,149 patients from the studies of the Danish Breast Cancer Cooperative Group (DBCG) Breast Cancer Res Treat. 1994;32(3):281–90. doi: 10.1007/BF00666005. [DOI] [PubMed] [Google Scholar]
- 4.Blamey RW, Ellis IO, Pinder SE, Lee AH, Macmillan RD, Morgan DA, Robertson JF, Mitchell MJ, Ball GR, Haybittle JL, Elston CW. Survival of invasive breast cancer according to the Nottingham Prognostic Index in cases diagnosed in 1990-1999. Eur J Cancer. 2007;43(10):1548–55. doi: 10.1016/j.ejca.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 5.D'Eredita G, Giardina C, Martellotta M, Natale T, Ferrarese F. Prognostic factors in breast cancer: the predictive value of the Nottingham Prognostic Index in patients with a long-term follow-up that were treated in a single institution. Eur J Cancer. 2001;37(5):591–6. doi: 10.1016/S0959-8049(00)00435-4. [DOI] [PubMed] [Google Scholar]
- 6.Sundquist M, Thorstenson S, Brudin L, Nordenskjold B. Applying the Nottingham Prognostic Index to a Swedish breast cancer population. South East Swedish Breast Cancer Study Group. Breast Cancer Res Treat. 1999;53(1):1–8. [DOI] [PubMed]
- 7.McCormack VA, dos Santos SI. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2006;15(6):1159–69. doi: 10.1158/1055-9965.EPI-06-0034. [DOI] [PubMed] [Google Scholar]
- 8.Masarwah A, Auvinen P, Sudah M, Rautiainen S, Sutela A, Pelkonen O, Oikari S, Kosma VM, Vanninen R. Very low mammographic breast density predicts poorer outcome in patients with invasive breast cancer. Eur Radiol. 2015;25(7):1875–82. doi: 10.1007/s00330-015-3626-2. [DOI] [PubMed] [Google Scholar]
- 9.Masarwah A, Tammi M, Sudah M, Sutela A, Oikari S, Kosma VM, Tammi R, Vanninen R, Auvinen P. The reciprocal association between mammographic breast density, hyaluronan synthesis and patient outcome. Breast Cancer Res Treat. 2015;153(3):625–34. doi: 10.1007/s10549-015-3567-0. [DOI] [PubMed] [Google Scholar]
- 10.Krishnamurti U, Silverman JF. HER2 in breast cancer: a review and update. Adv Anat Pathol. 2014;21(2):100–7. doi: 10.1097/PAP.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 11.Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987;235(4785):177–82. doi: 10.1126/science.3798106. [DOI] [PubMed] [Google Scholar]
- 12.Walker RA, Bartlett JM, Dowsett M, Ellis IO, Hanby AM, Jasani B, Miller K, Pinder SE. HER2 testing in the UK: further update to recommendations. J Clin Pathol. 2008;61(7):818–24. doi: 10.1136/jcp.2007.054866. [DOI] [PubMed] [Google Scholar]
- 13.Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M, Fitzgibbons P, Hanna W, Jenkins RB, Mangu PB, Paik S, Perez EA, Press MF, Spears PA, Vance GH, Viale G, Hayes DF, American Society of Clinical Oncology, College of American Pathologists Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013;31(31):3997–4013. doi: 10.1200/JCO.2013.50.9984. [DOI] [PubMed] [Google Scholar]
- 14.Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, Fitzgibbons PL, Francis G, Goldstein NS, Hayes M, Hicks DG, Lester S, Love R, Mangu PB, McShane L, Miller K, Osborne CK, Paik S, Perlmutter J, Rhodes A, Sasano H, Schwartz JN, Sweep FC, Taube S, Torlakovic EE, Valenstein P, Viale G, Visscher D, Wheeler T, Williams RB, Wittliff JL, Wolff AC. American Society of Clinical Oncology/College Of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol. 2010;28(16):2784–95. doi: 10.1200/JCO.2009.25.6529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Auvinen P, Tammi R, Kosma VM, Sironen R, Soini Y, Mannermaa A, Tumelius R, Uljas E, Tammi M. Increased hyaluronan content and stromal cell CD44 associate with HER2 positivity and poor prognosis in human breast cancer. Int J Cancer. 2013;132(3):531–9. doi: 10.1002/ijc.27707. [DOI] [PubMed] [Google Scholar]
- 16.Isola J, Tanner M, Forsyth A, Cooke TG, Watters AD, Bartlett JM. Interlaboratory comparison of HER-2 oncogene amplification as detected by chromogenic and fluorescence in situ hybridization. Clin Cancer Res. 2004;10(14):4793–8. doi: 10.1158/1078-0432.CCR-0428-03. [DOI] [PubMed] [Google Scholar]
- 17.Galea MH, Blamey RW, Elston CE, Ellis IO. The Nottingham Prognostic Index in primary breast cancer. Breast Cancer Res Treat. 1992;22(3):207–19. doi: 10.1007/BF01840834. [DOI] [PubMed] [Google Scholar]
- 18.Senkus E, Kyriakides S, Penault-Llorca F, Poortmans P, Thompson A, Zackrisson S, Cardoso F, ESMO Guidelines Working Group Primary breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24(Suppl 6):vi7–23. doi: 10.1093/annonc/mdt284. [DOI] [PubMed] [Google Scholar]
- 19.Goldhirsch A, Winer EP, Coates AS, Gelber RD, Piccart-Gebhart M, Thurlimann B, Senn HJ, Panel members Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary therapy of early breast cancer 2013. Ann Oncol. 2013;24(9):2206–23. doi: 10.1093/annonc/mdt303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Theriault RL, Carlson RW, Allred C, Anderson BO, Burstein HJ, Edge SB, Farrar WB, Forero A, Giordano SH, Goldstein LJ, Gradishar WJ, Hayes DF, Hudis CA, Isakoff SJ, Ljung BM, Mankoff DA, Marcom PK, Mayer IA, McCormick B, Pierce LJ, Reed EC, Schwartzberg LS, Smith ML, Soliman H, Somlo G, Ward JH, Wolff AC, Zellars R, Shead DA, Kumar R, National Comprehensive Cancer Network Breast cancer, version 3.2013: featured updates to the NCCN guidelines. J Natl Compr Canc Netw. 2013;11(7):753–60. doi: 10.6004/jnccn.2013.0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joensuu H, Bono P, Kataja V, Alanko T, Kokko R, Asola R, Utriainen T, Turpeenniemi-Hujanen T, Jyrkkio S, Moykkynen K, Helle L, Ingalsuo S, Pajunen M, Huusko M, Salminen T, Auvinen P, Leinonen H, Leinonen M, Isola J, Kellokumpu-Lehtinen PL. Fluorouracil, epirubicin, and cyclophosphamide with either docetaxel or vinorelbine, with or without trastuzumab, as adjuvant treatments of breast cancer: final results of the FinHer trial. J Clin Oncol. 2009;27(34):5685–92. doi: 10.1200/JCO.2008.21.4577. [DOI] [PubMed] [Google Scholar]
- 22.Schmidt M, Victor A, Bratzel D, Boehm D, Cotarelo C, Lebrecht A, Siggelkow W, Hengstler JG, Elsasser A, Gehrmann M, Lehr HA, Koelbl H, von Minckwitz G, Harbeck N, Thomssen C. Long-term outcome prediction by clinicopathological risk classification algorithms in node-negative breast cancer--comparison between Adjuvant! St Gallen, and a novel risk algorithm used in the prospective randomized Node-Negative-Breast Cancer-3 (NNBC-3) trial. Ann Oncol. 2009;20(2):258–64. [DOI] [PubMed]
- 23.Weigelt B, Reis-Filho JS. Molecular profiling currently offers no more than tumour morphology and basic immunohistochemistry. Breast Cancer Res. 2010;12(Suppl 4):S5. doi: 10.1186/bcr2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cooke T, Reeves J, Lannigan A, Stanton P. The value of the human epidermal growth factor receptor-2 (HER2) as a prognostic marker. Eur J Cancer. 2001;37(Suppl 1):S3–10. doi: 10.1016/S0959-8049(00)00402-0. [DOI] [PubMed] [Google Scholar]
- 25.Rakha EA, Soria D, Green AR, Lemetre C, Powe DG, Nolan CC, Garibaldi JM, Ball G, Ellis IO. Nottingham Prognostic Index Plus (NPI+): a modern clinical decision making tool in breast cancer. Br J Cancer. 2014;110(7):1688–97. doi: 10.1038/bjc.2014.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Van Belle V, Van Calster B, Brouckaert O, Vanden Bempt I, Pintens S, Harvey V, Murray P, Naume B, Wiedswang G, Paridaens R, Moerman P, Amant F, Leunen K, Smeets A, Drijkoningen M, Wildiers H, Christiaens MR, Vergote I, Van Huffel S, Neven P. Qualitative assessment of the progesterone receptor and HER2 improves the Nottingham Prognostic Index up to 5 years after breast cancer diagnosis. J Clin Oncol. 2010;28(27):4129–34. doi: 10.1200/JCO.2009.26.4200. [DOI] [PubMed] [Google Scholar]
- 27.Hilsenbeck SG, Ravdin PM, de Moor CA, Chamness GC, Osborne CK, Clark GM. Time-dependence of hazard ratios for prognostic factors in primary breast cancer. Breast Cancer Res Treat. 1998;52(1-3):227–37. doi: 10.1023/A:1006133418245. [DOI] [PubMed] [Google Scholar]
- 28.Callagy GM, Pharoah PD, Pinder SE, Hsu FD, Nielsen TO, Ragaz J, Ellis IO, Huntsman D, Caldas C. Bcl-2 is a prognostic marker in breast cancer independently of the Nottingham Prognostic Index. Clin Cancer Res. 2006;12(8):2468–75. doi: 10.1158/1078-0432.CCR-05-2719. [DOI] [PubMed] [Google Scholar]
- 29.Collett K, Skjaerven R, Maehle BO. The prognostic contribution of estrogen and progesterone receptor status to a modified version of the Nottingham Prognostic Index. Breast Cancer Res Treat. 1998;48(1):1–9. doi: 10.1023/A:1005945000264. [DOI] [PubMed] [Google Scholar]
- 30.Hansen S, Grabau DA, Sorensen FB, Bak M, Vach W, Rose C. Vascular grading of angiogenesis: prognostic significance in breast cancer. Br J Cancer. 2000;82(2):339–47. doi: 10.1054/bjoc.1999.0924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Malmstrom P, Bendahl PO, Boiesen P, Brunner N, Idvall I, Ferno M, South Sweden Breast Cancer Group S-phase fraction and urokinase plasminogen activator are better markers for distant recurrences than Nottingham Prognostic Index and histologic grade in a prospective study of premenopausal lymph node-negative breast cancer. J Clin Oncol. 2001;19(7):2010–9. doi: 10.1200/JCO.2001.19.7.2010. [DOI] [PubMed] [Google Scholar]
- 32.Bhoo-Pathy N, Yip CH, Hartman M, Saxena N, Taib NA, Ho GF, Looi LM, Bulgiba AM, van der Graaf Y, Verkooijen HM. Adjuvant! Online is overoptimistic in predicting survival of Asian breast cancer patients. Eur J Cancer. 2012;48(7):982–9. doi: 10.1016/j.ejca.2012.01.034. [DOI] [PubMed] [Google Scholar]
- 33.Campbell HE, Taylor MA, Harris AL, Gray AM. An investigation into the performance of the Adjuvant! Online prognostic programme in early breast cancer for a cohort of patients in the United Kingdom. Br J Cancer. 2009;101(7):1074–84. doi: 10.1038/sj.bjc.6605283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jung M, Choi EH, Nam CM, Rha SY, Jeung HC, Lee SH, Yang WI, Roh JK, Chung HC. Application of the adjuvant! Online model to Korean breast cancer patients: an assessment of prognostic accuracy and development of an alternative prognostic tool. Ann Surg Oncol. 2013;20(8):2615–24. doi: 10.1245/s10434-013-2956-z. [DOI] [PubMed] [Google Scholar]
- 35.Kumar R, Sharma A, Tiwari RK. Application of microarray in breast cancer: An overview. J Pharm Bioallied Sci. 2012;4(1):21–6. doi: 10.4103/0975-7406.92726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Callagy G, Cattaneo E, Daigo Y, Happerfield L, Bobrow LG, Pharoah PD, Caldas C. Molecular classification of breast carcinomas using tissue microarrays. Diagn Mol Pathol. 2003;12(1):27–34. doi: 10.1097/00019606-200303000-00004. [DOI] [PubMed] [Google Scholar]
- 37.Drukker CA, Nijenhuis MV, Bueno-de-Mesquita JM, Retel VP, van Harten WH, van Tinteren H, Wesseling J, Schmidt MK, Van't Veer LJ, Sonke GS, Rutgers EJ, van de Vijver MJ, Linn SC. Optimized outcome prediction in breast cancer by combining the 70-gene signature with clinical risk prediction algorithms. Breast Cancer Res Treat. 2014;145(3):697–705. doi: 10.1007/s10549-014-2954-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cardoso F. Show me the genes - I will tell you who/how to treat! Breast Cancer Res. 2005;7(2):77–9. doi: 10.1186/bcr1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sparano JA, Ostrer H, Kenny PA. Translating genomic research into clinical practice: promise and pitfalls. Am Soc Clin Oncol Educ Book. 2013;15–23. doi:10.1200/EdBook_AM.2013.33.15. [DOI] [PubMed]
- 40.Eden P, Ritz C, Rose C, Ferno M, Peterson C. "Good Old" clinical markers have similar power in breast cancer prognosis as microarray gene expression profilers. Eur J Cancer. 2004;40(12):1837–41. doi: 10.1016/j.ejca.2004.02.025. [DOI] [PubMed] [Google Scholar]
- 41.Weigelt B, Baehner FL, Reis-Filho JS. The contribution of gene expression profiling to breast cancer classification, prognostication and prediction: a retrospective of the last decade. J Pathol. 2010;220(2):263–80. doi: 10.1002/path.2648. [DOI] [PubMed] [Google Scholar]
- 42.Altman DG. Prognostic models: a methodological framework and review of models for breast cancer. Cancer Invest. 2009;27(3):235–43. doi: 10.1080/07357900802572110. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Information about dataset supporting the conclusions of this article is available on request through the corresponding author’s email address.


