Abstract
Background
China’s nutrition transition is characterized by dramatic increases in overweight and cardiometabolic (CM) risk. The burden of obesity, CM risk factors and dietary intake among Chinese children were explored.
Methods
Children 7-12y old from the 2009 China Health and Nutrition Survey with available dietary intake data, anthropometry, blood pressure, and fasting blood samples were included (n=663). CM risk prevalence was calculated; logistic regression was used to investigate the association of nutrient intakes with CM risk, adjusting for age, gender, physical activity, area of residence and income.
Results
14% of Chinese school-aged children and ~20% of those from urban areas and higher income households had overweight/obesity (p<0.05). The prevalence of prehypertension was ~20% while hypertension was 14%. Around 20% of all children and ≥30% of those from urban areas and higher income households had impaired glucose/HbA1c (p<0.05). More than half of the studied children had pre-dyslipidemia (i.e. at least one lipid measurement above borderline levels) and 21% of children had dyslipidemia. Approximately 30% of all children had energy intakes above requirements and 38% of them had excessive proportions of dietary fat and saturated fat. Children with higher intakes of total daily energy and total and added sugars had a greater likelihood of having impaired blood pressure and glucose/HbA1c.
Conclusions
Childhood overweight and CM risk is prevalent in urban and rural areas of China and across different socioeconomic groups although disparities between classes still pervade. Several dietary factors such as sugars were significant correlates of CM risk.
Keywords: obesity, cardiometabolic risk, dietary intake, children, China
INTRODUCTION
Coincident with a rapid social and economic transition in China, the rates of childhood overweight and obesity have increased across all age and socioeconomic (SES) groups.1-3 These trends have been remarkably notable in highly urbanized areas,4 where traditional diets and patterns of physical activity have shifted more dramatically.5,6 China’s eating patterns are currently moving towards higher intake of fat, animal-source and processed foods, away-from-home eating and snacking.6-8
Important increases in the prevalence of non-communicable disease (NCD) risk factors have been documented in parallel with these changes.4,9-12 In 2009, around 42% of Chinese children and adolescents presented at least one cardiometabolic (CM) risk factor such as hypertension, diabetes or dyslipidemia. Overall weight status, abdominal obesity and low physical activity were strong predictors of CM risk.4,9 These observed trends reveal the expanding burden of NCDs and their associated risks of morbidity and mortality in modernizing China.
The Chinese pediatric population is of special concern, not only because of their increasing rates of NCDs, but also because the high-risk lifestyle patterns that currently affect child health may continue tracking into adulthood or even worsen. To date, few studies have investigated NCDs and associated factors in China,4,9 but none has focused exclusively on children to explore the prevalence of obesity and CM risk factors and their relationship with selected dietary factors.
The present study used measures of dietary intake (i.e. energy, macro- and micronutrients), body composition (i.e. height and weight), blood pressure (BP) (i.e. Systolic BP and Diastolic BP), plasma markers of glucose (i.e. fasting glucose and Hemoglobin A1c (HbA1c)) and lipid metabolism (i.e. total cholesterol (TC), low-density (LDL) and high-density (HDL) lipoprotein cholesterol and triglycerides (TG)) from a sample of children 7-12 y who participated in the 2009 China Health and Nutrition Survey. The prevalence of CM risk factors and mean dietary intakes across strata of urban vs. rural areas and income groups was calculated. Associations between macro- and micronutrient intakes and obesity and CM risk factors were also explored. This study provides current data on the burden of overweight and NCDs among Chinese school-age children and brings further insights into the importance of some nutrients in the etiology of these chronic conditions. It is essential to understand and recognize the role of these nutrients on child health, as some of them are increasingly becoming an important part of the Chinese diet over the past decades.6,7
MATERIAL AND METHODS
Study population: the China Health and Nutrition Survey (CHNS)
The present study used the 2009 CHNS, a large-scale on-going longitudinal household-based cohort established in China in 1989.13,14 The CHNS was based on a multi-stage random cluster process implemented to randomly select individuals from 228 communities in 9 provinces from a wide range of economic and demographic categories.
Since the baseline survey, the CHNS has only collected blood samples in 2009. Dietary intake, anthropometric measures, blood pressure and detailed individual, household and community sociodemograpic data were collected by trained interviewers at each home visit spanning 3 days.14 The sample analyzed in this cross-sectional study includes children aged 7-12 from the 2009 CHNS (n=663) with available anthropometric data. Survey instruments, protocols and informed consents were approved by the institutional review committee of the University of North Carolina at Chapel Hill, the National Institute of Nutrition and Food Safety, the Chinese Center for Disease Control and Prevention, and the China-Japan Friendship Hospital, Ministry of Health.
Anthropometry and cardiometabolic (CM) disease risk factors
Anthropometric measurements were collected in light clothes and without shoes: weight was measured to the nearest 0.1 kg using a calibrated scale; height was measured to the nearest 0.2 cm using a portable Seca stadiometer (Seca North America, Chino, CA, USA). Body mass index was calculated dividing weight (kg) by the squared height (m). The International Obesity Task Force body mass index (BMI) cut points by age and sex15 were used to classify children according to their weight status. Underweight, normal weight, overweight and obesity cut-points correspond to an adult BMI of 18.5 (underweight), 25 (overweight) and 30 (obesity).
Fasting blood samples and blood pressure were obtained from individuals ≥7-y who visited a neighborhood clinic. Protocols and laboratory analysis methods are explained in detail elsewhere.4 For blood pressure, the mean of 3 measurements collected after a 10-min seated rest was used. The present study focuses on systolic (SBP) and diastolic blood pressure (DBP); biomarkers of glucose metabolism including fasting glucose and hemoglobin A1c (HbA1c); and biomarkers of dyslipidemia including total cholesterol (TC), low-density (LDL) and high-density (HDL) lipoprotein cholesterol and triglycerides (TG).
Internationally accepted cutoff values of CM risk were used to classify children in this study. For blood pressure, age- and gender-specific BP reference standards for Chinese children were used to define pre-hypertension (>90th percentile of SBP, DBP or both) and hypertension (>95% percentile of SBP, DBP or both).16 For impaired glucose metabolism, the criteria defined by the American Diabetes Association for increased risk of diabetes was used (fasting glucose ≥100mg/dL and HbA1c ≥5.7%).17 For dyslipidemia, pediatric-specific cutoff values defined by the National Cholesterol Education Program (NCEP) Expert Panel on Cholesterol Levels in Children were used: borderline values TC≥170 mg/dL, LDL≥110 mg/dL, HDL≤45 mg/dL, TG≥75 mg/dL for 0-9y and ≥90 mg/dL for 10-19y; high values TC≥200 mg/dL, LDL≥130 mg/dL, HDL<35 mg/dL, TG≥100 mg/dL for 0-9y and ≥130 mg/dL for 10-19y.18,19 Pre-dyslipidemia was defined as having at least one marker exceeding borderline cutoff values, whereas dyslipidemia was defined as having at least one marker exceeding high cutoff values.
Dietary intake measurements
Dietary intake was self-reported by children ≥12y or by the child’s caregiver for children <12y of age,6 and was collected using three consecutive 24-h recalls plus supplemental information from a daily household food inventory. The 3-day average of energy and nutrient intakes was used for this analysis.
The present study reported total daily energy and macronutrients (i.e. protein, total fat and carbohydrates), total and added sugars, saturated fat, monounsaturated fat, polyunsaturated fat, sodium and potassium. The latest Chinese food composition table was used, which includes approximately 2,500 foods.20 For nutrients that were not available in the Chinese FCT, such as saturated fat, total and added sugars, nutrient values were used from the USDA Food and Nutrient Database for Dietary Studies (FNDDS) or the National Nutrient Database for Standard Reference (SR),21 which were matched as closely as possible with foods in the Chinese food composition table.
To investigate the prevalence of inadequate or excessive intakes, the Chinese Dietary Reference Intakes (DRIs) were used to calculate the proportion of participants above and below defined Chinese DRI cutoff values.22 To examine if children were in energy balance, total energy intakes by age group were evaluated against Estimated Energy Requirements (EER) cutoffs for light physical activity (PA). Light PA cutoffs were used because our PA measurement was insufficient to classify children with light, moderate or heavy PA, and because low PA levels have been previously reported among children in the CHNS.23 Nutrient adequacies were evaluated using Estimated Average Requirements (EAR) and Acceptable Macronutrient Distribution Ranges (AMDR).24 Proposed Intakes for Preventing Non-communicable Chronic Diseases (PI-NCD), a Chinese dietary goal for disease prevention, was used to study the % of the population with excessive intakes of sodium and potassium.22
Socioeconomic (SES) variables and physical activity (PA)
Demographic characteristics were collected for each individual at home visits, including age, gender, area of residence; plus net household income and education of the primary caregiver (Additional Table 1). Based on population density, area of residence was categorized as urban or rural by calculating the total population of the community divided by the total community area from official records. Total net household income was calculated as the sum of incomes of all earners in the household, and was divided into tertiles for a proxy of lower, medium and higher income.
Daily PA was measured using questionnaires that collected the time spent in all activities in a typical week, including work, leisure, travel and household chores. A summary measure expressed as total metabolic equivalents (METs) was created multiplying the time spent in each activity by the METs of each activity.
Statistical analyses
Statistical analyses were performed using Stata (Release 13.0, Stata Corp., College Station, TX, USA). For descriptive analyses, results are presented as crude prevalences or population means (SE). Means and prevalences were calculated within strata of area of residence, income and weight status. Differences between groups of urban/rural, gender, income and weight status were tested using Student’s t test for means or X2 test for prevalence data. Logistic regression models were used to investigate the association of nutrient intakes with each CM risk factor, adjusting for age, gender, PA, area of residence and income. A p value of 0.05 was set to denote statistical significance.
RESULTS
Prevalence of cardiometabolic risk factors
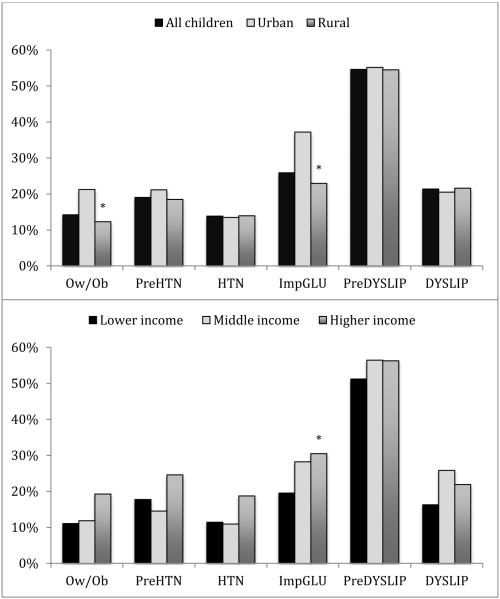
Approximately 14% of Chinese school-aged children were overweight or obese (Table 1). The prevalence was nearly 20% among children from urban areas and those from higher income households (p<0.05) (Figure 1). The prevalence of prehypertension was almost 20% while hypertension was 14%. Around 1 in 4 children had impaired glucose or HbA1c; ≥30% of children from urban areas and higher income households had impaired glucose or HbA1c (p<0.05). The prevalence of high triglycerides was 17% whereas the prevalence of children with lipid values exceeding borderline cut-points was 23% for total cholesterol, 13% for LDL and 14% for HDL. More than half of the studied children had pre-dyslipidemia (i.e. at least one lipid measurement exceeding borderline lipid cut-points) and 21% of children had dyslipidemia (i.e. at least one lipid measurement exceeding high lipid cut-points).
Table 1.
Prevalence (%) of cardiometabolic risk factors among children 7-12, (CHNS 2009).
|
|
|||
| Prevalence of risk factor | |||
|
| |||
|
Weight status
n=613 |
Mean ± SE |
%
Overweight/obesity |
|
|
| |||
| Body Mass Index (kg/m2) | 16.7 ± 3.09 | ||
| % Underweight | 25 | ||
| % Normal weight | 61 | 14 | |
| % Overweight | 11 | ||
| % Obesity | 3 | ||
|
| |||
|
Blood Pressure
n=499 |
Mean ± SE |
%
Pre-HTN |
%
HTN |
|
| |||
| SBP (mmHg) | 95.6 ± 12.9 | ||
| % >90th | 7 | ||
| % >95th | 4 | 19 | 14 |
| DBP (mmHg) | 64.4 ± 9.46 | ||
| % >90th | 17 | ||
| % >95th | 14 | ||
|
| |||
|
Glucose metabolism
n=379 |
Mean ± SE |
% Impaired
glucose/HbA1c |
|
|
| |||
| Fasting blood glucose (mg/dL) | 88.8 ± 17.9 | ||
| % ≥100 mg/dL | 9 | 26 | |
| Hemoglobin A1c (%) | 5.31 ± 0.56 | ||
| % ≥5.7% | 20 | ||
|
| |||
|
Lipid metabolism
n=379 |
Mean ± SE |
% Pre-
dyslipidemia |
%
Dyslipidemia |
|
| |||
| TC (mg/dL) | 153 ± 26.8 | ||
| % ≥170 mg/dL | 23 | ||
| % ≥200 mg/dL | 4 | ||
| LDL (mg/dL) | 85.0 ± 23.8 | ||
| % ≥110 mg/dL | 13 | ||
| % ≥130 mg/dL | 3 | 55 | 21 |
| HDL (mg/dL) | 57.2 ± 12.3 | ||
| % ≥45 mg/dL | 14 | ||
| % <35 mg/dL | 2 | ||
| TAG (mg/dL) | 85.1 ± 74.0 | ||
| % ≥75-90 mg/dL | 36 | ||
| % ≥100-130 mg/dL | 17 | ||
|
| |||
Weight status was classified using the International Obesity Task Force international age- and sex-specific BMI cut-points; which correspond to an adult BMI of 18.5 (underweight), 25 (overweight) or 30 (obesity). For blood pressure, age- and gender-specific BP reference standards for Chinese children were used to define pre-hypertension (>90th percentile of SBP, DBP or both) and hypertension (>95% percentile of SBP, DBP or both)16. For impaired glucose metabolism, criteria defined by the American Diabetes Association was used for increased risk of diabetes (fasting glucose ≥100mg/dL and HbA1c ≥5.7%)17. For dyslipidemia, pediatric-specific cutoff values were defined by the National Cholesterol Education Program (NCEP) Expert Panel on Cholesterol Levels in Children: borderline values TC≥170 mg/dL, LDL≥110 mg/dL, HDL≤45 mg/dL, TAG≥75 mg/dL for 0-9y and ≥90 mg/dL for 10-19y; high values TC≥200 mg/dL, LDL≥130 mg/dL, HDL<35 mg/dL, TAG≥100 mg/dL for 0-9y and ≥130 mg/dL for 10-19y18,19. Pre-dyslipidemia was defined as having at least one marker above borderline cutoff values, whereas dyslipidemia was defined as having at least one marker above high cutoff values.
Figure 1. Prevalence (%) of cardiometabolic risk factors by area of residence and income among children 7-12 y who participated in the China Health and Nutrition Survey in 2009.
Ow/Ob: overweight/obesity; PreHTN: pre-hypertension; HTN: hypertension; ImpGLU: impaired glucose/HbA1c; PreDYSLIP: pre-dyslipidemia; DYSLIP: dyslipidemia.
* Significantly different between urban vs. rural; or between lower vs. middle or higher income, Student’s t test, p<0.05.
Nutrient intakes and dietary adequacy
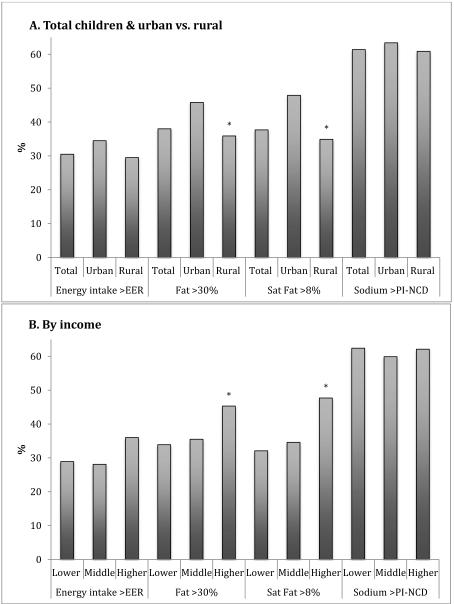
Total daily energy and nutrient intakes are presented in Table 2. Intake of energy most macro- and micronutrients was significantly higher among urban compared to rural children and among children from higher income compared to lower income households (p<0.05). Approximately 30% of all children had energy intakes above estimated energy requirements and around 38% of them had % total fat and % saturated fat above established AMDR ranges (Figure 2, Additional table 2). More than 60% of the studied children had sodium intakes above Chinese Proposed Intake cut-points.
Table 2.
Daily intake of energy (kcal), macro- (g) and micronutrients (mg) by area of residence and income among children 7-12 y (CHNS 2009).
|
Total children
n=658 |
Urban
n=142 |
Rural
n=516 |
||||
|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Mean | SE | |
| Energy (kcal/d) | 1540 | 18.7 | 1624 | 46.7 | 1517 | 20.0 * |
| Macronutrients (g/d) | ||||||
| Protein | 50.8 | 0.77 | 56.8 | 2.00 | 49.1 | 0.80 * |
| Carbohydrates | 228 | 2.87 | 225 | 6.53 | 229 | 3.20 |
| Total sugars | 20.7 | 0.71 | 25.1 | 1.60 | 19.5 | 0.78 * |
| Added sugars | 7.37 | 0.41 | 8.83 | 0.79 | 6.97 | 0.48 |
| Total Fat | 47.3 | 1.13 | 55.3 | 2.46 | 45.1 | 1.26 * |
| Saturated fat | 12.4 | 0.30 | 14.8 | 0.62 | 11.8 | 0.33 * |
| Monounsaturated fat | 18.8 | 0.49 | 22.0 | 1.05 | 18.0 | 0.56 * |
| Polyunsaturated fat | 12.5 | 0.33 | 14.5 | 0.74 | 12.0 | 0.37 * |
| Micronutrients (mg/d) | ||||||
| Sodium | 2540 | 86.9 | 2902 | 240 | 2440 | 88.6 * |
| Potassium | 1274 | 25.9 | 1353 | 49.4 | 1252 | 30.0 |
|
| ||||||
|
Lower income
n=218 |
Middle income
n=217 |
Higher income
n=214 |
||||
| Mean | SE | Mean | SE | Mean | SE | |
|
| ||||||
| Energy (kcal/d) | 1509 | 29.6 | 1486 | 31.9 | 1636 | 35.6 * |
| Macronutrients (g/d) | ||||||
| Protein | 47.1 | 1.05 | 50.0 | 1.31 | 55.8 | 1.58 * |
| Carbohydrates | 231 | 4.96 | 222 | 4.97 | 231 | 5.14 |
| Total sugars | 17.5 | 1.03 | 18.9 | 1.09 | 26.3 | 1.47 * |
| Added sugars | 6.91 | 0.67 | 6.02 | 0.59 | 9.31 | 0.88 * |
| Total Fat | 43.8 | 1.78 | 44.2 | 1.92 | 54.5 | 2.16 * |
| Saturated fat | 11.3 | 0.43 | 11.5 | 0.52 | 14.7 | 0.58 * |
| Monounsaturated fat | 17.8 | 0.80 | 17.7 | 0.88 | 21.3 | 0.90 * |
| Polyunsaturated fat | 12.2 | 0.58 | 11.6 | 0.53 | 14.0 | 0.62 * |
| Micronutrients (mg/d) | ||||||
| Sodium | 2592 | 154 | 2347 | 135 | 2693 | 165 |
| Potassium | 1142 | 28.2 | 1281 | 47.2 | 1417 | 54.8 * |
Estimates presented as mean ± SE.
Significantly different between urban vs. rural; or between lower vs. middle or higher income, Student’s t test, p<0.05.
Figure 2. Prevalence (%) of excessive intakes of energy, total fat, saturated fat and sodium by area of residence and income among children 7-12 y who participated in the China Health and Nutrition Survey 2009.
Estimates presented as %. Excessive intakes were calculated using EER for energy, AMDR for total fat and saturated fat, and Chinese Proposed Intakes (PI-NCD) for sodium; 2014 Dietary Reference Intakes for the Chinese Population.
* Significantly different between urban vs. rural; or between lower vs. middle or higher income, Student’s t test, p<0.05.
Significant differences were found in the prevalence of excessive intakes between children from urban vs. rural areas and from higher vs. lower income households regarding percentage of carbohydrate, total fat and saturated fat intakes (Additional table 2) (p<0.05). The prevalence of inadequate intakes of protein, carbohydrates and fat was significantly higher among children from rural vs. urban areas and lower vs. higher income households (p<0.05).
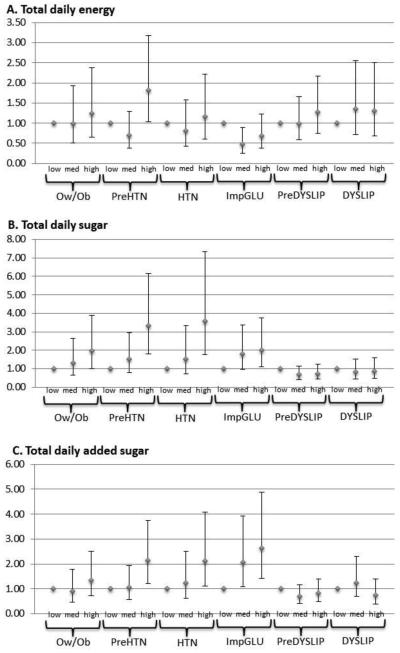
Dietary correlates of adverse cardiometabolic risk
Logistic regression analyses were adjusted by gender, age, physical activity, area of residence and income to compare the odds (OR, 95%CI) of having a CM risk factor in those who had a higher vs. middle or lower intakes of energy and selected macro- and micronutrients (Figure 3, Additional table 3). Higher intakes of total daily energy, total and added sugars were associated with an increased likelihood of having prehypertension. Higher intakes of total and added sugars were also associated with higher odds of having hypertension and impaired glucose/HbA1c. The associations found between polyunsaturated fat and prehypertension; and total sugar and overweight and obesity were non-significant after further adjustment for total daily energy intake, suggesting a potential mediating effect of energy intake on those outcomes. Those in the middle tertile of intake of total daily energy, saturated and monounsaturated fat had a lower likelihood of having impaired glucose/HbA1c, while those with medium intakes of protein had lower odds of having pre hypertension and hypertension.
Figure 3. Logistic regression models of CM risk factors as outcomes: odds ratios (95%CI) for the associations with daily nutrient intakes among children 7-12 years, 2009 CHNS.
* Odds Ratios from logistic regression models, adjusted by gender, age, physical activity, area of residence and income. Nutrient intakes modeled as tertiles (low, medium and high intake).
**Ow/Ob: overweight/obesity; PreHTN: pre-hypertension; HTN: hypertension; ImpGLU: impaired glucose/HbA1c; PreDYSLIP: pre-dyslipidemia; DYSLIP: dyslipidemia.
In supplemental analyses mean intakes and dietary adequacy of total daily energy and selected macro- and micronutrients are reported among children with overweight/obesity (Additional table 4) and those with impaired blood pressure, glucose and lipid markers compared to those without the condition (Additional table 5). Mean intake of total sugar and added sugars was significantly higher among overweight/obese children compared to normal weight, and among children with impaired glucose/HbA1c compared with those with normal values (p<0.05). Children with prehypertension had higher values of total daily energy and most macro- and micronutrients compared to those with normal blood pressure (p<0.05).
DISCUSSION
This research focused on obesity and CM risk factors in association with energy and macro- and micronutrients among Chinese school-age children. Firstly, high prevalences were found for the selected CM risk factors in our sample of children 7-12-y old. Approximately 14% of children had overweight/obesity or hypertension; 26% had impaired glucose/HbA1c and 21% had dyslipidemia. More than half of the sample had at least one lipid value exceeding the established borderline cutoffs. Among children from urban areas and higher income households, the prevalence of some of these risk factors was even higher. Several dietary factors such as sugars were found as important correlates of CM risk in our sample of Chinese school-age children.
Children and adolescents 2-18-y old in China have experienced a steady increase in overweight and obesity since 19911,3,4 with the younger cohorts examined in this study representing a major upward shift in weight and BMI from earlier cohorts.25 In 2011, the prevalence of overweight and obesity was 19% among children 7-12-y old %, and was approximately 27% among those from urban areas (unreported results). Furthermore, it has been observed that younger generations are becoming adults with higher BMIs than earlier generations. For example, at age 10, the average BMI was 3 units higher in 2009 than in 1991.1,4 Remarkably, in 2006, 6–10-y old children at the 95th centile had a BMI of 25, which was comparable to older children and adolescents. At age 6, the mean BMI at the 95th centile was 2.6 units higher compared to US children, suggesting that the Chinese pediatric population could become soon one of the heaviest across the globe.25
These increases in weight are consistent with the observed elevated prevalence of CM risk factors in Chinese children and adolescents over the same time period.4,9,11,12,26 At least 42% of children and adolescents 7-18-y old had one or more CM risk factors in 2009. The prevalence of pre-diabetes as measured by impaired HbA1c was 15% among 7-18-y-olds,4 whereas ~20% of 7-12-y-olds in our sample had impaired HbA1c, suggesting that the risk of diabetes might be even higher among younger children compared to adolescents. The rates of diabetes (HbA1c ≥6.5%) and inflammation (CRP ≥3 mg/dL) were higher in the CHNS adolescent population compared to adolescents from the U.S. or other Asian countries.4 In the context of the dramatic economic and environmental changes in China, these larger increases in weight and CM risk factors among younger children suggest that newer generations might be experiencing more profound health consequences than adolescent generations. Since children at the upper end of the distribution are heavier than ever before and given the higher risk of NCDs at lower BMIs among Asians,27 it is important to act rapidly in order to improve the future health status of Chinese children.
These patterns of increased overweight and CM risk factors among Chinese children have shown critical disparities by area of residence and income as seen before.3,28 Although we found overall higher prevalences among children from urban areas and higher income households, the proportion of rural and lower income children presenting overweight, obesity and CM risk factors was still high. This is consistent with previous studies that reported higher prevalence of overweight/obesity among children from urban areas and higher income households,2,3,29 and also with others that showed rapid increases in overweight and CM risk in less urban areas and across all income levels.2,4 As economic development reaches a broader area, even rural or less developed populations will be exposed to more obesogenic environments,30 which may contribute to the shifting burden of NCDs from the rich to the poor across China.2,31
This study showed important associations with dietary factors that portend significant implications for NCDs. About one in three children had daily energy intakes above requirements and ~50% of those from urban areas and higher income households had excessive intakes of fat and saturated fat. These findings are consistent with the observed changes in child dietary habits over the past two decades in China.5 Traditional dietary patterns and cooking methods have been shifting towards increased intakes of fried food, animal-sourced foods, snacks and away-from-home meals.6-8,31 Higher incomes and lower prices of edible oils and animal foods have contributed to these new patterns in China.32,33
Children with higher intakes of energy and sugars had a greater likelihood of having impaired blood pressure and glucose/HbA1c. The relationship between sugar and hypertension has recently been emphasized in a meta-analysis of RCTs that found a positive association with sugar-sweetened beverages (SSBs).34 Sugar might increase blood pressure through weight change but also through its association with salt intake and processed foods.26,35 In addition, high sugar intake could potentially trigger a brain response that increases heart rate and blood pressure, although other plausible mechanisms include decreased sodium excretion and impaired renin-angiotensin system.36-38 Although no association with sodium or potassium among Chinese children was found in the current study, Du and colleagues have shown that sodium intake and the sodium-potassium ratio was associated with hypertension in Chinese adults.39 These results still have implications for intervention because more than 60% of children in this sample had mean sodium intakes above the Chinese Proposed Intakes, which is set as a dietary goal for disease prevention. In contrast, consistent with a nutrient-balanced diet, normal intakes of total daily energy, protein and saturated and monounsaturated fat (as represented by the middle tertile) were associated in this study with lower likelihood of presenting some of these CM risks. This research generally showed a more critical role of total and added sugars on CM risk. In the context of a decreasing trend in sodium intake in China,39 individuals might be turning to high sugar and/or high fat diets,6,40 so “Westernized” dietary patterns rich in processed foods, SSBs and snacks coupled with sedentary lifestyles may be responsible for the higher risk of obesity and NCDs.41,42
The present work used the CHNS, a unique household-based cohort with a wide variability in urbanization, economic development and health indicators across China.13,14 Its main advantages are the availability of SES, nutrient intake and health data for an important sample of children in China. However, a limitation of the CHNS is the lack of survey weights to obtain nationally representative results, even though the CHNS captures different demographic and geographical areas, including urban and rural communities and neighborhoods.14 The study design is cross-sectional so causal inference is limited. In addition, health data (blood pressure and biomarkers) was missing for a small proportion of the sample and was completely unavailable for children ≤6-y, which is an important group to understand the burden of pediatric obesity and NCDs in China. Also, although dietary measurement in the CHNS was time consuming, expensive, and required trained field workers; these efforts were found to be positive because the combination of 24-hr recalls and detailed household food inventory improved the quality of individual dietary data compared to a single 24-hr recall.43-46 However, self-reported dietary intake and physical activity measurements might still be affected by measurement error. Another limitation was the overall small power to detect significant associations with dietary factors, although the sample size was generally adequate to address the rest of the hypotheses. Additional stratification by SES might have reduced representativeness and generalizability of the study results, especially for the estimates of prevalence of rare outcomes. Nevertheless, the changes in the economical, social and health landscape captured by the CHNS are instrumental to investigate recent dynamics in childhood nutrition and health status.
The high prevalence of overweight and CM risk factors anticipate an increased morbidity and mortality from NCDs over the next decades in China.9,32 Childhood overweight and CM risk is highly prevalent in urban and rural areas and across different SES groups in China although disparities between classes still pervade. In parallel, several dietary inadequacies exist, including excess energy intake and total and saturated fat. Total energy and sugar intakes were significant correlates of prehypertension and pre-diabetes. In conclusion, as China undergoes a nutrition transition, the health landscape is progressively shifting from underweight and stunting towards overweight and NCDs. These results present important implications for dietary interventions and target SES groups that might benefit the most from them. In the context of the increasing burden of pediatric obesity and NCDs, China must intervene rapidly in order to decrease and reverse these major public health concerns.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to thank Dr. Phil Bardsley for programming assistance; Dr. Alison L. Eldridge for helpful revision, and Ms. Frances L. Dancy for administrative assistance.
FUNDING DISCLOSURE:
Funding for this work was provided by the Nestlé Research Center, Lausanne, Switzerland.
ABBREVIATIONS
- AMDR
Acceptable Macronutrient Distribution Ranges
- CHNS
China Health and Nutrition Survey
- CM
Cardiometabolic risk
- DBP
Diastolic blood pressure
- EAR
Estimated Average Requirements
- EER
Estimated Energy Requirements
- FCT
Food composition table
- HbA1c
Hemoglobin A1c
- MET
total metabolic equivalents
- NCD
Non-communicable disease
- PA
Physical activity
- PI-NCD
Proposed intakes for Preventing Non-communicable Diseases
- SES
Socio-economic status
- SBP
Systolic blood pressure
- TC
Total cholesterol
- TG
triglycerides
Footnotes
AUTHOR CONTRIBUTIONS
C.P., D.W., and B.M.P. designed research; C.P., D.W., S.D., B.Z., Z.W., C.S. and B.M.P. conducted research; C.P. analyzed data; C.P., D.W., and B.M.P. wrote the paper; C.P., D.W., S.D., B.Z., Z.W., C.S. and B.M.P. had primary responsibility for final content. All authors have read and approved the final manuscript.
CONFLICT OF INTERESTS
The authors declare that they have no competing interests.
REFERENCES
- 1.Gordon-Larsen P, Wang H, Popkin BM. Overweight dynamics in Chinese children and adults. Obes Rev. 2014:37–48. doi: 10.1111/obr.12121. doi: 10.1111/obr.12121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dearth-Wesley T, Wang H, Popkin BM. Under- and overnutrition dynamics in Chinese children and adults (1991-2004) Eur J Clin Nutr. 2008;11:1302–7. doi: 10.1038/sj.ejcn.1602853. doi: 10.1038/sj.ejcn.1602853. [DOI] [PubMed] [Google Scholar]
- 3.Liang YJ, Xi B, Song AQ, Liu JX, Mi J. Trends in general and abdominal obesity among Chinese children and adolescents 1993-2009. Pediatr Obes. 2012;5:355–64. doi: 10.1111/j.2047-6310.2012.00066.x. doi: 10.1111/j.2047-6310.2012.00066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yan S, Li J, Li S, Zhang B, Du S, Gordon-Larsen P, Adair L, Popkin B. The expanding burden of cardiometabolic risk in China: the China Health and Nutrition Survey. Obes Rev. 2012;9:810–21. doi: 10.1111/j.1467-789X.2012.01016.x. doi: 10.1111/j.1467-789X.2012.01016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cui Z, Dibley MJ. Trends in dietary energy, fat, carbohydrate and protein intake in Chinese children and adolescents from 1991 to 2009. Br J Nutr. 2012;7:1292–9. doi: 10.1017/S0007114511006891. doi: 10.1017/S0007114511006891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhai FY, Du SF, Wang ZH, Zhang JG, Du WW, Popkin BM. Dynamics of the Chinese diet and the role of urbanicity, 1991-2011. Obes Rev. 2014:16–26. doi: 10.1111/obr.12124. doi: 10.1111/obr.12124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Z, Zhai F, Du S, Popkin B. Dynamic shifts in Chinese eating behaviors. Asia Pac J Clin Nutr. 2008;1:123–30. [PubMed] [Google Scholar]
- 8.Wang Z, Zhai F, Zhang B, Popkin BM. Trends in Chinese snacking behaviors and patterns and the social-demographic role between 1991 and 2009. Asia Pac J Clin Nutr. 2012;2:253. [PMC free article] [PubMed] [Google Scholar]
- 9.Adair LS, Gordon-Larsen P, Du SF, Zhang B, Popkin BM. The emergence of cardiometabolic disease risk in Chinese children and adults: consequences of changes in diet, physical activity and obesity. Obes Rev. 2014:49–59. doi: 10.1111/obr.12123. doi: 10.1111/obr.12123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, Shan Z, Liu J, Tian H, Ji Q. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;12:1090–101. doi: 10.1056/NEJMoa0908292. doi: 10.1056/NEJMoa0908292. [DOI] [PubMed] [Google Scholar]
- 11.Lee CG. The emerging epidemic of hypertension in asian children and adolescents. Curr Hypertens Rep. 2014;12:495. doi: 10.1007/s11906-014-0495-z. doi: 10.1007/s11906-014-0495-z. [DOI] [PubMed] [Google Scholar]
- 12.Liang YJ, Xi B, Hu YH, Wang C, Liu JT, Yan YK, Xu T, Wang RQ. Trends in blood pressure and hypertension among Chinese children and adolescents: China Health and Nutrition Surveys 1991-2004. Blood Press. 2011;1:45–53. doi: 10.3109/08037051.2010.524085. doi: 10.3109/08037051.2010.524085. [DOI] [PubMed] [Google Scholar]
- 13.Zhang B, Zhai FY, Du SF, Popkin BM. The China Health and Nutrition Survey, 1989-2011. Obes Rev. 2014:2–7. doi: 10.1111/obr.12119. doi: 10.1111/obr.12119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Popkin BM, Du S, Zhai F, Zhang B. Cohort Profile: The China Health and Nutrition Survey--monitoring and understanding socio-economic and health change in China, 1989-2011. Int J Epidemiol. 2010;6:1435–40. doi: 10.1093/ije/dyp322. doi: 10.1093/ije/dyp322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cole T, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012;4:284–94. doi: 10.1111/j.2047-6310.2012.00064.x. doi: 10.1111/j.2047-6310.2012.00064.x. [DOI] [PubMed] [Google Scholar]
- 16.Mi J, Wang T-y, Meng L-h, Zhu G-j, Han S-m, Zhong Y, Liu G, Wan Y, Xiong F, Shi J. Development of blood pressure reference standards for Chinese children. Chin J Evid Based Pediatr. 2010;1:4–14. [Google Scholar]
- 17.American Diabetes A Standards of medical care in diabetes--2014. Diabetes Care. 2014:S14–S80. doi: 10.2337/dc14-S014. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 18.Lauer R, Barness L, Clark R, Deckelbaum R, Finberg L, Kwiterovich P, McBride PE, Schieken RM, Scott LW, Strong JP. National Cholesterol Education-Program (NCEP)-highlights of the report of the expert panel on blood cholesterol levels in children and adolescents. Am Acad Pediatrics. 1992 [PubMed] [Google Scholar]
- 19.Kwiterovich PO., Jr Recognition and management of dyslipidemia in children and adolescents. J Clin Endocrinol Metab. 2008;11:4200–9. doi: 10.1210/jc.2008-1270. doi: 10.1210/jc.2008-1270. [DOI] [PubMed] [Google Scholar]
- 20.Yang Y, Wang G, Pan X. China food composition 2002. Peking University Medical Press; Beijing: 2002. p. 136. [Google Scholar]
- 21.US Department of Agriculture ARS USDA National Nutrient Database for Standard Reference: Release 27: USDA-ARS Washington. 2014 [Google Scholar]
- 22.Society CN. Chinese Dietary Reference Intakes (version 2013) Science Press; Beijing: 2014. [Google Scholar]
- 23.Tudor-Locke C, Ainsworth B, Adair L, Du S, Popkin B. Physical activity and inactivity in Chinese school-aged youth: the China Health and Nutrition Survey. Intl J Obes. 2003;9:1093–99. doi: 10.1038/sj.ijo.0802377. [DOI] [PubMed] [Google Scholar]
- 24.Murphy SP, Guenther PM, Kretsch MJ. Using the dietary reference intakes to assess intakes of groups: pitfalls to avoid. J Am Diet Assoc. 2006;10:1550–53. doi: 10.1016/j.jada.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 25.Popkin BM. Recent dynamics suggest selected countries catching up to US obesity. The Am J Clin Nutr. 2010;1:284S–288S. doi: 10.3945/ajcn.2009.28473C. doi: 10.3945/ajcn.2009.28473C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dong B, Ma J, Wang HJ, Wang ZQ. The association of overweight and obesity with blood pressure among Chinese children and adolescents. Biomed Environ Sci. 2013;6:437–44. doi: 10.3967/0895-3988.2013.06.004. doi: 10.3967/0895-3988.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 27.WHO EC Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;9403:157. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 28.Wagner K-H, Brath H. A global view on the development of non communicable diseases. Prev Med. 2012:S38–S41. doi: 10.1016/j.ypmed.2011.11.012. doi: 10.1016/j.ypmed.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 29.Wang X, Hojer B, Guo S, Luo S, Zhou W, Wang Y. Stunting and 'overweight' in the WHO Child Growth Standards - malnutrition among children in a poor area of China. Public Health Nutr. 2009;11:1991–8. doi: 10.1017/S1368980009990796. doi: 10.1017/S1368980009990796. [DOI] [PubMed] [Google Scholar]
- 30.Monteiro CA, Conde WL, Lu B, Popkin BM. Obesity and inequities in health in the developing world. Intl J Obes. 2004;9:1181–6. doi: 10.1038/sj.ijo.0802716. [DOI] [PubMed] [Google Scholar]
- 31.Du S, Mroz TA, Zhai F, Popkin BM. Rapid income growth adversely affects diet quality in China—particularly for the poor! Soc Sci Med. 2004;7:1505–15. doi: 10.1016/j.socscimed.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 32.Popkin BM, Du S. Dynamics of the nutrition transition toward the animal foods sector in China and its implications: a worried perspective. J Nutr. 2003;11:3898S–3906S. doi: 10.1093/jn/133.11.3898S. [DOI] [PubMed] [Google Scholar]
- 33.Ng SW, Zhai F, Popkin BM. Impacts of China's edible oil pricing policy on nutrition. Soc Sci Med. 2008;2:414–26. doi: 10.1016/j.socscimed.2007.09.015. doi: http://dx.doi.org/10.1016/j.socscimed.2007.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Malik AH, Akram Y, Shetty S, Malik SS, Yanchou Njike V. Impact of sugar-sweetened beverages on blood pressure. Am J cardiology. 2014;9:1574–80. doi: 10.1016/j.amjcard.2014.01.437. doi: 10.1016/j.amjcard.2014.01.437. [DOI] [PubMed] [Google Scholar]
- 35.DiNicolantonio JJ, O'Keefe JH, Lucan SC. An unsavory truth: sugar, more than salt, predisposes to hypertension and chronic disease. Am J Cardiol. 2014;114 doi: 10.1016/j.amjcard.2014.07.002. doi: 10.1016/j.amjcard.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 36.Rebello T, Hodges RE, Smith JL. Short-term effects of various sugars on antinatriuresis and blood pressure changes in normotensive young men. Am J Clin Nutr. 1983;1:84–94. doi: 10.1093/ajcn/38.1.84. [DOI] [PubMed] [Google Scholar]
- 37.Rowe JW, Young JB, Minaker KL, Stevens AL, Pallotta J, Landsberg L. Effect of insulin and glucose infusions on sympathetic nervous system activity in normal man. Diabetes. 1981;3:219–25. doi: 10.2337/diab.30.3.219. [DOI] [PubMed] [Google Scholar]
- 38.Johnson RJ, Segal MS, Sautin Y, Nakagawa T, Feig DI, Kang D-H, Gersch MS, Benner S, Sánchez-Lozada LG. Potential role of sugar (fructose) in the epidemic of hypertension, obesity and the metabolic syndrome, diabetes, kidney disease, and cardiovascular disease. An J Clin Nutr. 2007;4:899–906. doi: 10.1093/ajcn/86.4.899. [DOI] [PubMed] [Google Scholar]
- 39.Du S, Batis C, Wang H, Zhang B, Zhang J, Popkin BM. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am J Clin Nutr. 2014;2:334–43. doi: 10.3945/ajcn.113.059121. doi: 10.3945/ajcn.113.059121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Batis C, Sotres-Alvarez D, Gordon-Larsen P, Mendez MA, Adair L, Popkin B. Longitudinal analysis of dietary patterns in Chinese adults from 1991 to 2009. Br J Nutr. 2014;08:1441–51. doi: 10.1017/S0007114513003917. doi: 10.1017/S0007114513003917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Drewnowski A. The real contribution of added sugars and fats to obesity. Epidemiol Rev. 2007;1:160–71. doi: 10.1093/epirev/mxm011. [DOI] [PubMed] [Google Scholar]
- 42.Ng SW, Howard AG, Wang H, Su C, Zhang B. The physical activity transition among adults in China: 1991–2011. Obes Rev. 2014;S1:27–36. doi: 10.1111/obr.12127. doi: 10.1111/obr.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhai F, Guo X, Popkin BM, Ma L, Wang Q, Yu W, Jin S, Ge K. Evaluation of the 24-hour individual recall method in China. Food Nutr Bull. 1996:154–61. doi: [Google Scholar]
- 44.Popkin BM, Lu B, Zhai F. Understanding the nutrition transition: measuring rapid dietary changes in transitional countries. Public Health Nutr. 2002;5:947–53. doi: 10.1079/PHN2002370. [DOI] [PubMed] [Google Scholar]
- 45.Du S, Batis C, Wang H, Zhang B, Zhang J, Popkin BM. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am J Clin Nutr. 2014;2:334–43. doi: 10.3945/ajcn.113.059121. doi: 10.3945/ajcn.113.059121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.He K, Du S, Xun P, Sharma S, Wang H, Zhai F, Popkin B. Consumption of monosodium glutamate in relation to incidence of overweight in Chinese adults: China Health and Nutrition Survey (CHNS) Am J Clin Nutr. 2011;6:1328–36. doi: 10.3945/ajcn.110.008870. doi: 10.3945/ajcn.110.008870. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.