Abstract
Background:
Social media have been used to study many aspects of health and human behavior. Although social media present a unique opportunity to obtain unsolicited patient-reported outcomes, its use has been limited in plastic and reconstructive surgical procedures, including migraine nerve surgery. The goal of this study was to utilize the most popular social media site, Facebook, to evaluate patients’ experience with migraine surgery.
Methods:
Six months of data regarding nerve surgery, nerve stimulators, and radiofrequency nerve ablation were collected from posts and comments written by members of 2 Facebook groups. Outcomes were classified by degree of resolution of symptoms.
Results:
A total of 639 posts related to migraine surgery. Of 304 posts commenting on postoperative success of nerve surgery, 16% reported elimination of headaches and 65% significant improvement (81% with complete or significant improvement), 5% partial improvement, 11% no change, and 3% worsening symptoms. Nerve surgery had a higher success rate than nerve stimulators and radiofrequency ablation. Nerve surgery was recommended by 90% of users.
Conclusions:
The 81% rate of complete or significant improvement of symptoms in this study is close to the 79% to 84% shown in current literature. Similar to the findings of a recent systematic review, surgery is more efficacious compared with nerve stimulators and ablation. This study adds to evidence favoring migraine surgery by removing evaluator bias and demonstrates that surgical outcomes and satisfaction data may be obtained from social media.
Since the first article on migraine nerve surgery published in 2000, several centers have reported their results through retrospective and prospective studies, including the seminal randomized controlled trial published by Guyuron et al1–7 in 2009. A recent review looking at the collective literature found that the success rate of migraine surgery ranges from 68% to 95%.8 Despite the consistent results obtained by authors in different centers in the United States and Europe, nerve decompression for the treatment of chronic headaches is still often met with skepticism. Two of the most common critiques are that the positive results are attributable to placebo effect of the intervention and that the results in each of the outcome studies were evaluated and reported by the treating plastic surgeon.9, 10 Although almost all the studies measured outcomes by either migraine diaries or migraine questionnaires, both completed by the patient and not the surgeon, it will be useful to evaluate results as patients report them outside their surgeon’s office. Evaluating patient perceptions outside the clinical environment may shed additional light on an ongoing debate of the ways by which this intervention helps patients.
In the senior author’s (AMA) migraine surgery practice, we noticed that patients’ decisions to pursue surgical treatment are often influenced by information the patient gathers through social media, particularly Facebook support groups. This is not surprising, as 95% of patients turn to the Internet for surgical information before pursuing plastic surgery, and 23% of patients with chronic medical problems seek online support from other Facebook users with similar conditions.11,12
Facebook has been used to study many aspects of health care and provides a convenient, easily accessible way to collect unsolicited, observational patient data.13–15 The use of Facebook to study surgical outcomes has been limited and Facebook has not yet been used to evaluate migraine surgery.16 This study aimed to (1) determine the feasibility of using social media to evaluate surgical outcomes, (2) evaluate, using Facebook posts and comments, patient-reported outcomes after migraine surgery, particularly in comparison to other nonmedical treatments (implantable nerve stimulators and radiofrequency nerve ablation), and (3) review patient recommendations and advice to their peers about their experience with migraine surgery.
METHODS
Background and Data Collection
Institutional Review Board exemption was granted prior to data collection. Data were collected from social network groups within the social media site, Facebook (http://www.facebook.com). Online activity that was posted between October 2014 and March 2015 was reviewed. Using the “search” feature on Facebook’s Web site, the terms “migraine surgery” and “occipital neuralgia” were used to find relevant Facebook groups. A group was determined to be active if it had more than 50 posts in the last 30 days, and the top 2 active groups were selected. Two “closed” groups (eg, a Facebook member needed to “join” the group before participating in group features) were selected.
Two trained researchers with previous experience in coding data from social media performed data analysis. To achieve interrater reliability, 10% of data (3 weeks) were identified and coded by both researchers. A Cohen’s κ coefficient for interrater reliability for the subset of data was 0.78. Researchers did not create any posts or comments, and no attempt was made to contact members of the Facebook groups or to view individual profiles.
Data Analysis
We utilized content analysis to qualitatively assess online activity. After a preliminary review of the data collected from each post and comment, a code book was developed to formally categorize posts and comments as they related to migraine surgery.17 This was performed using a spreadsheet and by organizing recurring topics and themes into codes, subcodes, and broad categories. Terms that were used to identify posts and comments are shown in Table 1. Comments that were made in response to posts about surgery were coded if they commented on recovery or outcomes from surgery, or provided surgical advice. For example, “I had 100% relief!” in response to a post inquiring about migraine surgery was coded even though it did not contain a code term. Emotional posts that did not contain information about recovery, outcomes, or advice, such as “Good luck with your surgery!” were not included. Any posts or comments that might have been made by a health care professional were excluded from this study. Coded posts and comments were organized in a secure spreadsheet. All data were deidentified. Posts included as examples in this manuscript have been altered from their original wording to protect the identities of group members.
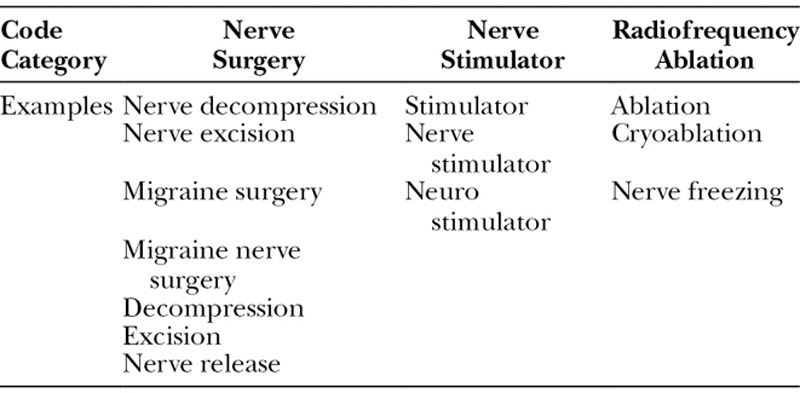
Table 1.
Examples from Code Book Developed to Identify Terms Related to the 3 Surgical Treatments of Migraine Headaches When Collecting Data from Facebook Posts
Variables
Demographic data were limited to subjective identification of the sex of the Facebook member creating the coded post, based on name and profile picture. Facebook profiles were not accessed, and no additional demographic data were collected. Posts were categorized by type of procedure: nerve surgery, nerve stimulator, nerve radiofrequency ablation, or other surgical procedure. Data regarding the patient-reported success of surgery were grouped into 6 categories:
1) Reporting elimination of headaches, 100% relief, no longer having headaches;
2) Reporting relief of headaches, general comments about helping or changing life, or improvement of symptoms or need for fewer medications without specifying amount of relief;
3) Reporting improvement >50%, helping “a lot,” or much relief;
4) Reporting improvement <50%, helping “a little,” or some relief;
5) Reporting no change; and
6) Reporting worsening of symptoms.
As most of the previous articles on migraine surgery used a 50% improvement as the cutoff point for surgical success, we similarly defined “success” as categories 1 to 3. The second data point collected was recommendations for or against surgery that were provided by patients. These were coded as either “recommend surgery” or “do not recommend surgery.” For the third end point, posts were identified that gave advice related to surgery. Miscellaneous additional coded data included complications, insurance coverage, and shared information or advice about recovery from surgery.
Statistical Analysis
Data were analyzed using frequency calculations, for which confidence intervals were included. Chi-square tests were performed to evaluate relationships between responses, and a P value of ≤0.05 was considered statistically significant. Statistical analysis was performed using SPSS software (SPSS Inc., Chicago, Ill.).
RESULTS
Six months of data were gathered from 2 Facebook groups. Group A comprised more than 2,000 members, whereas group B contained over 500 members. A total of 639 data points (posts and comments) was collected. Of these data points, 120 were posts that initiated a discussion, and 519 were comments that replied to existing posts. A total of 261 data points were collected from group A and 378 from group B. Female group members contributed to the majority of data points (94%).
All posts and comments were categorized by type of surgical management that was referenced. Nerve surgery was referenced in 534 data points (84%), nerve radiofrequency ablation in 78 (12%), nerve stimulator in 26 (4%), and other surgical procedure in 3 (0.5%)
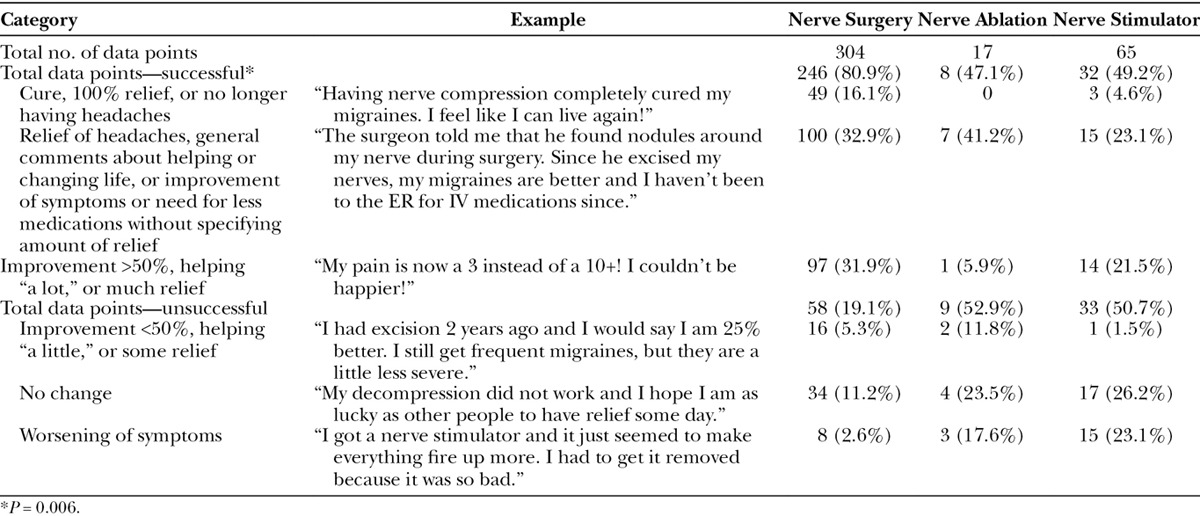
Data points that specifically referenced “outcome” were coded according to the above classification system for success rate to fulfill the second aim of the study. A total of 386 comments and posts referenced surgical success, with the majority referencing nerve surgery. Overall, 81% of nerve surgery posts were coded as a surgical success (elimination of headaches, >50% improvement, or improvement) compared with 47% of nerve stimulator and 49% of nerve ablation (P = 0.006; Fig. 1). Examples of data points referencing surgical success and rates of success for each surgical procedure are included in Table 2.
Fig. 1.
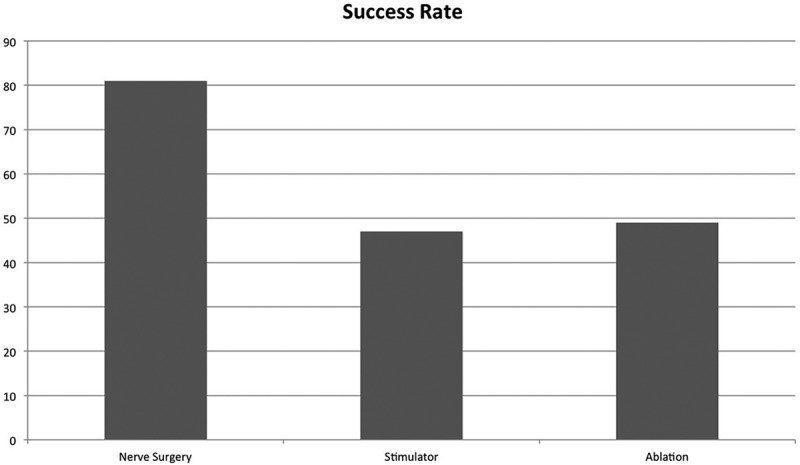
Patient-reported success rates of 3 surgical procedures, as defined by >50% resolution of symptoms.
Table 2.
Surgical Success Rates by Surgical Procedure
The third aim of the study was to observe recommendations for surgery by patients. We evaluated comments that favorably discussed and, in some cases, recommended migraine surgery. Thirty-nine data points referenced recommendations about nerve surgery. An example of a post “for” surgery is “I would recommend nerve surgery to everyone, mine went great!” in contrast to “If I could do it again, I would not have had surgery. I wouldn’t recommend going through it.” Nerve surgery was recommended by 90% of these types of posts. Nerve stimulator was recommended in 1 data point and not recommended in 1 data point. Nerve ablation was recommended in 3 data points and not recommended in 3 data points.
In post hoc analysis, a number of data points were identified as either requesting advice for making decisions related to surgery or giving advice. Data points regarding advice include “What kind of surgery would be best for my symptoms?” or “I really think that you should ask about nerve excision instead of nerve decompression surgery.” A total of 95 posts (15% of total data points) were related to surgical advice, including decisions about which type of surgery to pursue and which surgeon to seek out.
Additionally, 112 data points (18% of posts) referenced the postoperative period and recovery from nerve surgery. Examples include “Make sure you sleep in a chair for a couple nights after surgery, it will really help with the swelling!” or “(After surgery) I would recommend decreasing 1 medication at a time over the first month.” A small number of data points (25 posts, 4% of total posts) referenced questions or advice about insurance coverage of migraine surgery.
Complications of surgical procedures were referenced in 43 data points (7% of posts). The most frequently reported complications of nerve surgery were numbness, itching, and need for further surgery. Two complications (8%) were reported for nerve stimulator and 6 (8%) for nerve ablation.
DISCUSSION
This study found that a significant amount of data regarding patient experience, perception, and outcomes can be collected from social media sites such as Facebook. Eighty-one percent of posts considered nerve surgery to be “successful,” compared with 47% and 49% of posts reporting success of nerve stimulator and radiofrequency ablation, respectively. To our knowledge, this is the first study in plastic surgery evaluating outcomes using the world’s most popular social media site. In addition, this study evaluated outcomes for the often-debated migraine nerve surgery as reported by the patients themselves in an environment outside their treating physicians’ offices, thereby decreasing physician bias and the possibility that patients are reporting better outcomes in clinic so as not to disappoint their surgeons.
When compared with current available literature about migraine surgery, we were surprised about the marked resemblance between the patient-reported outcomes observed in this study and the results reported in the literature. Our data suggest an 81% success rate of nerve surgery. Several of the largest series evaluating migraine surgery have reported success, or positive response, rates of 67–91%.1–7 Equally surprising is the comparison between outcomes of the different procedures (ie, surgery, stimulator, and ablation), as seen in Figure 1, compared with the systematic analysis by Ducic et al.18 In both studies, nerve surgery was found to be more common, to have a higher success rates and to have fewer complications compared with nerve stimulator and radiofrequency ablation. The abundance of data available on Facebook and the similarity between the Facebook-reported outcomes and the current literature might be an indication that social media have the potential to evaluate surgical outcomes of migraine surgery and other plastic and reconstructive surgical procedures.
The use of social media in medicine is not new. However, the focus in plastic surgery has usually been on using social media to grow a practice and help educate patients, and our group and others have previously published on this topic.19 However, social networking sites can and have been used to evaluate many aspects of health care and plastic surgery, including evaluating facial attractiveness, measuring acceptance of cosmetic surgery, and reviewing impact of social media use on plastic surgery practice.11, 16, 20–22 However, the use of social media to evaluate outcomes in plastic surgery is limited, and to our knowledge this is the first such study for evaluating migraine surgery.
In a face-to-face clinic visit, physicians can often misinterpret what patients are saying, or patients might report inaccurate symptoms for a variety of reasons.23–26 Social media can provide plastic surgeons insight into their patients’ expectations, concerns, and queries as reported by patients in an unsolicited environment. Such feedback might be extremely difficult or costly to obtain otherwise. It might also help us appreciate patients’ preconceived perceptions before a surgical consultation. All physicians should be aware of the American Medical Association guidelines for physicians’ use of social media.27
Another interesting finding of this study is the 3% of posts that referenced worsening of symptoms after nerve surgery. To our knowledge, this has not been previously reported in the literature. In a survey sent to members of the American Society of Plastic Surgeons who perform migraine nerve surgery, none of the respondents reported that a patient’s migraines worsened after their surgery.28 Without knowing more about these specific patients, we cannot make further conclusions other than recommending that surgeons establish clear expectations before surgery. Even when patients’ symptoms do not change after surgery, it can be an emotionally intense experience as the patients often feel that surgery was their last resort. It is unclear whether patients are reporting they are worse because of actually worsened headache symptoms or other factors such as a surgical complication, disappointment with failure to improve, out of pocket expenses or dissatisfaction with other aspects of their treatment.
Any patient who undergoes surgery may voice their experience, questions, or perceptions on social media, and this activity may positively and negatively impact other patients. Montemurro et al11 report that worldwide, 95% of patients turn to the Internet for information before having a consultation with a plastic surgeon, and almost half of these use social media as their primary source of information. In the present study, we found that patients with migraines are using Facebook to share perceptions and outcomes of their surgical treatment and specifically, 90% recommend nerve surgery. Patients are also offering surgical guidance on Facebook, including advice on choosing a surgeon, which surgery to pursue, insurance coverage, and postoperative recovery and complications. In the present study, we evaluated Facebook posts by individuals who are considering or have undergone surgery for migraines; future studies of other Facebook groups, including those that discuss the impact of migraines or various medical treatments, may yield interesting results. Plastic surgeons should embrace social media as a method for enhancing clinical conversations and anticipate that patients may wish to discuss information they obtained from sites such as Facebook.
There are some limitations to this study. Because of selection bias, we are unsure as to whether outcomes in social media users are different from those in individuals who do not use social media.29 We feel it important to acknowledge this bias while also emphasizing the strength of the data generated from open online discussions. In a recent study of Twitter activity exploring outcomes after lung cancer surgery, Cooke et al30 advocated for the use of social media as a methodology that offers the benefit of studying a more diverse population than that seen with focus groups or individual interviews. Freedman et al31 evaluated barriers to breast cancer treatment by analyzing “user-generated content” on multiple Web sites, including Facebook, Twitter, and WebMD, and supports the use of social media as a “powerful tool” for qualitative research. The present study is observational in nature, and the lack of formal treatment and control groups is a limitation. However, the “open access” nature of social media prohibits the same control as would be seen in such a study. We believe that some of the limitations of the observational nature of the study are also strengths. The patient perspectives evaluated in this study reflect individuals’ online activity separate from a clinic encounter and should be interpreted as such. The “anonymous” nature of the posting allows the subject and the study team members to set aside biases, as these individuals are not necessarily patients of the senior author. The “Facebook perspective” provides us the ability to capture the patient experience in a natural environment, and the outcomes reported by the subjects in this study were unsolicited, essentially eliminating the possibility that patients are reporting better outcomes when being asked directly by their treating surgeon. To explore the relationship between qualitative and quantitative outcomes after migraine surgery, we are planning a study comparing social media activity, semistructured interviews, and validated headache questionnaires.
CONCLUSIONS
This study found a remarkable resemblance between the migraine surgery outcomes as reported by patients on Facebook and the outcomes reported in the literature. Social media will continue to play an expanding role for all plastic surgeons and has the potential to be used for evaluation of outcomes of other procedures in plastic surgery. Similar to the published articles, nerve surgery seems to be efficacious for many patients, and 90% of the posts on Facebook support groups did recommend nerve surgery. Surgical treatment was also rated more favorably compared with nerve stimulator and radiofrequency ablation. This study adds an important perspective to a growing body of evidence advocating for the ongoing use of migraine surgery.
Footnotes
Presented at the 54th Annual Scientific Meeting of the Midwest Association of Plastic Surgeons, 2015: Discovery in Plastic Surgery, May 30, 2015, Chicago, Ill., and at the American Society of Plastic Surgeons Meeting, 2015, October 16 to 20, 2015, Boston, Mass.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Guyuron B, Reed D, Kriegler JS, et al. A placebo-controlled surgical trial of the treatment of migraine headaches. Plast Reconstr Surg. 2009;124:461–468. doi: 10.1097/PRS.0b013e3181adcf6a. [DOI] [PubMed] [Google Scholar]
- 2.Dirnberger F, Becker K. Surgical treatment of migraine headaches by corrugator muscle resection. Plast Reconstr Surg. 2004;114:652–657; discussion 658–659. doi: 10.1097/01.prs.0000131906.27281.17. [DOI] [PubMed] [Google Scholar]
- 3.Poggi JT, Grizzell BE, Helmer SD. Confirmation of surgical decompression to relieve migraine headaches. Plast Reconstr Surg. 2008;122:115–122; discussion 123–124. doi: 10.1097/PRS.0b013e31817742da. [DOI] [PubMed] [Google Scholar]
- 4.Guyuron B, Kriegler JS, Davis J, et al. Five-year outcome of surgical treatment of migraine headaches. Plast Reconstr Surg. 2011;127:603–608. doi: 10.1097/PRS.0b013e3181fed456. [DOI] [PubMed] [Google Scholar]
- 5.Gfrerer L, Maman DY, Tessler O, et al. Nonendoscopic deactivation of nerve triggers in migraine headache patients: surgical technique and outcomes. Plast Reconstr Surg. 2014;134:771–778. doi: 10.1097/PRS.0000000000000507. [DOI] [PubMed] [Google Scholar]
- 6.Janis JE, Dhanik A, Howard JH. Validation of the peripheral trigger point theory of migraine headaches: single-surgeon experience using botulinum toxin and surgical decompression. Plast Reconstr Surg. 2011;128:123–131. doi: 10.1097/PRS.0b013e3182173d64. [DOI] [PubMed] [Google Scholar]
- 7.Ducic I, Hartmann EC, Larson EE. Indications and outcomes for surgical treatment of patients with chronic migraine headaches caused by occipital neuralgia. Plast Reconstr Surg. 2009;123:1453–1461. doi: 10.1097/PRS.0b013e3181a0720e. [DOI] [PubMed] [Google Scholar]
- 8.Janis JE, Barker JC, Javadi C, et al. A review of current evidence in the surgical treatment of migraine headaches. Plast Reconstr Surg. 2014;134(4 Suppl 2):131S–141S. doi: 10.1097/PRS.0000000000000661. [DOI] [PubMed] [Google Scholar]
- 9.Mathew PG. A critical evaluation of migraine trigger site deactivation surgery. Headache. 2014;54:142–152. doi: 10.1111/head.12218. [DOI] [PubMed] [Google Scholar]
- 10.McGeeney BE. Migraine trigger site surgery is all placebo. Headache. 2015;55:1461–1463. doi: 10.1111/head.12715. [DOI] [PubMed] [Google Scholar]
- 11.Montemurro P, Porcnik A, Hedén P, et al. The influence of social media and easily accessible online information on the aesthetic plastic surgery practice: literature review and our own experience. Aesthetic Plast Surg. 2015;39:270–277. doi: 10.1007/s00266-015-0454-3. [DOI] [PubMed] [Google Scholar]
- 12.Fox S. Internet, Science & Tech. Washington, DC: PewResearchCenter; 2011. Feb 28, Peer-to-peer Health Care Pew Study, [Google Scholar]
- 13.Moreno MA, Cox ED, Young HN, et al. Underage college students’ alcohol displays on Facebook and real-time alcohol behaviors. J Adolesc Health. 2015;56:646–651. doi: 10.1016/j.jadohealth.2015.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.D’Angelo J, Kerr B, Moreno MA. Facebook displays as predictors of binge drinking: from the virtual to the visceral. Bull Sci Technol Soc. 2014;34(5–6):159–169. doi: 10.1177/0270467615584044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Egan KG, Moreno MA. Prevalence of stress references on college freshmen Facebook profiles. Comput Inform Nurs. 2011;29:586–592. doi: 10.1097/NCN.0b013e3182160663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khansa I, Khansa L, Pearson GD. Patient satisfaction after rhinoplasty: a social media analysis. Aesthet Surg J. 2016;36:NP1–NP5. doi: 10.1093/asj/sjv095. [DOI] [PubMed] [Google Scholar]
- 17.Moreno MA, Egan KG, Brockman L. Development of a researcher codebook for use in evaluating social networking site profiles. J Adolesc Health. 2011;49:29–35. doi: 10.1016/j.jadohealth.2011.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ducic I, Felder JM, 3rd, Fantus SA. A systematic review of peripheral nerve interventional treatments for chronic headaches. Ann Plast Surg. 2014;72:439–445. doi: 10.1097/SAP.0000000000000063. [DOI] [PubMed] [Google Scholar]
- 19.Israel JS, Mandel BA, Bentz ML, et al. Tweeting all surgeons: update your Facebook status, enhance your reputation, and “pin” your practice on the wild, wild web. Plast Reconstr Surg. 2013;131:865e–868e. doi: 10.1097/PRS.0b013e318287a14f. [DOI] [PubMed] [Google Scholar]
- 20.Fogel J, King K. Perceived realism and Twitter use are associated with increased acceptance of cosmetic surgery among those watching reality television cosmetic surgery programs. Plast Reconstr Surg. 2014;134:233–238. doi: 10.1097/PRS.0000000000000322. [DOI] [PubMed] [Google Scholar]
- 21.Popenko NA, Devcic Z, Karimi K, et al. The virtual focus group: a modern methodology for facial attractiveness rating. Plast Reconstr Surg. 2012;130:455e–461e. doi: 10.1097/PRS.0b013e31825dcb48. [DOI] [PubMed] [Google Scholar]
- 22.Vardanian AJ, Kusnezov N, Im DD, et al. Social media use and impact on plastic surgery practice. Plast Reconstr Surg. 2013;131:1184–1193. doi: 10.1097/PRS.0b013e318287a072. [DOI] [PubMed] [Google Scholar]
- 23.Mulley AG, Trimble C, Elwyn G. Stop the silent misdiagnosis: patients’ preferences matter. BMJ. 2012;345:e6572. doi: 10.1136/bmj.e6572. [DOI] [PubMed] [Google Scholar]
- 24.Cocco G. Erectile dysfunction after therapy with metoprolol: the Hawthorne effect. Cardiology. 2009;112:174–177. doi: 10.1159/000147951. [DOI] [PubMed] [Google Scholar]
- 25.Baig MR, Levin TT, Lichtenthal WG, et al. Factitious disorder (Munchausen’s syndrome) in oncology: case report and literature review. Psychooncology. 2016;25:707–711. doi: 10.1002/pon.3906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghori AK, Chung KC. A decision-analysis model to diagnose feigned hand weakness. J Hand Surg Am. 2007;32:1638–1643. doi: 10.1016/j.jhsa.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 27.McMahon J., Sr Report of the council on ethical and judicial affairs: professionalism in the use of social media. CEJA. 2011;8:3–7. [PubMed] [Google Scholar]
- 28.Kung TA, Pannucci CJ, Chamberlain JL, et al. Migraine surgery practice patterns and attitudes. Plast Reconstr Surg. 2012;129:623–628. doi: 10.1097/PRS.0b013e3182412a24. [DOI] [PubMed] [Google Scholar]
- 29.IQS Research. Social Media as a Research Tool—the Danger of Selection Bias. Available at: http://iqsresearch.com/social-media-as-a-research-tool-the-danger-of-selection-bias/. Accessed July 4, 2016.
- 30.Cooke DT, West H, Conway L, et al. Social media can be used as a qualitative research tool in surgical patient-centered outcomes research. J Am Col Surgeons. 2015;221:e29. [Google Scholar]
- 31.Freedman RA, Viswanath K, Vaz-Luis I, et al. Learning from social media: utilizing advanced data extraction techniques to understand barriers to breast cancer treatment. Breast Cancer Res Treat. 2016;158:395–405. doi: 10.1007/s10549-016-3872-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


