Abstract
Spondylodiscitis is often iatrogenic in nature. We report the case of a 69-year-old man presenting with spondylodiscitis and associated epidural abscess following transrectal ultrasonography guided prostate biopsy despite ciprofloxacin cover. To our knowledge, this is the first case of spondylodiscitis secondary to fluoroquinolone resistant Escherichia coli.
Keywords: Prostate, Biopsy, Spondylodiscitis
Prostate cancer is the most commonly diagnosed cancer in men, accounting for approximately a quarter of all male cancers. Transrectal ultrasonography guided biopsy of the prostate (TRUBP) is a common procedure in the diagnosis of prostate cancer and has a good safety profile. However, infective complications following biopsy (including bacteriuria, bacteraemia, fever and sepsis) are well documented, occurring in 2–4% of patients despite appropriate antibiotic cover.1
Spondylodiscitis is a rare condition defined by inflammation of the intervertebral disc space and adjacent vertebrae, with an incidence of 0.4–2.4/100,000 per year.2,3 While spondylodiscitis can occur spontaneously, the majority of cases are iatrogenic. Several reports describing spondylodiscitis following TRUBP have been described. However, we believe this is the first case of iatrogenic pyogenic spondylodiscitis with associated epidural abscess, secondary to fluoroquinolone resistant Escherichia coli infection following transrectal prostate biopsy.
Case History
A 69-year-old man underwent TRUBP with ciprofloxacin antibiotic cover, as per local trust guidelines. Four weeks later, he presented with a two-week history of progressive low back pain with associated fever, rigors, bilateral lower limb radiculopathy and numbness, preventing him from undertaking some of his activities of daily living. There were no new bladder or bowel symptoms. Other than benign prostatic hyperplasia, he reported no previous medical history.
Prior to admission to our unit, the patient had completed a two-week course of ciprofloxacin, with no improvement in symptoms.
Examination and imaging
Examination revealed bilateral leg weakness (Medical Research Council grade 3/5 in all myotomes, with associated sensory loss in L1–L5 dermatomes bilaterally). Anal tone and sensation was intact. Cardiovascular examination identified a sinus tachycardia. Blood cultures identified an E coli septicaemia. Lumbosacral magnetic resonance imaging demonstrated discitis at the L3/4 level with local osteomyelitis and an epidural abscess with involvement of the psoas muscle.
Management
Computed tomography guided aspiration of the collection at the level of L2/3 revealed a purulent aspirate, positive for E coli on culture, which was resistant to fluoroquinolones. A combined eight-week course of meropenem and six-week course of co-trimoxazole was commenced.
Discussion
Spondylodiscitis is a rare complication of TRUBP, which is generally a safe procedure. Six cases describing spondylodiscitis following TRUBP have been reported previously. Occurrence of infective complications following TRUBP is not surprising given that 100% of patients develop a transient bacteraemia following the intervention.4 The risk of discitis is increased as a result of the direct vascular connection between venous drainage of both the prostate and lumbar vertebrae.
Until recently, uncertainty over the role of antibiotic prophylaxis existed. A 2011 Cochrane review evaluated the effectiveness of prophylactic antibiotics, reported across nine trials.1 This displayed a significant reduction in complications with appropriate antibiotic cover from 14.8% to 3.9%. Subsequently, the use of prophylactic antibiotics has become common practice, with almost universal cover with fluoroquinolones such as ciprofloxacin.
To the best of our knowledge, we report the first case of spondylodiscitis with associated epidural abscess secondary to a fluoroquinolone resistant E coli infection. However, this case is not the only report of a severe complication secondary to fluoroquinolone resistant bacteria following TRUBP. Assimacopoulus et al describe a case of necrotising epididymo-orchitis resulting from fluoroquinolone resistant E coli infection following TRUBP.5
Ciprofloxacin resistant E coli has been observed in 22% of patients on rectal swab prior to biopsy.6 Similar results, identifying preoperative fluoroquinolone resistant bacteria in 14% of patients, were reported by Duplessis et al, who recommended rectal swab cultures and targeted antibiotic therapy prior to TURBP.7 Prophylactic rectal cleansing with povidone-iodine prior to the biopsy provides another potential solution as it appears to reduce the relative risk of infection following the procedure.8
Figure 1.
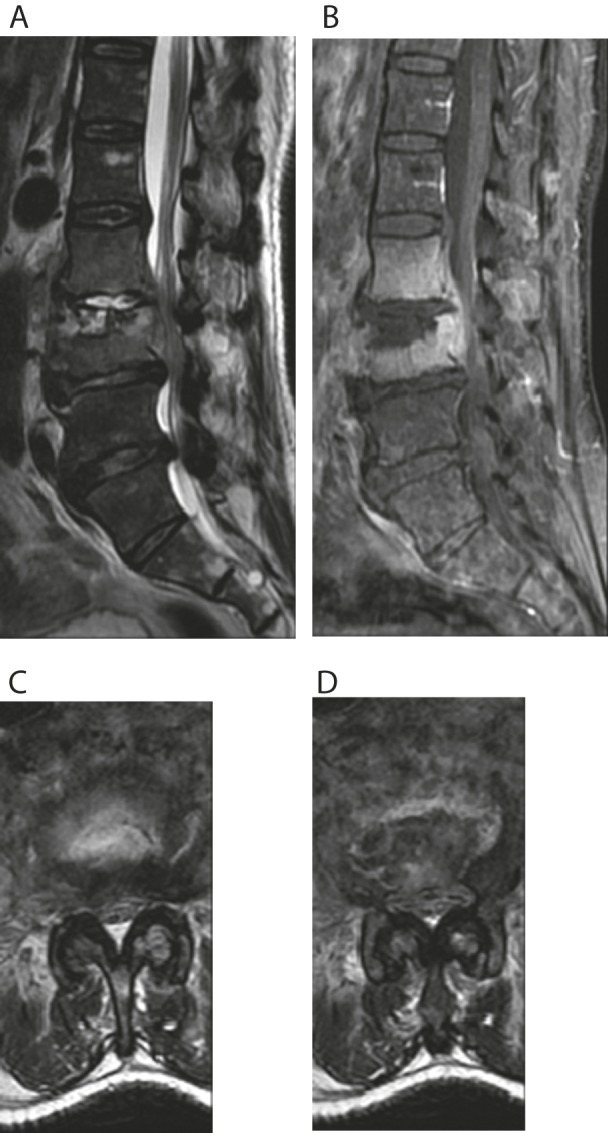
Magnetic resonance imaging: Sagittal T2 weighted imaging (A) displaying loss of disc height and increased signal at the L2/3 level, with associated oedema in the vertebral bodies on T1 weighted imaging (B), and narrowing of the canal; and axial T2 imaging displaying increased signalling in the disc space, with associated cauda equina compression (C and D).
Conclusions
A diagnosis of spondylodiscitis should be considered in patients presenting with low back pain and fever following TRUBP, regardless of antibiotic status. Given the incidence of fluoroquinolone resistant bacteria, blood cultures should be obtained as a matter of urgency in these patients. Owing to the relative ease of performing pre-TRUBP rectal swabs, it is suggested that prophylactic antibiotics tailored to the individual patient are used to reduce the risk of any postoperative infective complications.
References
- 1.Zani EL, Clark OA, Rodrigues Netto N. Antibiotic prophylaxis for transrectal prostate biopsy. Cochrane Database Syst Rev 2011; : CD006576. [DOI] [PubMed] [Google Scholar]
- 2.Cottle L, Riordan T. Infectious spondylodiscitis. J Infect 2008; : 401–412. [DOI] [PubMed] [Google Scholar]
- 3.Grammatico L, Baron S, Rusch E et al. Epidemiology of vertebral osteomyelitis (VO) in France: analysis of hospital-discharge data 2002–2003. Epidemiol Infect 2008; : 653–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thompson PM, Pryor JP, Williams JP et al. The problem of infection after prostatic biopsy: the case for the transperineal approach. Br J Urol 1982; : 736–740. [DOI] [PubMed] [Google Scholar]
- 5.Assimacopoulos A, Johnston B, Clabots C, Johnson JR. Post-prostate biopsy infection with Escherichia coli ST131 leading to epididymo-orchitis and meningitis caused by Gram-negative bacilli. J Clin Microbiol 2012; : 1,157–4,159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steensels D, Slabbaert K, De Wever L et al. Fluroquinolone-resistant E coli in intestinal flora of patients undergoing transrectal ultrasound-guided prostate biopsy – should we reassess our practices for antibiotic prophylaxis? Clin Microbiol Infect 2012; : 575–581. [DOI] [PubMed] [Google Scholar]
- 7.Duplessis CA, Bavaro M, Simons MP et al. Rectal cultures before transrectal ultrasound-guided prostate biopsy reduce post-prostatic biopsy infection rates. Urology 2012; : 556–561. [DOI] [PubMed] [Google Scholar]
- 8.Abughosh Z, Margolick J, Goldenberg SL et al. A prospective randomized trial of povidone-iodine prophylactic cleansing of the rectum before transrectal ultrasound guided prostate biopsy. J Urol 2013; : 1,326–1,331. [DOI] [PubMed] [Google Scholar]


