Abstract
Purpose
Patients transferred between hospitals are at high risk of adverse events and mortality. This study aims to identify which components of the transfer handoff process are important predictors of adverse events and mortality.
Materials and Methods
We conducted a retrospective, observational study of 335 consecutive patient transfers to three ICUs at an academic tertiary referral center. We assessed the relationship between handoff documentation completeness and patient outcomes. The primary outcome was in-hospital mortality. Secondary outcomes included adverse events, duplication of labor, disposition error, and length of stay.
Results
Transfer documentation was frequently absent with overall completeness of 58.3%. Adverse events occurred in 42% of patients within 24 hours of arrival, with an overall in-hospital mortality of 17.3%. Higher documentation completeness was associated with reduced in-hospital mortality (OR 0.07, 95% CI 0.02 to 0.38, p=0.002), reduced adverse events (coef −2.08, 95% CI −2.76 to −1.390, p<0.001), and reduced duplication of labor (OR 0.19, 95% CI 0.04 to 0.88, p=0.033) when controlling for severity of illness.
Conclusions
Documentation completeness is associated with improved outcomes and resource utilization in patients transferred between hospitals.
Keywords: Inter-hospital transfer, hand-off, ICU mortality, information, transitions of care
Introduction
Transitions of care, whether between institutions or within, are frequent sources of medical errors, inefficiency, and unnecessary costs[1–4]. The root cause of adverse events associated with transitions of care is poor transfer of information between providers[5]. Multiple studies demonstrate that improving communication to provide coordinated care during transition can result in more cost efficient care, reduced rate of errors and near misses, and improved patient satisfaction[6–9].
An understudied area within the transitions of care literature is inter-hospital transfers. Multiple barriers such as bed availability, transportation coordination, and establishing an accepting physician create uncertainty in the transfer process and can delay care[7, 10–14]. Moreover, patients who are transferred to tertiary referral centers are heterogeneous, often with complex comorbidities and unique diagnoses. Characterizing this group on a population level and comparing them with a non-transferred population is challenging[15, 16].
Only a handful of studies have investigated the process of transferring patients between hospitals and its impact on clinical outcomes[17, 18]. The field has largely focused on areas in which point-of-care risk stratification is simple; ST segment elevation myocardial infarctions and high risk traumas can be triaged to tertiary care centers via regional protocols[19–22]. These diagnoses constitute only a fraction of indications for inter-hospital transfers. Despite established practices, delays are frequent and often related to unnecessary testing, uncertain diagnoses, and imperfect adherence to guidelines[12, 23–26].
When decision making is complex, patients are diverse, and hospital staffing patterns are variable, creating a transfer protocol to encompass all scenarios is not practical. Even while utilizing specialized retrieval teams (e.g., mobile ICUs) to facilitate movement of critically ill patients, communication errors are commonplace [18, 27, 28]. The Emergency Medical Treatment and Labor Act (EMTALA) demonstrates the importance of stabilizing patients prior to transfer; however, its protections do not apply to patients who decompensate following admission[29].
Ideal handoffs consist of both a verbal and written exchange between providers. Creating protocols for this exchange using programs such as IPASS, which optimized hand-offs during shift changes, have demonstrated a reduction in medical errors[30]. However, a recent survey of intensivists found that only 13% have standardized handoff processes in place, and many reported adverse events related to poor information exchange during handoffs[31]. In a large study of transfer centers, inter-hospital handoff processes varied widely. A verbal handoff was often recorded between providers, but concurrent documentation was rarely required[32].
Integrating clinical documentation and objective data is an important facet of high-quality care coordination[33]; however, the role of complete documentation in transitions of care remains understudied. Documentation completion has been associated with improved data availability[34], improved adherence to guidelines[35], and improved patient satisfaction[36]; however, its full impact on inpatient care delivery and subsequent outcomes remains unclear[37].
In a health care environment with a new focus on care coordination to prevent diagnostic and medical error, we attempted to systematically evaluate the process of patient handoffs between hospitals in order to identify unique predictors of risk and important areas for improvement. This pilot study analyzed 335 consecutive patients transferred to a single academic tertiary care hospital. A novel tool was developed to objectively describe and evaluate the information quality of inter-hospital transfer documentation. We then tested the hypotheses that documentation is an important aspect of a safe transfer, irrespective of the verbal handoff, and that comprehensive transfer documentation is associated with lower mortality, adverse events, and over-utilization.
Methods
We conducted a retrospective observational study of patients transferred to three ICUs (Medical ICU, Surgical ICU, and Cardiac Care Unit) of the Robert Wood Johnson University Hospital (RWJUH). RWJUH is a 610-bed tertiary academic medical center located in New Brunswick, New Jersey and is the principal teaching hospital of Rutgers-Robert Wood Johnson Medical School. Consecutive transfers between December 1, 2011 and December 31, 2012 were identified through transfer center records. Inclusion criteria encompassed all patients directly transferred to a RWJUH ICU from outside hospital critical care units or emergency departments (ED). Patients who were transferred via the RWJUH ED (an extra level of triage) were excluded from the study, as well as all patients under the age of 18. The institutional review board at Rutgers-Robert Wood Johnson Medical School approved the protocol.
Transfer Process
Patient transfer is initiated through the RWJUH transfer center, a unit with the sole purpose of identifying an appropriate accepting physician and coordinating the practical aspects of transport based on bed availability and patient’s clinical status (Supplemental Figure 1). A verbal handoff between physicians is subsequently facilitated by the transfer center at the time of acceptance, and between nurses at the time of transfer. The transfer center also requests that a complete copy of the patient’s chart is sent at the time of transfer.
Unit Descriptions
The Medical ICU is a 16 bed teaching ICU, with a high intensity model of care. Both university and community physicians may be the attending of record, and an in-house overnight intensivist supervises resident- and APN-led patient care. The CCU is a 14 bed teaching ICU, where resident care is supervised by a cardiology boarded university or community physician. The surgical ICU is a 20 bed closed ICU in which a 24 hour in-house acute care surgeon supervises resident- and APN-led patient care.
Completeness of transfer documentation
Reviews of referring hospital records and outcomes were performed independently by two reviewers and results and merged only for averaging and subsequent statistical analysis to maintain blinding of the reviewer to patient outcomes. Each record was evaluated for the presence and completeness of a discharge summary, history and physical, laboratory values, images (including digital copies when important for patient care), consults, medication reconciliation, and progress notes. Each element was given a 0 for absent, 1 for incomplete, or 2 for complete, using strict criteria (Supplemental Data). Cohen’s kappa was calculated from all documentation elements to assess for inter-rater reliability. Documentation completeness presented as a percentage of the total possible points, with a higher score representing the presence of more complete information.
As the percentage of document completeness represents an abstraction of multiple elements of documentation quality, we also performed a Principal Component Analysis including each individual documentation element to develop a weighted transfer score. Two components with Eigenvalues greater than one were identified following orthogonal rotation: documentation completeness (progress note, laboratory values (labs), images, discharge summary, consults, H&P) and transfer timing (progress notes, medication reconciliation, and consults), which were unlikely to be completed in a transfer from the emergency department or early in the hospitalization. Correlation matrix, variable loading, and unexplained variance are shown in supplemental Table I–II.
Outcomes and Measures
The primary outcome was in-hospital mortality using logistic regression. Severity of illness was controlled using MPM0-III, a validated measure based on age, laboratory values, vitals, and comorbidities on arrival that predict mortality[38]. Secondary outcomes were adverse events and duplication of labor. Adverse events reflected early escalations of care as a marker of instability within the first 24 hours of transfer, indicated by intubation, initiation of a new vasopressor, blood product transfusion, and initiation of renal replacement therapy.
We also investigated several measures of resource utilization including duplication of labor, disposition error, and length of stay. Duplication of labor was included as a measure of overutilization unique to patients transferred between facilities. This was defined as a dichotomous variable, and considered present if there was clear evidence of repeat laboratory testing, imaging, or procedures without new medical indication. For example, a repeat cardiac catheterization in advance of open heart surgery, solely due to the unavailability of outside hospital catheterization films, would be identified as duplication of labor. Disposition error was defined positive if a patient was admitted to the ICU and was transferred to the wards within 24 hours without receiving any critical care. There was moderate pre-consensus inter-observer agreement in identifying duplication of labor and disposition error (κ = 0.49), similar to prior studies[8]. Finally, we investigated the management of patients in shock with appropriate access prior to transfer as a means of assessing care quality. Shock was defined if patient arrived with a mean arterial pressure < 65 mm Hg with our without central access established.
Statistics
A summary of variables, their definitions, and their measures is reported in Supplemental Table III. Demographic information was presented as a number and percentage if a dichotomous variable, and a median and inter-quartile range if a continuous variable. Multivariate logistic regression was used to evaluate the relationship between information completeness and inpatient mortality. Poisson regression was used to evaluate the effect of transfer score on adverse events. The measure of documentation completion was included as a ratio (range 0 to 1.0). In each analysis, we controlled for patient demographics, whether the patient was transferred from a referring ED, arrived at night, and MPM0-III. A p value of less than 0.05 was considered statistically significant. STATA v13.0 (StataCorp; College Station, TX) was used for all statistical analysis, and GraphPad Prism 5.0c (GraphPad Software; San Diego, CA) was used for visualization.
Results
Patient Demographics and Outcomes
For the one-year period examined, 335 patients were transferred directly to RWJUH ICUs from 37 centers, mostly located in central New Jersey. This sample represented approximately 8% of all ICU admissions. Patient demographics, outcomes, and measures are summarized in Table I. Indications for transfer are summarized in Supplemental Table I. The overall in-hospital mortality rate was 17.3%. A significant proportion of patients also had features of over-utilization: 10.87% of patients had evidence of labor duplication and 12.8% of patients were unnecessarily admitted to an ICU.
Table I.
Summary statistics, patient demographics, measures, and outcomes.
| Demographics | ||
| N | 335 | |
| Age (IQR) | 63.1 (15.3) | |
| Male (%) | 208 (62) | |
| White | 234 (70) | |
| Race (%) | Black | 34 (10) |
| Other | 67 (20) | |
| MICU | 57 (17) | |
| Unit of arrival (%) | CCU | 144 (43) |
| SICU | 134 (40) | |
| Apache-II (IQR) | 11 (7 – 20) | |
| MPMo-III (IQR) | 10.5 (4.1 – 21.0) | |
| Transfer | ||
| Transit Time, hours (IQR) | 4.1 (2.64 – 9.6) | |
| Patients transferred at night (%) | 163 (48.0) | |
| Patients transferred across shifts (%) | 134 (40.0) | |
| Transferred from Emergency Department (%) | 107 (31.9) | |
| Prior Hospital LOS, days (IQR) | 1.33 (0.6 – 2.7) | |
| Outcomes and Measures | ||
| In-hospital Mortality (%) | 58 (17.3) | |
| Shock on admission (%) | 87 (26.0) | |
| Shock without central access on admission (%) | 31 (9.2) | |
| Adverse Events within 24 hours of arrival (IQR) | 1.0 (0.0 – 2.0) | |
| ICU LOS, days (IQR) | 2.96 (2.0 – 6.81) | |
| Hospital LOS, days (IQR) | 6.33 (2.92 – 14.7) | |
| Patients with Labor Duplication (%) | 36 (10.87) | |
| Patients with Disposition Error (%) | 43 (12.8) | |
Patient triage and transit
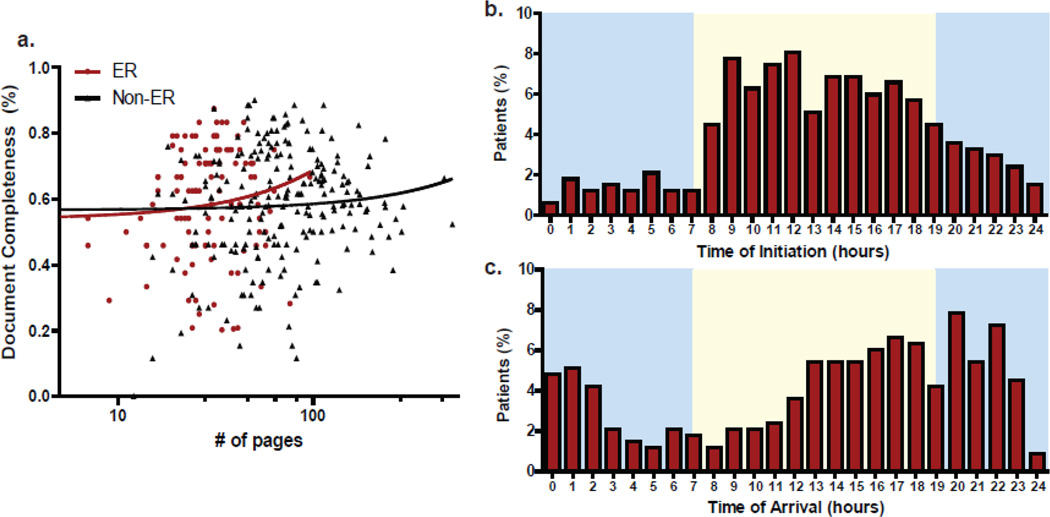
We investigated the transfer process and triage of each patient to identify unique aspects that conferred risk independent of verbal handoff and disease severity. The time of initial call followed a circadian distribution with peak initiation between 12:00 PM and 1:00 PM. Time of arrival followed a bimodal distribution with peak arrival times within one hour of nursing shift change (7:00 to 8:00 PM) and between 1:00 AM and 2:00 AM when staffing is reduced (Figure 1). A mean of 10.9 hours (median 4.1) elapsed between the initial call and patient arrival. There was no correlation between a patient’s severity of illness and the time it took to transfer a patient.
Figure 1. Variation in transfer documentation and patient disposition.
a) There was no relationship between documentation volume and information content, independent of whether patients were transferred from a referring ICU or ED. b,c) despite a circadian distribution of transfer initiation, patient arrival occurred more frequently at night.
Written Transfer Documentation
22,351 pages of outside hospital records were reviewed for the presence and completeness of 2,345 specific elements. Only four charts had no scanned data. Including or excluding these records had no impact on the results, and are included in this analysis. On average, a patient arrived with 67 pages of documentation (SD = 61). The document completion mean was 58% (median 0.6, IQR 0.46 to 0.71, Range 0.0 – 1.0) with no significant difference between ICUs. Inter-observer variability showed moderate agreement for all documentation elements (κ = 0.613), and overall document completeness was similar between the two reviews (r2=0.486, Supplemental Figure 2). Prevalence of individual elements within the transfer documentation is summarized in Table II. A complete discharge summary was only included with 12% of patients, and complete imaging only arrived with 15% of patients. Remarkably, 28.5% of all transferred patients arrived without any documented laboratory analysis.
Table II.
Completion rates and average scores for each documentation element.
| Discharge Element | % Complete | Mean Score (SD) |
|---|---|---|
| History and Physical | 128 (38.2) | 1.34 (0.69) |
| Discharge Summary | 41 (12.2) | 0.8 (0.67) |
| Laboratory Values | 203 (60.6) | 1.66 (0.53) |
| Images | 49 (14.6) | 1.16 (0.56) |
| Consults | 107 (32.9) | 1.38 (0.59) |
| Progress Notes | 132 (39.4) | 1.34 (0.69) |
| Medication Reconciliation | 97 (29.0) | 0.9 (0.41) |
There was no correlation between the number of pages arriving with the patient and the completeness of information (Figure 1). Patients arriving from EDs, 96% of which had a full adoption of electronic health records (EHR), had a lower volume of documentation than patients arriving from other referring units, which had a full EHR adoption rate of only 7%. Despite high EHR compliance and low documentation burden, the correlation between quality and quantity remained absent for ED to ICU transfers. Document completeness did not improve with increased transit time, defined as time from initial call to patient arrival (p=0.379). Longer outside hospital length of stay, in which the burden of documentation is inherently higher, also did not correlate with the completion of documentation (p=0.694). We also did not identify a statistically significant correlation between the completeness of documentation and MPM0-III score (p=0.208).
As an unweighted percentage, documentation completeness captures the end product of multiple components of documentation quality and the transfer process. We performed a Principal Component Analysis to generate an objective weighted documentation score (Supplemental Table II). Two components were identified: a documentation score (progress notes, history and physical, discharge summary, labs, consults, and images), which did not vary by the transit time (p=0.831) or the length of stay at the prior hospital (p=0.908), and another component related to elements which were largely impacted by transfer coordination and timing (consults, progress notes, and medication reconciliation). This score increased with both transit time (p=0.041), duration of prior hospital stay (p=0.019), and was significantly lower in ED to ICU transfers (p<0.001).
Transfer, Information completeness, and Outcomes
When controlling patient demographics, severity of illness using MPM0-III, the timing of transfer, and patient demographics, higher degree of document completeness was associated with lower in-hospital mortality (OR 0.07, 95% CI 0.02 to 0.38, p=0.002) and reduced adverse events within 24 hours (coeff −2.08, 95% CI −2.76 to −1.390, p<0.001, Table 3). Greater documentation completeness was also associated with a reduced rate of labor duplication (OR 0.19, 95% CI 0.04 to 0.88, p=0.033), but not disposition error (p=0.39). Arrival at night, transit time, and transfer from referring hospital ED was not significantly related to adverse events or inpatient mortality in this study.
Table III.
Multivariate regression of outcomes of patients transferred from outside hospitals
| In Hospital Mortality | Adverse Events within 24 hours | |||||
|---|---|---|---|---|---|---|
| Variable | OR | 95% CI | p | coef | 95% CI | p |
| Male | 1.31 | (0.69 to 2.48) | 0.84 | 0.25 | (−0.04 to 0.55) | 0.09 |
| White | 1.00 | Reference | 1.00 | Reference | ||
| Black | 0.86 | (0.27 to 2.67) | 0.788 | −0.02 | (−0.51 to 0.48) | 0.95 |
| Other | 1.25 | (0.59 to 2.67) | 0.559 | 0.11 | (−0.21 to 0.43) | 0.51 |
| MPM0-III | 15.22 | (2.11 to 109.52) | 0.007 | 1.51 | (0.70 to 2.33) | <0.001 |
| ER Transfer | 1.14 | (0.51 to 2.52) | 0.32 | 0.11 | (−0.23 to 0.45) | 0.45 |
| Night Transfer | 1.34 | (0.72 to 2.49) | 0.36 | 0.20 | (−0.08 to 0.48) | 0.16 |
| Document Score | 0.78 | (0.62 to 0.92) | 0.001 | −0.25 | (−0.34 to −0.17) | <0.001 |
| Transfer Timing | 1.01 | (0.74 to 1.38) | 0.95 | −0.10 | (−0.24 to 0.04) | 0.15 |
Similarly, a higher weighted documentation score was associated with reduced mortality (OR 0.78, 95% CI 0.62 to 0.92, p = 0.001), reduced adverse events (coef −0.25, 95% CI −0.33 to −0.17, p <0.001), and reduced duplication of labor (OR 0.66, 95% CI 0.52 to 0.86, p = 0.001). The measure reflecting transfer timing was not associated with mortality, adverse events, or over-utilization (Table III).
Individual elements of the transfer documentation were disproportionately important in their association with patient outcomes. The presence of complete laboratory analysis independently correlated with reduced in-hospital mortality (OR 0.55, 95% CI 0.33 to 0.92, p=0.02) when controlling for the other elements of the transfer score; whereas a complete history and physical (coef −0.32, 95% CI −0.44 to −0.11, p=0.002), discharge summary (coef −0.24, 95% CI −0.49 to −0.01, p=0.05), and images (coef −0.28, 95% CI −0.53 to −0.03, p=0.030) were associated with reduced adverse events within the first 24 hours by Poisson regression (Table 4).
Table IV.
Multivariate regression of individual transfer elements on patient outcomes
| Discharge Element | In-Hospital Mortality | Adverse Events within 24 hours | ||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p value |
coeff | 95% CI | p value | |
| Discharge Summary | 0.75 | 0.44 to 1.27 | 0.138 | −0.24 | −0.49 to −0.01 | 0.05 |
| History and Physical | 1.01 | 0.65 to 1.60 | 0.936 | −0.32 | −0.44 to −0.11 | 0.002 |
| Consults | 1.02 | 0.64 to 1.65 | 0.921 | −0.12 | −0.34 to 0.09 | 0.248 |
| Laboratory Values | 0.55 | 0.33 to 0.92 | 0.021 | −0.21 | −0.44 to 0.02 | 0.070 |
| Images | 0.64 | 0.36 to 1.12 | 0.121 | −0.28 | −0.53 to −0.03 | 0.030 |
| Medication Reconciliation |
0.83 | 0.40 to 1.75 | 0.641 | −0.05 | −0.50 to 0.28 | 0.747 |
| Progress Notes | 0.78 | 0.31 to 1.94 | 0.601 | 0.12 | −0.31 to 0.59 | 0.540 |
Hemodynamic stability
We investigated management of shock during the transfer process as a measure for the quality of care coordination. Eighty-nine patients were transferred with either mean arterial pressure < 65 on admission or requiring vasopressors. Of these patients, 31 had no central access on admission. When controlling for patient demographics, arrival at night, and ED origination, more complete documentation was associated with a lower probability of arriving with a MAP < 65 (OR 0.17, 95% CI 0.1 to 0.4, p<0.001), or without central access (OR 0.19, 95% CI 0.07 to 0.84, p 0.041).
Discussion
The goal of this study was to describe and quantify a critical aspect of inter-hospital handoffs that impacts patient outcomes. We developed a novel tool to evaluate transfer documentation quality. When controlling for severity of illness, the completeness of documentation was associated with lower rates of in-hospital mortality, adverse events, and labor duplication. Complete objective information, such as laboratory results and imaging, seemed to disproportionately improve outcomes.
Despite being requested at the time of transfer, referring hospital documentation is commonly incomplete or absent. We investigated a number of potential contributors to poor documentation, such as expedited travel, high patient complexity, and adoption of electronic health records; none of which resulted in consistent changes in documentation quality. Remarkably, the volume of documentation had no association with information completeness. These data provide evidence that current methods and infrastructure are inadequate to assure accurate and complete information transfer when patients move from one facility to another. One overarching solution is EHR interoperability, which would allow for all documentation to be available both pre- and post-transfer. There are a number of barriers to interoperability implementation, but data such as these highlight the critical importance of information loss and its impact on patient outcomes.
This analysis also describes a number of unique aspects of inter hospital transfers, including the duration of transfer, the timing of patient arrival, and the frequency of hemodynamic instability. Primarily driven by administrative bottlenecks such as bed availability, transfer delays were unpredictable, leaving ample time for clinical status changes following the initial verbal sign out. Patients frequently arrived at night, when staffing is reduced and the ability to clarify information from the referring hospital is difficult. About 40% of transfers occurred across practitioner shifts, resulting in a loss of provider continuity. These findings demonstrate the importance of complete, updated objective documentation, so that handoffs are not subject to gaps in communication.
Effective communication and care coordination is a critical process limiting medical errors. The need to establish mechanisms which link communication to health outcomes is a focus of the Institute of Medicine’s report on improving diagnosis[39]. Our study begins to address this gap in literature by finding a significant association between mortality and the quality of communication. This is likely due to challenges particular to inter-hospital transfer: variability in transfer time, high patient acuity, and discontinuity of care. In this context, the consequence of medical error is great, and near-misses become misses. Inter-hospital transfers likely present an optimal model system for studying diagnostic error and patient outcomes. More importantly, as approximately 1.6 million patients are transferred between hospitals on a yearly basis in the US, standardizing the delivery of care to this especially vulnerable population should be a national priority[40].
Checklists such as found in the NJ universal transfer form and universal accept tools employed by Malpass et al, have not been shown to improve risk adjusted mortality or length of stay[17]. This is likely explained by multiple additional barriers, for example, pending dictations or the ability to generate final radiology images, which may impede communication despite a practitioner’s best effort. EHR adoption alone may not address these infrastructural challenges due to lack of interoperability. However, these data suggest regional adoption of health information exchanges, and improved communication between individual information systems has the potential to improve mortality, care coordination, and cost effectiveness.
Our study has several limitations. First, as this is a retrospective, single center chart review, individual reviewers could not be blinded to a patient’s mortality. While they were blinded to other clinical outcomes such as adverse events and severity of illness, which remained robust, we cannot rule out potential observer bias, thus tempering the strength of our conclusions. However, this concern is abrogated by the agreement of independent documentation reviews, as well as the high diversity of patients in whom important predictors of mortality are likely to be variable. Additionally, as a retrospective study, documentation completion likely captures many unobserved and interacting variables. We attempted to adjust for this using principal component analysis, but ultimately these findings warrant validation in a prospective study.
Adjustment for illness severity is another challenge. We elected to use MPM0-III as it is limited to findings on patient arrival[38], and is largely driven by diagnoses that are less likely to be a result of the transfer process. While we found no significant association between MPM0-III and documentation completeness, we did find that patients with less complete documentation were more likely to present in shock. Unstable patients may present an instance where expedience trumps the quality of a transfer. While superficially this appears reasonable, the end result is that the most unstable patients receive the least care coordination, and unsurprisingly the worst outcomes.
An important concern is that patients who are transferred between facilities often have diagnoses for which unified risk stratification tools are inadequate [15, 41]. We adjusted for this by studying a highly variable patient population that included three different ICUs. The relationship between documentation completeness and patient outcomes remained significant in disparate patient populations and ICU staffing structures, strengthening our conclusions.
This study relies on the assumption that care at the outside facility adhered to best practice independent of the quality of the transfer. However, optimal treatment during a transition requires high quality communication and a system for feedback in order to provide coordinated care. The quality of documentation may serve as a marker for poor communication or the overall quality of care. We find some evidence of this, as incomplete documentation correlated with higher rate of hemodynamic instability on arrival, and a lower rate of central line placement. Whether direct or indirect, the association between information content and outcomes implies the need for high quality communication throughout the transfer. Quality improvement initiatives should focus not only on making clinical information complete at the time of transfer, but facilitating more fluid communication throughout the continuum of the transfer.
Finally, the crux of investigating care transitions is demonstrating that improvement in the handoff process improves patient important outcomes, such as mortality. The strength of these data is provocative, but significant infrastructural barriers exist for quality improvement. Not only does the lack of adequate documentation inhibit care coordination, it prevents identification of medical errors and signs of instability prior to transfer, both of which are necessary for quality improvement and additional research. Mandating complete documentation including laboratory analysis and images as a requirement for transfer is a reasonable first step in improving outcomes. This study provides an evidence-based framework to justify this step, both to improve care coordination as well as a necessity for future quality improvement initiatives.
Conclusion
This study highlights the degree of information discontinuity that exists when critically ill patients are transferred between hospitals and the marked impact of information loss on mortality, adverse events, and resource utilization. Quality improvement based on effective triage, improved communication, and complete objective information at the time transfer may improve outcomes and facilitate higher value care.
Supplementary Material
Highlights.
We developed a tool to evaluate the documentation of patients transferred between hospitals.
We show that patients arrive frequently with incomplete or absent documentation.
Document completeness is associated with improved in-patient outcomes.
Acknowledgments
Funding: NIH Clinical and Translational Science Award at the University of Minnesota: UL1TR000114.
We would additionally like to thank Sarang Kim and Anne Marie Webber-Main for their critical review prior to submission.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No conflict of interests for any author.
References
- 1.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 2.Raduma-Tomas MA, Flin R, Yule S, Williams D. Doctors' handovers in hospitals: a literature review. BMJ Qual Saf. 2011;20(2):128–133. doi: 10.1136/bmjqs.2009.034389. [DOI] [PubMed] [Google Scholar]
- 3.Snow V, Beck D, Budnitz T, Miller DC, Potter J, Wears RL, Weiss KB, Williams MV. Transitions of Care Consensus Policy Statement American College of Physicians-Society of General Internal Medicine-Society of Hospital Medicine-American Geriatrics Society-American College of Emergency Physicians-Society of Academic Emergency Medicine. J GEN INTERN MED. 2009;24(8):971–976. doi: 10.1007/s11606-009-0969-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wohlauer MV, Arora VM, Horwitz LI, Bass EJ, Mahar SE, Philibert I. The patient handoff: a comprehensive curricular blueprint for resident education to improve continuity of care. Acad Med. 2012;87(4):411–418. doi: 10.1097/ACM.0b013e318248e766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Commission TJ. The Joint Commission. Sentinel event statistics data: root causes by event type. 2013 http://wwwjointcommissionorg/sentinal_event_statistics. [Google Scholar]
- 6.Abraham J, Kannampallil T, Patel B, Almoosa K, Patel VL. Ensuring patient safety in care transitions: an empirical evaluation of a handoff intervention tool. AMIA Annu Symp Proc. 2012;3 [PMC free article] [PubMed] [Google Scholar]
- 7.Gombeski WR, Jr, Konrad D, Kanoti G, Ulreich S, Skilogianis J, Clough J. Selection of a hospital for a transfer: the roles of patients, families, physicians and payers. Journal of hospital marketing. 1997;12(1):61–77. [PubMed] [Google Scholar]
- 8.Starmer AJ, Sectish TC, Simon DW, Keohane C, McSweeney ME, Chung EY, Yoon CS, Lipsitz SR, Wassner AJ, Harper MB, et al. Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA : the journal of the American Medical Association. 2013;310(21):2262–2270. doi: 10.1001/jama.2013.281961. [DOI] [PubMed] [Google Scholar]
- 9.Nagpal K, Abboudi M, Fischler L, Schmidt T, Vats A, Manchanda C, Sevdalis N, Scheidegger D, Vincent C, Moorthy K. Evaluation of postoperative handover using a tool to assess information transfer and teamwork. Ann Surg. 2011;253(4):831–837. doi: 10.1097/SLA.0b013e318211d849. [DOI] [PubMed] [Google Scholar]
- 10.Bertazzoni G, Cristofani M, Ponzanetti A, Trabalzini A, Attalla H, De Vito C, Villari P. Scant justification for interhospital transfers: a cause of reduced efficiency in the emergency department. Emerg Med J. 2008;25(9):558–561. doi: 10.1136/emj.2007.052415. [DOI] [PubMed] [Google Scholar]
- 11.Boockvar KS, Fridman B. Inter-facility transfer of patient information before and after HIPAA privacy measures. J Am Med Dir Assoc. 2006;7(3 Suppl):38. doi: 10.1016/j.jamda.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 12.Chatoorgoon K, Huezo K, Rangel E, Francois N, Schweer L, Daugherty M, Koehn M, Ricketts C, Brown RL, Garcia VF, et al. Unnecessary imaging, not hospital distance, or transportation mode impacts delays in the transfer of injured children. Pediatric emergency care. 2010;26(7):481–486. doi: 10.1097/PEC.0b013e3181e5bef3. [DOI] [PubMed] [Google Scholar]
- 13.Iwashyna TJ. The incomplete infrastructure for interhospital patient transfer. Crit Care Med. 2012;40(8):2470–2478. doi: 10.1097/CCM.0b013e318254516f. [DOI] [PubMed] [Google Scholar]
- 14.Kelly SG, Hawley M, O'Brien J. Impact of bed availability on requesting and offering in-hospital intensive care unit transfers: A survey study of generalists and intensivists. Journal of critical care. 2013 doi: 10.1016/j.jcrc.2012.10.070. [DOI] [PubMed] [Google Scholar]
- 15.Etxebarria MJ, Serrano S, Ruiz Ribo D, Cia MT, Olaz F, Lopez J. Prospective application of risk scores in the interhospital transport of patients. European journal of emergency medicine : official journal of the European Society for Emergency Medicine. 1998;5(1):13–17. [PubMed] [Google Scholar]
- 16.Hill AD, Vingilis E, Martin CM, Hartford K, Speechley KN. Interhospital transfer of critically ill patients: demographic and outcomes comparison with nontransferred intensive care unit patients. J Crit Care. 2007;22(4):290–295. doi: 10.1016/j.jcrc.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Malpass HC, Enfield KB, Keim-Malpass J, Verghese GM. The Interhospital Medical Intensive Care Unit Transfer Instrument Facilitates Early Implementation of Critical Therapies and Is Associated With Fewer Emergent Procedures Upon Arrival. Journal of intensive care medicine. 2014 doi: 10.1177/0885066614521964. [DOI] [PubMed] [Google Scholar]
- 18.Wiegersma JS, Droogh JM, Zijlstra JG, Fokkema J, Ligtenberg JJ. Quality of interhospital transport of the critically ill: impact of a Mobile Intensive Care Unit with a specialized retrieval team. Crit Care. 2011;15(1):R75. doi: 10.1186/cc10064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Luca G, Ernst N, Suryapranata H, Ottervanger JP, Hoorntje JC, Gosselink AT, Dambrink JH, de Boer MJ, van 't Hof AW. Relation of interhospital delay and mortality in patients with ST-segment elevation myocardial infarction transferred for primary coronary angioplasty. The American journal of cardiology. 2005;95(11):1361–1363. doi: 10.1016/j.amjcard.2005.01.083. [DOI] [PubMed] [Google Scholar]
- 20.Lossius HM, Kristiansen T, Ringdal KG, Rehn M. Inter-hospital transfer: the crux of the trauma system, a curse for trauma registries. Scandinavian journal of trauma, resuscitation and emergency medicine. 2010;18:15. doi: 10.1186/1757-7241-18-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manari A, Ortolani P, Guastaroba P, Casella G, Vignali L, Varani E, Piovaccari G, Guiducci V, Percoco G, Tondi S, et al. Clinical impact of an inter-hospital transfer strategy in patients with ST-elevation myocardial infarction undergoing primary angioplasty: the Emilia-Romagna ST-segment elevation acute myocardial infarction network. Eur Heart J. 2008;29(15):1834–1842. doi: 10.1093/eurheartj/ehn323. [DOI] [PubMed] [Google Scholar]
- 22.Norwood S, Fernandez L, England J. The early effects of implementing American College of Surgeons level II criteria on transfer and survival rates at a rurally based community hospital. The Journal of trauma. 1995;39(2):240–244. doi: 10.1097/00005373-199508000-00009. discussion 244–245. [DOI] [PubMed] [Google Scholar]
- 23.Mahmoud KD, Gu YL, Nijsten MW, de Vos R, Nieuwland W, Zijlstra F, Hillege HL, van der Horst IC, de Smet BJ. Interhospital transfer due to failed prehospital diagnosis for primary percutaneous coronary intervention: an observational study on incidence, predictors, and clinical impact. European heart journal Acute cardiovascular care. 2013;2(2):166–175. doi: 10.1177/2048872613481449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murphy SM, Whately K, Eadie PA, Orr DJ. Unnecessary inter-hospital referral of minor hand injuries: a continuing problem. Irish journal of medical science. 2010;179(1):123–125. doi: 10.1007/s11845-009-0416-3. [DOI] [PubMed] [Google Scholar]
- 25.Rokos IC, Sanddal ND, Pancioli AM, Wolff C, Gaieski DF. Inter-hospital communications and transport: turning one-way funnels into two-way networks. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2010;17(12):1279–1285. doi: 10.1111/j.1553-2712.2010.00929.x. [DOI] [PubMed] [Google Scholar]
- 26.Smith J, Lynch J, Sugrue M, Caldwell E, Jalaludin B, Sisson G, O'Regan S. An evaluation of compliance with practice guidelines on interhospital trauma transfer. Injury. 2005;36(9):1051–1057. doi: 10.1016/j.injury.2005.05.027. [DOI] [PubMed] [Google Scholar]
- 27.Philpot C, Day S, Marcdante K, Gorelick M. Pediatric interhospital transport: diagnostic discordance and hospital mortality. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2008;9(1):15–19. doi: 10.1097/01.PCC.0000298658.02753.C1. [DOI] [PubMed] [Google Scholar]
- 28.Vos GD, Nieman FH, Meurs AM, Van Waardenburg DA, Ramsay G, Donckerwolcke RA. Problems in interhospital pediatric intensive care transport in The Netherlands: results from a survey of general pediatricians. Intensive care medicine. 2003;29(9):1555–1559. doi: 10.1007/s00134-003-1889-6. [DOI] [PubMed] [Google Scholar]
- 29.Taravella S. San Diego hospital hopes for 'mercy' on fine for illegal patient transfer. Modern healthcare. 1991;21(43):6. [PubMed] [Google Scholar]
- 30.Starmer AJ, Spector ND, Srivastava R, West DC, Rosenbluth G, Allen AD, Noble EL, Tse LL, Dalal AK, Keohane CA, et al. Changes in medical errors after implementation of a handoff program. The New England journal of medicine. 2014;371(19):1803–1812. doi: 10.1056/NEJMsa1405556. [DOI] [PubMed] [Google Scholar]
- 31.Lane-Fall MB, Collard ML, Turnbull AE, Halpern SD, Shea JA. ICU Attending Handoff Practices: Results From a National Survey of Academic Intensivists. Crit Care Med. 2016;44(4):690–698. doi: 10.1097/CCM.0000000000001470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Herrigel DJ, Carroll M, Fanning C, Steinberg MB, Parikh A, Usher M. Interhospital transfer handoff practices among US tertiary care centers: A descriptive survey. Journal of hospital medicine : an official publication of the Society of Hospital Medicine. 2016 doi: 10.1002/jhm.2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kuhn T, Basch P, Barr M, Yackel T Medical Informatics Committee of the American College of P. Clinical documentation in the 21st century: executive summary of a policy position paper from the American College of Physicians. Ann Intern Med. 2015;162(4):301–303. doi: 10.7326/M14-2128. [DOI] [PubMed] [Google Scholar]
- 34.Weiskopf NG, Hripcsak G, Swaminathan S, Weng C. Defining and measuring completeness of electronic health records for secondary use. J Biomed Inform. 2013;46(5):830–836. doi: 10.1016/j.jbi.2013.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zenni EA, Robinson TN. Effects of structured encounter forms on pediatric house staff knowledge, parent satisfaction, and quality of care. A randomized, controlled trial. Arch Pediatr Adolesc Med. 1996;150(9):975–980. doi: 10.1001/archpedi.1996.02170340089017. [DOI] [PubMed] [Google Scholar]
- 36.Humphreys T, Shofer FS, Jacobson S, Coutifaris C, Stemhagen A. Preformatted charts improve documentation in the emergency department. Annals of emergency medicine. 1992;21(5):534–540. doi: 10.1016/s0196-0644(05)82520-x. [DOI] [PubMed] [Google Scholar]
- 37.Mann R, Williams J. Standards in medical record keeping. Clin Med (Lond) 2003;3(4):329–332. doi: 10.7861/clinmedicine.3-4-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Higgins TL, Teres D, Copes WS, Nathanson BH, Stark M, Kramer AA. Assessing contemporary intensive care unit outcome: an updated Mortality Probability Admission Model (MPM0-III) Crit Care Med. 2007;35(3):827–835. doi: 10.1097/01.CCM.0000257337.63529.9F. [DOI] [PubMed] [Google Scholar]
- 39.Singh H, Graber ML. Improving Diagnosis in Health Care--The Next Imperative for Patient Safety. The New England journal of medicine. 2015;373(26):2493–2495. doi: 10.1056/NEJMp1512241. [DOI] [PubMed] [Google Scholar]
- 40.HCUP National Inpatient Sample (NIS) Agency for Healthcare Research and Quality. Rockville, MD: Healthcare Cost and Utilizaltion Project (HCUP); 2012. at: www.hcup-us.ahrq.gov/nisover-view.jsp. [Google Scholar]
- 41.Britto J, Nadel S, Habibi P, Levin M. Pediatric Risk of Mortality Score underestimates the requirement for intensive care during interhospital transport. Crit Care Med. 1994;22(12):2029–2030. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.