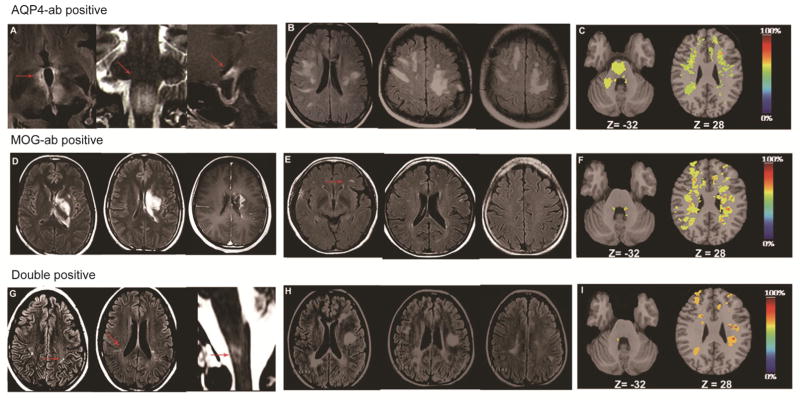
Figure 4.
Brain lesions in MRIs of NMOSD patients with different antibody profiles during attacks. A–C, NMOSD patients with AQP4-ab. D–F, NMOSD patients with MOG-ab. G–I, NMOSD patients with both AQP4 and MOG-abs. A, Typical NMO-like lesion: fluid-attenuated inversion recovery sequence (FLAIR) with T2-weighted hyper-intensities evident in peri-ependymal areas and the diencephalon, including bilateral hypothalamic lesions (A left, arrows); T2-weighted hyperintensities in the floor of the fourth ventricle, bilateral area postrema lesion (A middle, arrow); chiasmal lesion with gadolinium enhancement (A right, arrow). B, ADEM-like lesion without enhancement: patient with extensive bihemispheric subcortical white matter FLAIR signals abnormality without enhancement. The lack of enhancement suggests an intact blood-brain barrier and supports a unique mechanism of edema induction from the dysfunction of water channels. C, Lesion probability distribution for NMOSD patients with AQP4-ab (n=26): the color scale (from 0% to 100%) represents the minimum to maximum probability of a lesion occurring in a particular spatial location. Montreal Neurological Institute (MNI) standard space template Z coordinate is shown in millimeters. D, AMED like lesions with enhancement: a patient with MOG-ab had a large confluent FLAIR signal abnormality in the left putaman, thalamus and paraventricle white matter that demonstrates diffuse gadolinium enhancement. Emerging enhancement suggests disruption of the blood-brain barrier and supports an inflammatory mechanism producing edema. E, MS-like lesion but lesions were too few to satisfy the Barkhof criteria for MS (arrow). F, Lesion probability distribution for NMOSD patients positive for MOG-ab (n=8). G, Small MS-like lesions satisfy Barkhof criteria, also a special NMO-like lesion with area postrema lesion surprisingly happened in the same patient (arrow). H, Large typical MS-like lesions satisfy Barkhof criteria. I, Lesion probability distribution for NMOSD patients with MOG-ab and AQP4-ab (n=10).