Abstract
In this work we demonstrate that blood glucose can be controlled remotely through light stimulated release of insulin from an injected cutaneous depot. Human insulin was tethered to an insoluble but injectable polymer via a linker, which was based on the light cleavable di-methoxy nitrophenyl ethyl (DMNPE) group. This material was injected into the skin of streptozotocin-treated diabetic rats. We observed insulin being released into the bloodstream after a 2 min trans-cutaneous irradiation of this site by a compact LED light source. Control animals treated with the same material, but in which light was blocked from the site, showed no release of insulin into the bloodstream. We also demonstrate that additional pulses of light from the light source result in additional pulses of insulin being absorbed into circulation. A significant reduction in blood glucose was then observed. Together, these results demonstrate the feasibility of using light to allow for the continuously variable control of insulin release. This in turn has the potential to allow for the tight control of blood glucose without the invasiveness of insulin pumps and cannulas.
Keywords: insulin, light controlled drug release, photoactivated depot, DMNPE
Introduction
Insulin continues to be the main treatment for type 1 diabetes.1−4 As effective as insulin is, it has major problems associated with its use. It has low oral bioavailability, requiring it to be injected.5,6 In addition, its dosage is highly variable through the course of a day, depending on diet as well as activity level. Ideally, for insulin to be most effective, it would be administered in amounts that would vary minute by minute, as blood glucose itself varies minute by minute. This is impractical currently, as even a regimen of 4–5 variable injections per day is a challenge for the typical patient. Because of these issues, there has been significant interest in the development of an artificial pancreas, a system that can administer variable amounts of insulin in response to blood glucose information.7−11 Multiple solutions to this problem have been explored, including (1) exogenous implanted beta cells,12 (2) sugar responsive insulin releasing polymers,13 and (3) a continuous glucose monitor (CGM) combined with an insulin pump.7,14 The latter approach is the most mature and is the subject of human clinical trials.
One of the advantages of the CGM/pump approach is that the function of blood glucose monitoring is separated from the function of insulin delivery, so that each piece of the final system can be optimized independently. This increases the chances of the complete system working robustly. One of the main challenges associated with insulin pumps is that they require a physical connection between the outside of the patient (i.e., insulin reservoir) and the inside of the patient. This connection is typically a cannula that is inserted subcutaneously. This leads to multiple problems: The point of insertion gets rapidly biofouled, leading to variation in delivery or complete blockage, requiring cannula replacement every 2 days. In addition, the pump and cannula in the course of a normal active life can get snagged or removed.15−18 What we have sought is a method of insulin delivery that retains the advantages of a pump (continuous, variable insulin release), while eliminating the physical connection between insulin reservoir and the patient. Ideally it would allow the insulin to be initially administered in a fashion identical to normal insulin via injection, but allow for continuously variable release in response to blood glucose information.
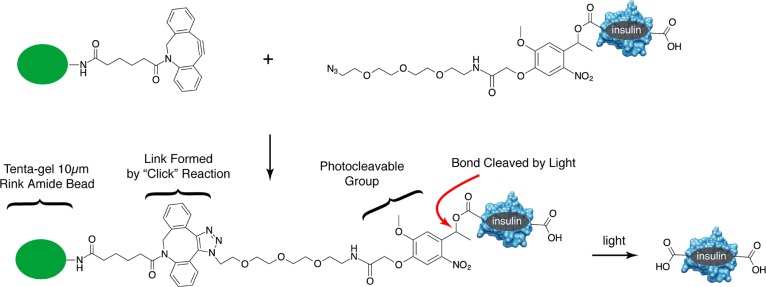
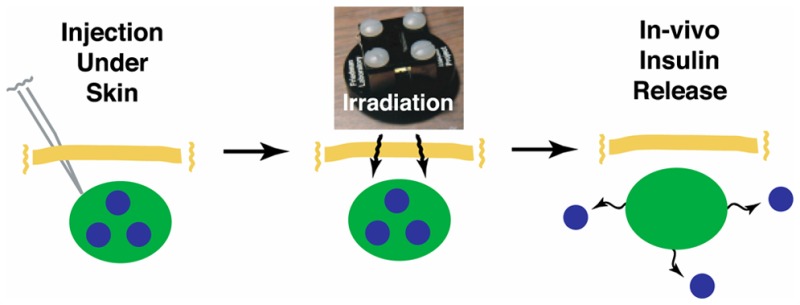
We introduced such an approach recently, the so-called PhotoActivated Depot or PAD approach.19 This prior work described a material in which insulin was linked to an insoluble polymer via a photocleavable linker. We demonstrated in vitro that insulin was released from this material in a controlled and predictable fashion using pulses of light from an LED. The long-term aim for such a material is that it be injected in a fashion identical to insulin (i.e., cutaneously) and then be irradiated through the skin by a small light source that is guided by blood glucose information (Figure 1). Thus, insulin release could be varied continuously without the need for a physical connection that is inherently vulnerable and invasive. The success of this material in vitro suggested multiple critical questions that we sought to address in this work: (1) Can sufficient light cross the upper layers of skin to allow photolysis of the PAD in vivo? (2) Will the released insulin retain its biological activity, despite the synthetic processing required to originally create the PAD? (3) Can sufficient moles of insulin be released to stimulate blood glucose reduction? (4) Can insulin release be varied by varying the amount of light applied?
Figure 1.
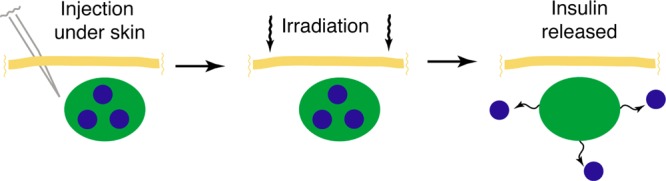
PhotoActivated Depot (PAD) approach. PAD material consisting of insulin linked to polymer via photocleavable linker injected under the skin. This is followed by transcutaneous irradiation, photolysis of the insulin–PAD bond, and uptake into circulation.
In this work, we demonstrate that an insulin PAD succeeds in all these requirements. Insulin released from the insulin PAD retains its biological activity after photolysis. After intradermal injection of the material to form the insoluble depot site in the skin of diabetic rats, light from a compact LED source is capable of stimulating release of insulin into the bloodstream. We demonstrate that additional pulses of LED illumination result in additional pulses of insulin released into the bloodstream. Finally, we show that insulin release is followed by a reduction in blood glucose. All the observed effects are specific to the irradiation of the depot and are not seen in control animals, similarly treated. The results confirm the potential of remotely controlled drug release, which will be particularly useful in the case of diseases like diabetes that require highly varying amounts and highly varying timing of administration.
Materials and Methods
In addition to the following, a complete description of methods and materials, including characterization of photoactivated depot materials and intermediates, is contained in detail in the Supporting Information.
Light Source
The light source was constructed from a Nichia NCSU033B LED, with a 365 nm peak irradiation. This was driven by a 6.5 V power source using a current limiting power resistor. The light source holds the LED ∼0.32 cm from the skin surface, and the measured absolute irradiance at the skin was 0.71 W/cm2. The absolute irradiance of the light source was determined using a calibrated USB2000 spectrophotometer (Ocean Optics) and a CC-3–UV-S cosine corrector via an optic fiber. The Spectrasuite software was used to analyze absolute irradiance in the range of 350–400 nm that brackets the LED output.
Animals
Spague Dawley male rats (250–300 g) were obtained from Harlan Laboratories (Indianapolis, IN). Chemical diabetes was induced by treatment with 65 mg/kg Streptozotocin (Sigma-Aldrich, St. Louis, MO). Diabetes was defined as blood glucose concentrations >250 mg/dL on 3 consecutive days using a One Touch II glucometer and blood obtained from the tail vein.
This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health, eighth edition. The protocol was approved by the University of Missouri Kansas City Institutional Animal Care Use Committee protocol #1401.
Intradermal Injection of PAD Material
Rats were anesthetized with isoflurane gas using a precision vaporizer. The upper backs of rats were shaved prior to injection of the PAD materials. Injections of ∼80 μL of PAD material were made using a 1/2 cc syringe and a 27 gauge needle. Due to limitations of the volume of material that can be injected into the dermal layer of skin at one time, two injections (40 μL each) of PAD materials were made side by side. The compact LED light source was anchored to the skin over the injection sites by two small dots of superglue. Rats’ body temperature and hydration was maintained throughout the experiment.
Insulin Analysis by ELISA
Blood samples were collected in Microvette 100 μL Li-HEP tubes (Sarstedt) from the tail-vein using a glass capillary. After collecting all time points from an experiment, the samples were centrifuged at 5000 rpm for 2 min. The supernatant was removed and stored at −20 °C until the ELISA analysis was performed. The ultrasensitive human insulin ELISA kit (Alpco, Salem, NH) was used according to the manufacturer’s instructions.
Glucose Measurements
Glucose measurements were made using One Touch II Lifescan glucometer and strips (Johnson & Johnson, Milpitas, CA) using plasma from blood samples obtained from the tail vein.
Results and Discussion
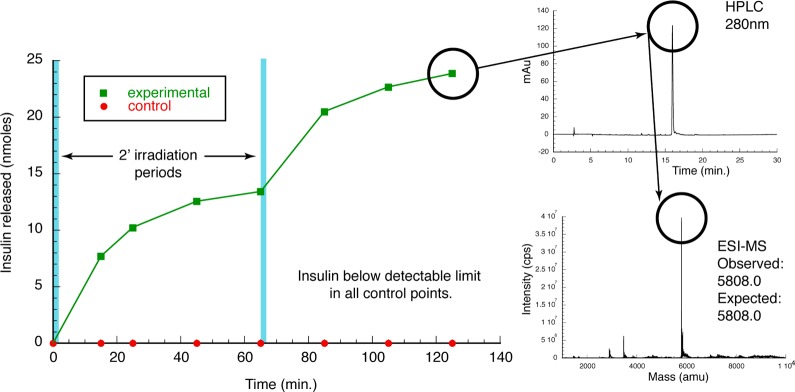
The insulin PAD material was synthesized in an analogous fashion to our previously described material.19 Specifically, human insulin was joined to a photocleavable linker via an ester linkage formed between carboxyl groups on insulin and a diazo group on the linker.19,20 This linker was terminated in an azide. In parallel, we synthesized a base resin that would ultimately attach to the linked insulin. Our previous insulin PAD material was built using ChemMatrix resin as the base upon which insulin was attached via a photocleavable linker. While this resin was sufficient for in vitro demonstration of the approach, it had a particle size (150–500 μm) that was too large to be conveniently injected during in vivo experiments. We therefore created a new PAD material using small diameter TentaGel Rink amide beads (Rapp Polymere). These were 10 μm in diameter, which allowed them to be injected using a standard 27 G needle. The amine group of the resin was coupled with dibenzocyclooctyne (DBCO) acid.21,22 The DBCO was then coupled via a “click” reaction with insulin monoazide, which was synthesized as previously described (Figure 2). The final synthesized material was characterized in two ways, by cleavage of the entire species (DBCO-linker-photocleavable group-insulin) from the resin using TFA. This was confirmed to have the expected molecular weight (6597.0 observed, 6593.4 calculated).
Figure 2.
Synthesis of PAD material using a 10 μm Rink-amide Tentagel resin coupled with strained cyclo-octyne, then reacted with IMA (insulin monoazide) containing one photocleavable group. Final material photolyzes to release native insulin.
The material was also photolyzed in vitro using light from a 365 nm LED (Figure 3). In this experiment, test and control samples were treated identically, except that light was blocked from irradiating the control sample by aluminum foil. This allowed the elimination of heat as a factor in insulin release. The only difference between test and control samples was light. We irradiated the samples for 2 min and followed insulin release over time. For the 5 min prior to sampling, we gently vortexed the resin, followed by centrifugation and sample withdraw at the time point. We observed no detectable insulin release for the light-blocked control sample (Figure 3 left) and significant insulin release in the light-irradiated test sample. A majority of the released insulin was detected in the first time point after irradiation, but we continued to see additional release approaching a plateau in later time points. Because we see no insulin release in the control samples, we associate this additional insulin detected to a slower kinetic process such as diffusion from the resin following photolysis. At 65 min, we again irradiated the samples for 2 min and saw a similar pattern: no detectable insulin in the light-blocked control sample and a spike in insulin release, followed by a slower and plateauing evolution of insulin. The material released from the resin in response to irradiation showed an HPLC retention time identical to insulin (Figure 3, upper right). In addition, ESI mass spectrometry confirmed this, showing a native molecular weight (5808.0 calculated, 5808.0 observed) (Figure 3, lower right).
Figure 3.
In vitro insulin PAD photolysis. PAD material was exposed to two 2′ periods of 365 nm LED light (blue bars). Supernatant was monitored for insulin release (left). Material released showed a retention time in HPLC consistent with insulin (upper right), and this was confirmed to be insulin via ESI-MS (lower right).
This PAD material has two key components and attributes: (1) an insoluble, but injectable polymer that keeps the material at the site of injection; (2) a linkage to insulin that is cleaved with light and releases native insulin. Complete synthetic schemes and characterization are contained within the Supporting Information.
Because the insulin was exposed to multiple synthetic steps, some involving organic solvents, we wanted to ensure that it retains biological activity in vivo after this processing. We previously have demonstrated that insulin photoreleased from resin retains the molecular weight and HPLC retention time of native insulin. In addition, it is recognized by anti-insulin antibodies in an ELISA sandwich assay. Both of these data suggest that our processed insulin has retained its native conformation. To confirm that this in vitro activity persists in vivo, we tested our processed insulin in a diabetic rat model. For all studies, we have used a streptozotocin induced rat model of diabetes.23 Diabetes was induced with a one-time injection of streptozotocin resulting in rats with average blood glucose levels of ∼450 mg/dL by day 2 postinjection. For all experiments, we lightly anesthetized the rats to reduce distress during the procedures.
In-vitro, we photolyzed the insulin PAD material, and collected the released insulin in the supernatant above the resin. This released insulin was quantitated using HPLC. We injected 14.2 nmol/kg of this photoreleased insulin into diabetic rats. For all our studies, we injected into the dermal layer of skin. The dermal layer has multiple advantages, including that it is shallow and therefore more accessible to light as well as leading to faster uptake of insulin.24Figure 4 shows the change in blood insulin and glucose levels in response to these injections. Insulin levels increase rapidly, peaking at 15 min. This is accompanied by a rapid decrease in blood glucose levels, demonstrating that, despite synthetic processing, in vitro photoreleased insulin retains biological activity.
Figure 4.
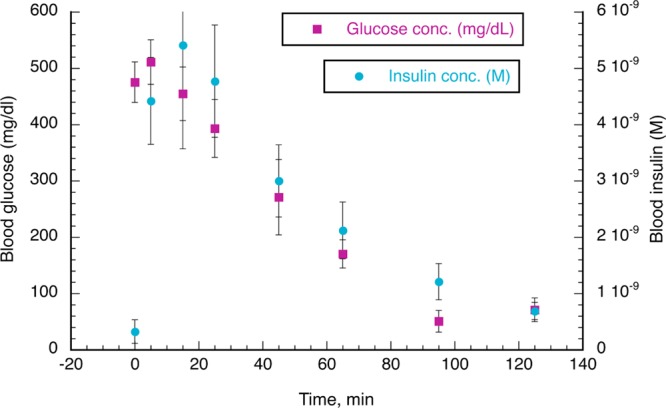
Confirmation of in vivo activity of in vitro photolyzed insulin from the PAD. Insulin isolated from photolyzed PAD material was injected into the dermal layer of diabetic rats (n = 3). Insulin (blue circles) was rapidly detected in the blood. Blood glucose (purple squares) was reduced, confirming in vivo activity of in vitro photolyzed PAD insulin.
The blood glucose reduction that we observed by injecting photoreleased insulin is very similar to what is expected from unprocessed human insulin. Studies with unprocessed human insulin injected intradermally follow similar kinetics with respect to insulin concentration and % blood glucose reduction (data not shown). These matched what is reported elsewhere, specifically that a 2–3 IU/kg dose of human insulin causes an approximately 70% reduction in glucose levels in Sprague–Dawley rats when injected subcutaneously.25−27 We have utilized a 2.36 IU/kg (14.2 nmol/kg) dose here and observe a similar result when injected intradermally.
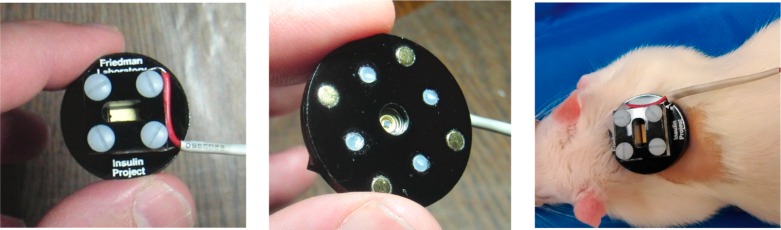
We then examined the ability of the PAD material to release insulin into the systemic circulation after injection and transcutaneous irradiation of the injection site. Diabetic rats were injected with ∼80 μL of PAD material, containing ∼140 nmoles of covalently bound insulin, into the dermal layer. Both experimental and control animals were fitted with a compact LED light source that uses a Nichia 365 nm LED, with an estimated output of 0.71 W/cm2 at the skin (Figure 5). The light source was activated for 2 min at time 0. Control animals were also irradiated but had the light blocked by a layer of aluminum foil, thus allowing for the control of any heat effects (we observe a ∼9 °C increase in temperature during the irradiation period). The only difference between experimental and control animals was the presence of light on the skin of the experimental animals. We did not observe any surface changes such as scabbing in the skin several days postexperiment. We monitored both blood insulin levels and blood glucose levels (via blood obtained from the tail vein). Blood glucose was determined in real time using test strips, and blood insulin levels were determined using a human insulin ELISA assay (Alpco). The ELISA assay shows minimal cross reaction with rat insulin, allowing us to track specifically the human insulin released from our material. Figure 6 shows the results of these experiments performed in triplicate experimental and control animals.
Figure 5.
Compact LED light source used for in vivo studies. Light source shown from top and bottom (left and middle panels) and in place on rat back (right panel).
Figure 6.
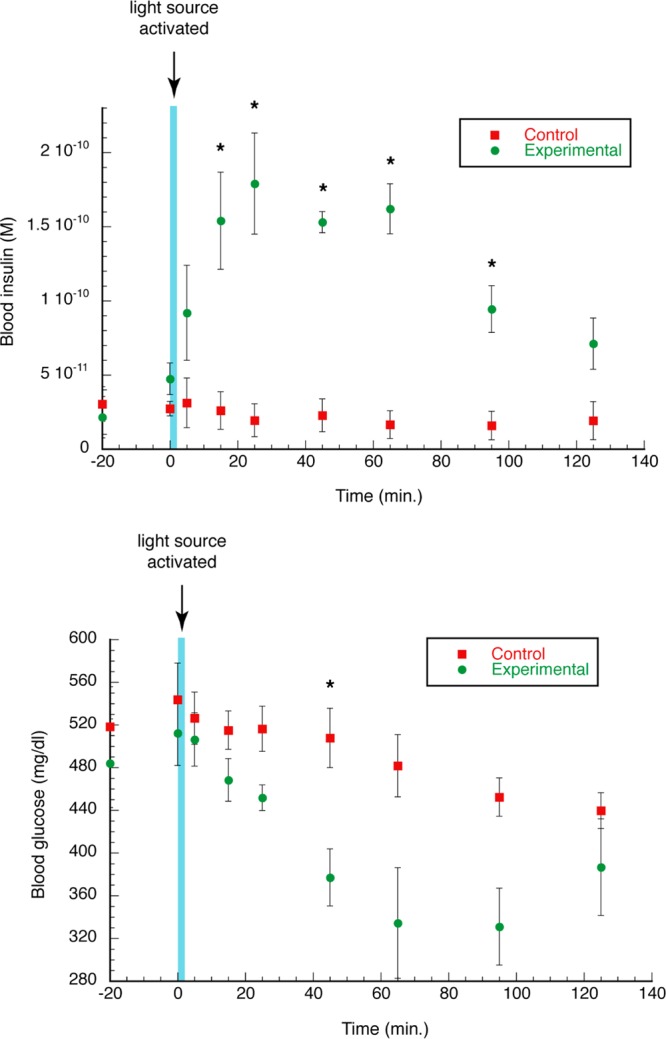
Photoactivated insulin release. Blood insulin levels, as determined by ELISA assay (top panel), and blood glucose levels (bottom panel) before and after a 2 min period of LED activation (indicated by blue bar). * indicates p < 0.05 for differences between control and experimental points.
Prior to irradiation, almost undetectable amounts of insulin are observed in the blood of both experimental and control animals. This persists in the control animal over a 2 h period, demonstrating no leaching of insulin from the PAD material due to biochemical degradation. The experimental animals, however, showed a sharp increase in plasma insulin levels immediately after irradiation, with a peak level at 25 min, followed by a slow decrease. This decrease is likely due to normal degradative and absorptive processes. To our knowledge, this is the first demonstration of insulin release in a live animal stimulated by light.
Following an increase in plasma insulin we observed a modest decrease in blood glucose, with only the 45′ time point showing significance (p < 0.05). We then investigated whether we could further decrease blood glucose by stimulating the release of two pulses of insulin from the depot with a second pulse of LED light from the light source. As before, we injected ∼80 μL of the insulin PAD material containing 140 nmol of insulin covalently linked to the polymer, and then irradiated the skin over the depot site. Control animals again were treated identically except the light was blocked from the skin by aluminum foil. The results are shown in Figure 7.
Figure 7.
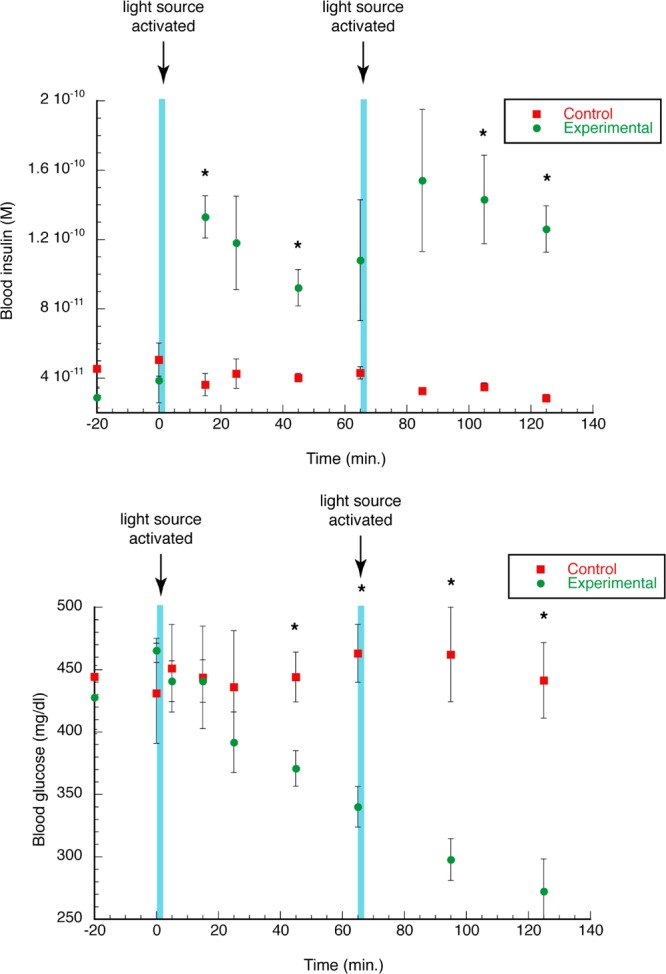
Insulin release and blood glucose reduction with multiple irradiations of PAD. Blood insulin levels, as determined by ELISA assay (top panel), and blood glucose levels (bottom panel) before and after 2 min periods of LED activation at time 0 and 65 min (indicated by blue bar). * indicates p < 0.05 for differences between control and experimental points.
We measured both the blood insulin and glucose levels, starting at 20 min prior to the first irradiation. We observed little to no leaching of insulin from the depot site into the blood. At time 0, we irradiated for 2 min. As before we saw a sharp increase in blood insulin level only in the experimental animals, peaking at 15 min, and a modest drop in blood glucose. At 65 min, we irradiated the injection site for an additional 2 min period and saw an additional release of insulin into the blood, peaking at 85 min. With this additional irradiation step, we now observed a robust drop in blood glucose in the experimental vs control animals. This demonstrates that we can meter insulin release with light and that by doing so we can meter the control of blood glucose.
Conclusions
In this work we have described for the first time an injectable form of insulin that is controlled with light in a living animal. The insulin PAD material described is a first generation material, and each element in it (polymer, photocleavable linker, insulin) is amenable to optimization to improve performance. For example, there is the potential for immunogenicity, and this can be modulated by the nature of the polymer carrier. We currently use a PEG based polymer, which is likely not to be cleared easily from the dermal site, as it is biocompatible, not biodegradable. Second generation materials under development are based on biodegradable polymers or methods that require no polymer. These will eliminate the potential for toxicity associated with the matrix portion of the materials.
In addition, the di-methoxy nitrophenyl ethyl (DMNPE) photocleavable group currently used requires 365 nm light to cleave, which has the potential for phototoxicity. Previous studies that utilize 350–365 nm light for light triggered release in vivo,28,29 or light activated transdermal polymerization30 purposes have not revealed cell toxicity after a 2–3 min exposure. Given this, we are developing materials that release insulin using visible light,31 to eliminate any residual phototoxicity and to increase dermal light penetration. This has the potential to significantly reduce the amount of light needed to photolyze.
An additional point of optimization is the insulin loading of the material. The first generation material is <5% w/w insulin. This resulted in 140 nmol of insulin per depot injection or about 0.8 mg of insulin. This is approximately half of the daily dose for an adult human. Given that the loading efficiency of this material is in the low single digits, it suggests that second generation, higher loading materials (>50%) will have sufficient material to last for several days in a human. We have recently begun developing such higher loading materials.32 Increasing insulin loading and release efficiency can reduce the volume of injection needed, increase the lifetime of the depot, and reduce the amount of light needed to stimulate insulin release.
An optimized insulin PAD has the potential to allow continuously variable release of insulin in response to blood glucose information using a familiar injectable material. As such, it can form the foundation of an artificial pancreas system in which insulin delivery is not controlled by an unwieldy pump and cannula, but rather through pulses of light delivered through a light source. When combined with blood sugar information provided by a continuous glucose monitor (CGM), such a system has the potential to provide a convenient and usable route to control of blood glucose and the health benefits that result from this control.33
Acknowledgments
Research reported in this publication was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number DP3DK106921 as well as the support of a University of Missouri Fast Track Award, the Childrens’ Mercy Hospital Endocrine Section (Dr. Wayne V. Moore), and the UMKC School of Pharmacy Dean’s Bridge Fund. The support of S.H.F. by Drs. Bastian Domajnko, Aram Hezel, Carol Lustig, and Hong Zhang is gratefully acknowledged. We acknowledge Prof. William Gutheil for guidance regarding mass spectrometry issues.
Supporting Information Available
The Supporting Information is available free of charge on the ACS Publications website at DOI: 10.1021/acs.molpharmaceut.6b00633.
Complete and detailed materials and methods, including synthesis and characterization of intermediates and products; HPLC and ESI-MS analysis (PDF)
The authors declare no competing financial interest.
Supplementary Material
References
- Schaan B. D.; Scheffel R. S. Modern insulins, old paradigms and pragmatism: Choosing wisely when deciding how to treat type 1 diabetes. Diabetol. Metab. Syndr. 2015, 7 (1), 35. 10.1186/s13098-015-0033-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahani S.; Shahani L. Use of insulin in diabetes: A century of treatment. Hong Kong Medical Journal 2015, 21 (6), 553–559. 10.12809/hkmj154557. [DOI] [PubMed] [Google Scholar]
- Stephens E. Insulin Therapy in Type 1 Diabetes. Med. Clin. North Am. 2015, 99 (1), 145–156. 10.1016/j.mcna.2014.08.016. [DOI] [PubMed] [Google Scholar]
- Switzer S. M.; Moser E. G.; Rockler B. E.; Garg S. K. Intensive Insulin Therapy in Patients with Type 1 Diabetes Mellitus. Endocrinol. Metab. Clin. North Am. 2012, 41 (1), 89–104. 10.1016/j.ecl.2011.12.001. [DOI] [PubMed] [Google Scholar]
- Lopes M.; Simones S.; Veiga F.; Seica R.; Ribeiro A. Why most oral insulin formulations do not reach clinical trials. Ther. Delivery 2015, 6 (8), 973–987. 10.4155/TDE.15.47. [DOI] [PubMed] [Google Scholar]
- Sousa F.; Castro P.; Fonte P.; Sarmento B. How to overcome the limitations of current insulin administration with new non-invasive delivery systems. Ther. Delivery 2015, 6 (1), 83–94. 10.4155/tde.14.82. [DOI] [PubMed] [Google Scholar]
- Battelino T.; Omladic J. S.; Phillip M. Closed loop insulin delivery in diabetes. Best Practice and Research: Clinical Endocrinology and Metabolism 2015, 29 (3), 315–325. 10.1016/j.beem.2015.03.001. [DOI] [PubMed] [Google Scholar]
- Davis T.; Salahi A.; Welsh J. B.; Bailey T. S. Automated insulin pump suspension for hypoglycaemia mitigation: Development, implementation and implications. Diabetes, Obes. Metab. 2015, 17 (12), 1126–1132. 10.1111/dom.12542. [DOI] [PubMed] [Google Scholar]
- Forlenza G. P.; Buckingham B.; Maahs D. M. Progress in Diabetes Technology: Developments in Insulin Pumps, Continuous Glucose Monitors, and Progress towards the Artificial Pancreas. J. Pediatr. 2015, 169, 13. 10.1016/j.jpeds.2015.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haidar A.; Legault L.; Messier V.; Mitre T. M.; Leroux C.; Rabasa-Lhoret R. Comparison of dual-hormone artificial pancreas, single-hormone artificial pancreas, and conventional insulin pump therapy for glycaemic control in patients with type 1 diabetes: An open-label randomised controlled crossover trial. Lancet Diabetes Endocrinol. 2015, 3 (1), 17–26. 10.1016/S2213-8587(14)70226-8. [DOI] [PubMed] [Google Scholar]
- Weinzimer S. A. Closed-loop artificial pancreas: Current studies and promise for the future. Curr. Opin. Endocrinol., Diabetes Obes. 2012, 19 (2), 88–92. 10.1097/MED.0b013e3283514e6b. [DOI] [PubMed] [Google Scholar]
- Soria B.; Gauthier B. R.; Martin F.; Tejedo J. R.; Bedoya F. J.; Rojas A.; Hmadcha A. Using stem cells to produce insulin. Expert Opin. Biol. Ther. 2015, 15 (10), 1469–1489. 10.1517/14712598.2015.1066330. [DOI] [PubMed] [Google Scholar]
- Veiseh O.; Tang B. C.; Whitehead K. A.; Anderson D. G.; Langer R. Managing diabetes with nanomedicine: Challenges and opportunities. Nat. Rev. Drug Discovery 2014, 14 (1), 45–57. 10.1038/nrd4477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tauschmann M.; Hovorka R. Insulin pump therapy in youth with type 1 diabetes: Toward closed-loop systems. Expert Opin. Drug Delivery 2014, 11 (6), 943–955. 10.1517/17425247.2014.910192. [DOI] [PubMed] [Google Scholar]
- Heinemann L.; Fleming G. A.; Petrie J. R.; Holl R. W.; Bergenstal R. M.; Peters A. L. Insulin pump risks and benefits: a clinical appraisal of pump safety standards, adverse event reporting and research needs. A Joint Statement of the European Association for the Study of Diabetes and the American Diabetes Association Diabetes Technology Working Group. Diabetologia 2015, 58 (5), 862–870. 10.1007/s00125-015-3513-z. [DOI] [PubMed] [Google Scholar]
- Kuroda K.; Takeshita Y.; Kaneko S.; Takamura T. Bending of a vertical cannula without alarm during insulin pump therapy as a cause of unexpected hyperglycemia: A Japanese issue?. Journal of Diabetes Investigation 2015, 6 (6), 739–740. 10.1111/jdi.12357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moser C.; Maurer K.; Binder E.; Meraner D.; Steichen E.; Abt D.; Freund-Unsinn K.; Hofer S. E. Needle detachment in a slim and physically active child with insulin pump treatment. Pediatric Diabetes 2016, 17, 385. 10.1111/pedi.12297. [DOI] [PubMed] [Google Scholar]
- Plager P.; Murati M. A.; Moran A.; Sunni M. Two case reports of retained steel insulin pump infusion set needles. Pediatric Diabetes 2016, 17, 160. 10.1111/pedi.12266. [DOI] [PubMed] [Google Scholar]
- Jain P. K.; Karunakaran D.; Friedman S. H. Construction of a Photoactivated Insulin Depot. Angew. Chem., Int. Ed. 2013, 52, 1404. 10.1002/anie.201207264. [DOI] [PubMed] [Google Scholar]
- Holmes C. P. Model Studies for New o-Nitrobenzyl Photolabile Linkers: Substituent Effects on the Rates of Photochemical Cleavage. J. Org. Chem. 1997, 62 (8), 2370–2380. 10.1021/jo961602x. [DOI] [PubMed] [Google Scholar]
- Agard N. J.; Prescher J. A.; Bertozzi C. R. A strain-promoted [3 + 2] azide-alkyne cycloaddition for covalent modification of biomolecules in living systems. J. Am. Chem. Soc. 2004, 126 (46), 15046–7. 10.1021/ja044996f. [DOI] [PubMed] [Google Scholar]
- Debets M. F.; van Berkel S. S.; Dommerholt J.; Dirks A. T.; Rutjes F. P.; van Delft F. L. Bioconjugation with strained alkenes and alkynes. Acc. Chem. Res. 2011, 44 (9), 805–15. 10.1021/ar200059z. [DOI] [PubMed] [Google Scholar]
- Portha B.; Blondel O.; Serradas P.; McEvoy R.; Giroix M. H.; Kergoat M.; Bailbe D. The rat models of non-insulin dependent diabetes induced by neonatal streptozotocin. Diabete Metab 1989, 15 (2), 61–75. [PubMed] [Google Scholar]
- Rini C. J.; McVey E.; Sutter D.; Keith S.; Kurth H. J.; Nosek L.; Kapitza C.; Rebrin K.; Hirsch L.; Pettis R. J. Intradermal insulin infusion achieves faster insulin action than subcutaneous infusion for 3-day wear. Drug Delivery Transl. Res. 2015, 5 (4), 332–345. 10.1007/s13346-015-0239-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L.; Zhou C.; Xia X.; Liu Y. Self-assembled lecithin/chitosan nanoparticles for oral insulin delivery: preparation and functional evaluation. Int. J. Nanomed. 2016, 11, 761–9. 10.2147/IJN.S96146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qinna N. A.; Badwan A. A. Impact of streptozotocin on altering normal glucose homeostasis during insulin testing in diabetic rats compared to normoglycemic rats. Drug Des., Dev. Ther. 2015, 9, 2515–25. 10.2147/DDDT.S79885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonaje K.; Lin K. J.; Wey S. P.; Lin C. K.; Yeh T. H.; Nguyen H. N.; Hsu C. W.; Yen T. C.; Juang J. H.; Sung H. W. Biodistribution, pharmacodynamics and pharmacokinetics of insulin analogues in a rat model: Oral delivery using pH-responsive nanoparticles vs. subcutaneous injection. Biomaterials 2010, 31 (26), 6849–58. 10.1016/j.biomaterials.2010.05.042. [DOI] [PubMed] [Google Scholar]
- Lee T. T.; Garcia J. R.; Paez J. I.; Singh A.; Phelps E. A.; Weis S.; Shafiq Z.; Shekaran A.; Del Campo A.; Garcia A. J. Light-triggered in vivo activation of adhesive peptides regulates cell adhesion, inflammation and vascularization of biomaterials. Nat. Mater. 2015, 14 (3), 352–60. 10.1038/nmat4157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dudani J. S.; Jain P. K.; Kwong G. A.; Stevens K. R.; Bhatia S. N. Photoactivated Spatiotemporally-Responsive Nanosensors of in Vivo Protease Activity. ACS Nano 2015, 9 (12), 11708–17. 10.1021/acsnano.5b05946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elisseeff J.; Anseth K.; Sims D.; McIntosh W.; Randolph M.; Langer R. Transdermal photopolymerization for minimally invasive implantation. Proc. Natl. Acad. Sci. U. S. A. 1999, 96 (6), 3104–7. 10.1073/pnas.96.6.3104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen M. J.; Velema W. A.; Lerch M. M.; Szymanski W.; Feringa B. L. Wavelength-selective cleavage of photoprotecting groups: strategies and applications in dynamic systems. Chem. Soc. Rev. 2015, 44 (11), 3358–77. 10.1039/C5CS00118H. [DOI] [PubMed] [Google Scholar]
- Sarode B. R.; Jain P. K.; Friedman S. H. Polymerizing Insulin with Photocleavable Linkers to Make Light-Sensitive Macropolymer Depot Materials. Macromol. Biosci. 2016, 16 (8), 1138–46. 10.1002/mabi.201500471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orchard T. J.; Nathan D. M.; Zinman B.; Cleary P.; Brillon D.; Backlund J. Y. C.; Lachin J. M. Association between 7 years of intensive treatment of type 1 diabetes and long-Term mortality. JAMA - Journal of the American Medical Association 2015, 313 (1), 45–53. 10.1001/jama.2014.16107. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.