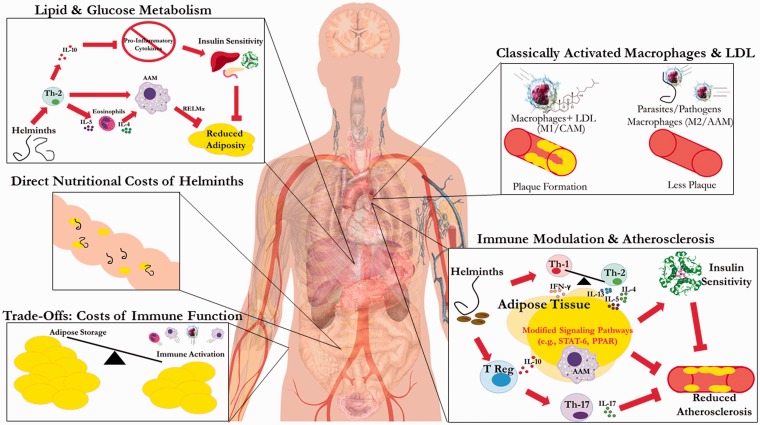
Figure 1.
Summary of mechanisms by which helminths affect CAD and T2DM. ‘Lipid and Glucose Metabolism’: Helminths promoting Th2 immune bias induce systemic elevations in eosinophils and alternatively activated macrophages (AAMs or M2), especially in white adipose tissue. AAMs producing resistin-like molecule alpha (REMα) inhibit adipogenesis, while increased anti-inflammatory cytokines (e.g. IL-10) downregulate pro-inflammatory cytokines, increasing insulin sensitivity [34]. Together these factors reduce obesity and insulin resistance, lowering risk of T2DM. Direct ‘Nutritional Costs of Helminths’: Helminths can directly consume blood lipids, but may also decrease lipid levels by inhibiting their intestinal absorption, depending on species and density of infection. ‘Trade Offs: Costs of Immune Function’: Immune activation is energetically expensive, and results in increased RMR, which can lead to less adipose storage, or possible consumption of existing adipose tissue to generate eosinophils, macrophages and other immune components. ‘Classically Activated Macrophages (CAMs) and LDL’: In hygienic populations, CAMs or M1 cluster at the site of arterial injuries and bind with LDL cholesterol, resulting in calcified lesions that progress with repeated exposure. In presence of helminths, LDL is lower, and immunity is Th2-polarized with anti-inflammatory M2 macrophages recruited to fight infection; the net effect is decreased atherosclerotic lesion progression. ‘Immune Modulation and Regulation and Atherosclerosis’: Th2-biased immunity increases AAMs and regulatory T-cells, which release cytokines (IL-4, IL-5, IL-13, IL-10) that impact signaling pathways within adipose tissue (e.g. PPAR, STAT-6). T regulatory cells inhibit Th-17 responses (e.g. IL-17), and produce other anti-inflammatory cytokines (e.g. IL-10) that result in immunomodulation disfavoring atherosclerotic lesions, plaque vulnerability or insulin resistance [35]. Note: regular arrowhead suggests promotion, whereas flat arrowhead signifies inhibition