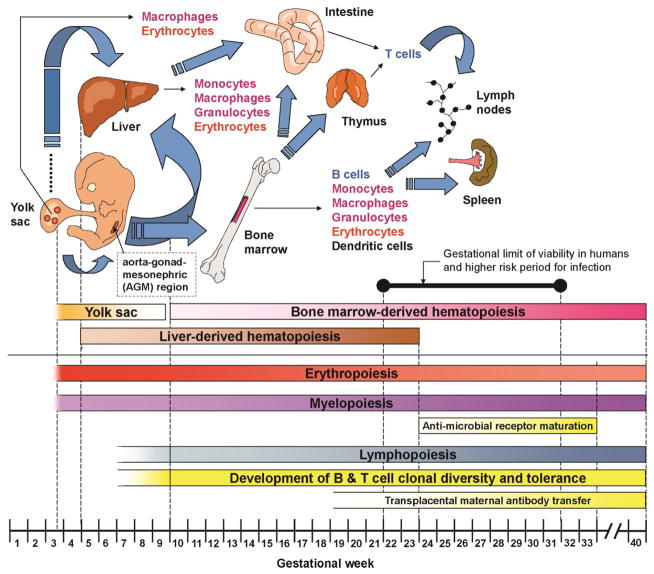
Figure 1. Immune Development during Gestation.
The development of hematopoiesis begins early in embryonic life in the yolk sac, followed by the liver, bone marrow, and other secondary hematopoietic organs. Lymphopoiesis begins after erythropoiesis and myelopoiesis. The blue arrows illustrate hematopoietic cells and their progenitors (and precursors) migrating between hematopoietic organs at different stages of embryonic and fetal life. The diagram also represents the aorta–gonad–mesonephric (AGM) region which is an important structure supporting the early colonization of hema-topoietic organs by hematopoietic cells and their progenitors. Infants born very prematurely, between 22 (defining the absolute gestational limit of viability in humans) and 32 weeks, are at high risk of infection. This period also corresponds to a critical period where substantial maturation of antimicrobial PRRs occurs, beginning with endosomal/cytoplasmic, followed by extracellular PRRs. This period also likely overlaps with the beginning of the development of mature, adult-like fetal T cells from an earlier wave of fetal T cells. Concomitant to this is the passive immunization of fetuses through trans-placental maternal antibody transfer. All these events contribute to the immaturity of the neonatal immune system in the context of a preterm birth.