Abstract
Objectives. We evaluated the impact of a comprehensive, multitiered youth suicide prevention program among the White Mountain Apache of Arizona since its implementation in 2006.
Methods. Using data from the tribally mandated Celebrating Life surveillance system, we compared the rates, numbers, and characteristics of suicide deaths and attempts from 2007 to 2012 with those from 2001 to 2006.
Results. The overall Apache suicide death rates dropped from 40.0 to 24.7 per 100 000 (38.3% decrease), and the rate among those aged 15 to 24 years dropped from 128.5 to 99.0 per 100 000 (23.0% decrease). The annual number of attempts also dropped from 75 (in 2007) to 35 individuals (in 2012). National rates remained relatively stable during this time, at 10 to 13 per 100 000.
Conclusions. Although national rates remained stable or increased slightly, the overall Apache suicide death rates dropped following the suicide prevention program. The community surveillance system served a critical role in providing a foundation for prevention programming and evaluation.
Public health scholars are shedding light on the magnitude of suicide and need for comprehensive, population-specific prevention approaches. Although suicide rates have been stable over the past decade, national data show increases in recent years (10.43/100 000 in 2000 vs 12.93, 13.00, and 13.41/100 000 in 2012, 2013, and 2014),1 with suicide deaths (n = 41 149) surpassing deaths from motor vehicle accidents (n = 35 612) in 2013.1 Youth is a heightened period of risk nationally and globally; suicide accounts for 20% of all deaths nationally among those aged 15 to 24 years,2 and despite improvements, suicide now exceeds maternal mortality as the leading cause of death among 15- to 19-year-old girls globally.3
American Indian and Alaska Native (AI/AN) persons are not only disproportionately affected by suicide, but their disparities are almost entirely concentrated among youths. From 1999 to 2004, the suicide rate for AI/AN males aged 15 to 24 years was the highest (27.99/100 000) among same-age males from other races (White = 17.54/100 000; Black = 12.80/100 000; Asian/Pacific Islander = 8.96/100 000).4 First Nations and Inuit populations in Canada are also suffering from this public health problem.5,6 In 2000, the First Nations suicide rate for all ages was 24 per 100 000 (2 times the national rate)6 and the Nunavut Inuit rate over a 15-year period was 111.4 per 100 000 (9.8 times the national rate).5 Suicide rates among Indigenous people are also known to be underestimated through racial misclassification.7 Finally, suicide rates for American Indians are often reported as national estimates, which masks marked regional differences and does not yield a clear picture for a targeted public health response.7 Although indigenous populations are one of the highest-risk groups, remarkably few suicide prevention programs have been developed among them.8,9 (For a review of AI/AN suicide prevention programs, see Middlebrook et al.10)
To address their high rates of suicide, the White Mountain Apache Tribe created a unique community surveillance system to track and triage suicide deaths, attempts, and ideation that has been used to illustrate differences between their tribe’s suicide rates and those reported by the Indian Health Service (IHS) and the Centers for Disease Control and Prevention (CDC).11–13 From 2001 to 2006, the Apache documented that their suicide rate among those aged 15 to 24 years (128.5/100 000) was 13 times the US all-races rate and 7 times the AI/AN rate.12 The ratio of suicide attempts to deaths in this age group was 36:1 from 2005 to 2006, 17 times higher than in similar studies.12
To build on the foundation of their surveillance system, the tribe was awarded several Substance Abuse and Mental Health Services Administration (SAMHSA) Garret Lee Smith grants to deliver a comprehensive youth suicide prevention program spanning universal, selected, and indicated tiers of intervention beginning in 2006. These activities are supported by a Community Advisory Board and Elders’ Council. The focus of universal activities has been to coordinate planning among local agencies and to raise community awareness. The funding supported interagency meetings and a public education campaign, including the following print materials and radio-broadcasted messages: a SAMHSA Native American Lifelines poster in a local newspaper every 2 weeks since 2008 (approximate distribution = 20 000), 8 public service announcements with a National Suicide Prevention Lifeline phone number that aired daily from 2008 to 2011, talk shows about program events with audience member call-in (monthly; approximate listenership = 10 000), and a series of 4 posters displayed in schools and tribal departments. In addition, there were biannual suicide prevention walks; 6 suicide prevention conferences; a door-to-door campaign providing information and materials about the surveillance system mandate, services, and lifeline (approximately 1600 households); a series of empowerment educational workshops reaching about 391 tribal members; and information booths at local health and tribal fairs.
The goals of selected programming were to better identify at-risk youths and increase coping skills and resiliency. Activities included the Applied Suicide Intervention Skills Training,14,15 which was open to the community, to tribal departments such as law enforcement and fire, and to emergency medical technicians, school nurses, social workers, guidance counselors, tribal leaders, and Apache Behavioral Health Services staff (approximately 136 trainees). The Sources of Strength suicide prevention program16 was also offered in 2 middle schools and to community organizations and individuals (e.g., substance use and mental health centers, Head Start, and casino employees). In addition, a coping skills curriculum, based on the American Indian Life Skills Development Curriculum, was provided to seventh to eighth graders (about 230 youths) once a week for 1 year.17 Funding also supported strengths-based and culturally based activities led by Apache elders, including quarterly field trips to sacred sites, monthly school-based workshops for kindergarten-through fifth-grade students in 3 schools, and a monthly curriculum (Elders’ Curriculum) for 2 middle schools teaching Apache culture, traditional ceremonies, identity, language, and values.
Indicated interventions targeted youths who were exhibiting suicidal ideation and attempts. Activities included a brief intervention (2–4 hours) with a powerful, locally adapted video and curriculum for youths identified by the surveillance system as having made a suicide attempt, to teach them risk reduction and motivate them to engage in services.18–20 This was followed by a multisession life skills curriculum that included a family member and taught communication, coping skills, problem-solving, goal setting, and how to connect to community resources (adapted from LaFromboise and Howard-Pitney17). The brief curriculum was also adapted for youths who came through the surveillance system for binge drinking. Finally, a community mental health specialist tried to conduct an in-person follow-up of all youths (and adults) who were reported to the surveillance system for suicidal thoughts and behavior, in order to verify their behavior, gather information, listen to their story, provide emotional support, connect them to care, and provide case management and monitoring of individuals’ welfare if needed.
We estimated changes in suicide death rates and attempts over time using surveillance system data12 to evaluate the impact of the Apache suicide prevention program. We present data on suicide death rates overall, by age and compared with those of other populations, as well as the methods and characteristics of those who died by suicide. In addition, we report the number of suicide attempts over time by age and gender, as well as the methods and characteristics of those who attempted suicide.
METHODS
The White Mountain Apache Tribe resides on the rural Fort Apache Indian Reservation, spanning 1.7 million acres in eastern Arizona. The Celebrating Life surveillance system was established by tribal resolution in 2001 and mandates that all persons, departments, and schools are responsible for reporting individuals at risk for self-injurious behaviors. The surveillance system functions as follows: an initial report is submitted describing a reportable behavior (suicide ideation, nonsuicidal self-injury, binge substance use, suicide attempt, or suicide death). The Apache Behavioral Health Services is notified and offers formal treatment services to the individual. Simultaneously, a Celebrating Life community mental health specialist seeks out the individual to complete an in-person interview to validate the initial report and facilitate linkages to and compliance with care. The Celebrating Life team reviews information from the interview and reaches consensus on final coding of the event. The consensus procedure was established in 2005 and defines attempts as “definite,” “probable,” or “possible.” Coding was based on the attempt method and documentation of intent to die from interview, medical charts, or police reports. For deaths, police reports are the primary data source.11
Surveillance data are entered into a secure, online database that is password protected and accessible only to Celebrating Life staff. Data are entered twice and validated for quality assurance. Celebrating Life staff conduct monthly reviews to check for and address missing data. They analyze trends and patterns on a quarterly, semiannual, and annual basis and reported to the Tribal Council annually. Analyses and related manuscripts are reviewed and approved by the Tribal Council and Health Advisory Board.
In this report, we describe the number and characteristics of suicide deaths and attempts from the surveillance system between January 1, 2007, and December 31, 2012. Using the same methods, we compared the 2007 to 2012 rates (suicide deaths per 100 000 per year) with previously published data from 2001 to 2006.12 Because this is a small population, we aggregated data over this 6-year period to improve the stability of the estimate. Numbers of suicide deaths and attempts (the numerators) came from the surveillance system. Numbers for the total and age-specific tribal population sizes (the denominators) came from 2007 to 2012 IHS estimates for the Whiteriver Service Unit, which serves the Fort Apache Indian Reservation. The Whiteriver Service Unit user population is limited to those who have used its services at least once in the past 3 years. To account for the younger age distribution of the Apache Tribe relative to the general US population, we calculated age-adjusted suicide rates, using the 2010 US Census population as the reference population. To ensure validity with small case numbers, we calculated confidence intervals for the suicide incidence rates based on the gamma distribution as proposed by Tiwari et al.21
We defined a suicide death as one resulting from an intentional self-inflicted injury. Police reports are the primary source for information regarding suicide deaths, validated by Bureau of Indian Affairs reports on a case-by-case basis. We defined a suicide attempt as an intentional self-injury with intent to die. Suicide attempts were validated by the individual, or by the Celebrating Life staff using available medical, police, and human service records when the person had no recollection of the event.
We compared Apache suicide rates with age-adjusted suicide incidence rates for the general US all-races population and the US White population using the most recent data from the CDC’s Web-Based Injury Statistics Query and Reporting System (WISQARS). We also compared Apache rates with national AI/AN age-adjusted suicide incidence rates for 2001 to 2008 (the most recent data available) as reported by the IHS.22
To maintain consistency with previously published results, we chose to limit the data to a 6-year time frame (2007–2012). The only exception was numbers of suicide attempts, which are often validated more closely in time to the event than deaths. We used the interviewer’s lethality rating, which assesses the likelihood of death on a scale of 1 to 10 (≤ 5 = low or no risk and ≥ 6 = could have led to death). We also used the Columbia Classification Algorithm for Suicide Assessment, which assesses actual, interrupted, and aborted attempts.23 In cases in which individuals attempted suicide more than once during the reporting period, we included the individual only once and selected the most lethal event for summary. For example, because interrupted attempts were considered less lethal than noninterrupted attempts, noninterrupted would be the index case. Characteristics of the individuals and their index events included in the analyses were age, gender, year, method, reason for act, and substance use during the event.
We analyzed all data with Stata version 14 (Stata Corp LP, College Station, TX).
RESULTS
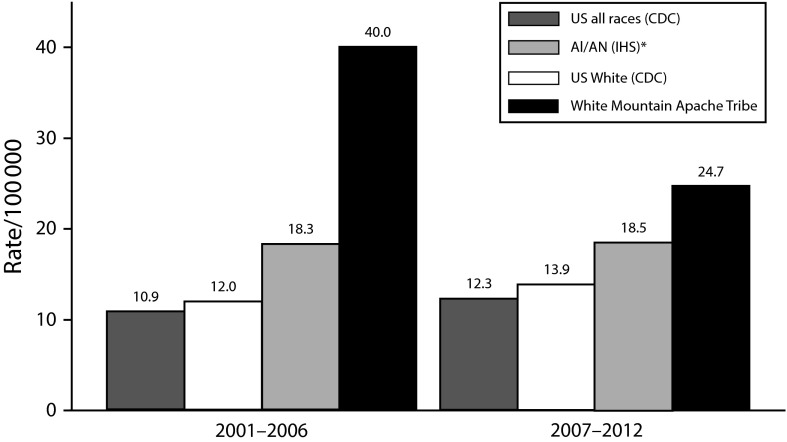
Overall suicide death rates (crude and age-adjusted) and age-specific rates per 100 000 are presented for the White Mountain Apache (Table 1). For comparison, Apache rates for the last (2001–2006) and current (2007–2012) reporting periods are displayed along with US all-races, US White, and all AI/AN referent population rates (Figure 1). Overall, Apache suicide death rates dropped from 40.0 to 24.7 per 100 000, a 38.3% decrease. These rates represent the loss of 41 and 29 Apache tribal members from 2001 to 2006 and from 2007 to 2012, respectively. During this 12-year period, national suicide rates remained stable. From 2001 to 2012, the rate ratio of suicide deaths among Apache persons compared with the United States (all races) decreased from 3.7 to 2.1; compared with all AI/AN persons, it decreased from 3.9 to 2.4.
TABLE 1—
Suicide Death Rates Among the White Mountain Apache: Arizona, 2001–2012
| Suicide Incidence Rate (per 100 000) (95% CI) |
|||
| 2001–2006 | 2007–2012 | % Change | |
| Age group, y | |||
| Birth–4 | 0 | 0 | . . . |
| 5–9 | 0 | 0 | . . . |
| 10–14 | 17.1 (2.1, 61.6) | 23.6 (2.9, 85.3) | 38.0 |
| 15–19 | 107.8 (53.8, 192.8) | 101.9 (48.9, 187.4) | −5.5 |
| 20–24 | 151.9 (78.5, 265.2) | 96.0 (43.9, 182.2) | −36.8 |
| 25–34 | 95.0 (47.4, 169.9) | 37.9 (12.3, 88.4) | −60.1 |
| 35–44 | 23.3 (4.8, 68.2) | 9.1 (0.2, 50.6) | −60.9 |
| 45–64 | 15.5 (1.9, 56.2) | 11.7 (1.4, 42.3) | −24.5 |
| ≥ 65 | 0 | 0 | . . . |
| Total (all ages) | |||
| Crude | 45.5 (32.7, 61.7) | 30.3 (19.3, 41.3) | −33.4 |
| Age adjusted | 40.0 (27.8, 52.1) | 24.7 (16.3, 36.2) | −38.3 |
Note. CI = confidence interval. Ellipses indicate not calculable.
FIGURE 1—
Suicide Death Rates per 100 000 for US All Races, US Whites, American Indians/Alaska Natives, and Apache Populations: 2001–2006 and 2007–2012
Note. AI/AN = American Indian/Alaska Native; IHS = Indian Health Service; CDC = Centers for Disease Control and Prevention.
Apache suicide rates decreased in every age group except for those aged 10 to 14 years (17.1–23.6/100 000). During both reporting periods, there were 2 deaths in this age group, but because of population changes, the rates differ. The age groups with the most change were ages 25 to 34 years (from 95.0 to 37.9/100 000, a 60% decrease) and 20 to 24 years (from 151.9 to 96/100 000, 37% decrease). For SAMHSA’s Garret Lee Smith grant target population (youths aged 15 to 24), the suicide rate decreased from 128.5 to 99.0 per 100 000, a 23% decrease.
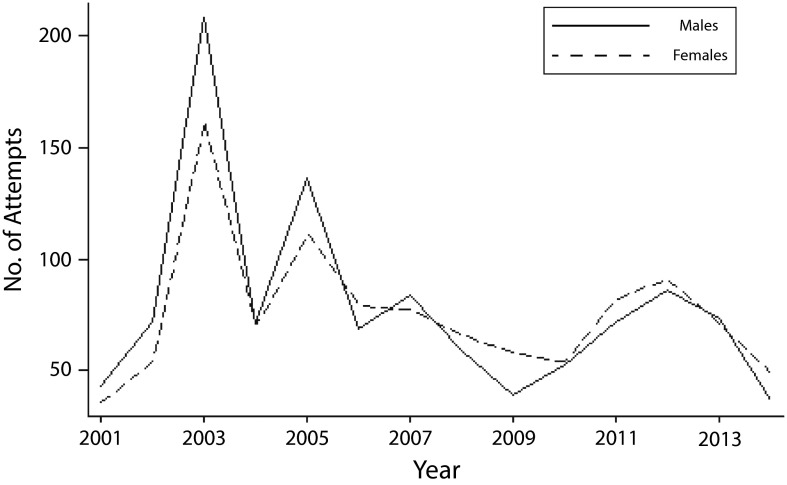
From 2007 to 2012, there were 433 attempts (366 individuals) reported to the surveillance system. Approximately 69% of attempts (299/433) were by youths younger than 25 years. Despite some fluctuations, the pattern appears to represent a general overall downward trend, with a similar number of attempts and relative decreases for males and females from 2001 to 2014 (Figure 2). The annual number of attempts also decreased from 75 individuals in 2007 to 35 in 2012 (Table 2).
FIGURE 2—
Suicide Attempts Among Males and Females Over Time in the Apache Suicide Surveillance System: Arizona, 2001–2014
TABLE 2—
Characteristics of Suicide Deaths and Attempts Captured in the Apache Suicide Surveillance System: Arizona, 2007–2012
| Characteristic | Deaths, No. (%) | Attempts, No. (%) |
| Year of event | ||
| 2007 | 3 (10) | 75 (20) |
| 2008 | 2 (7) | 78 (21) |
| 2009 | 10 (34) | 58 (16) |
| 2010 | 2 (7) | 62 (17) |
| 2011 | 4 (14) | 58 (16) |
| 2012 | 8 (28) | 35 (10) |
| Gender | ||
| Male | 19 (66) | 172 (47) |
| Female | 10 (34) | 194 (53) |
| Age group, y | ||
| Birth–4 | 0 (0) | 0 (0) |
| 5–9 | 0 (0) | 2 (< 1) |
| 10–14 | 2 (7) | 53 (14) |
| 15–19 | 10 (34) | 134 (37) |
| 20–24 | 9 (31) | 63 (17) |
| 25–29 | 5 (17) | 53 (14) |
| 30–34 | 0 (0) | 26 (7) |
| 35–39 | 1 (3) | 14 (4) |
| 40–44 | 0 (0) | 9 (2) |
| 45–49 | 2 (7) | 5 (1) |
| 50–54 | 0 (0) | 4 (1) |
| 55–59 | 0 (0) | 3 (< 1) |
| Method used | ||
| Overdose | 1 (3) | 161 (44) |
| Hanging | 26 (90) | 106 (29) |
| Laceration or cut | 0 (0) | 52 (14) |
| Jump | 1 (3) | 25 (7) |
| Firearm | 1 (3) | 9 (3) |
| No info from this source | 0 (0) | 13 (34) |
| Individual drunk or high at the time of incident (not mutually exclusive) | ||
| Yes (any substance) | 17 (59) | 268 (73) |
| Alcohol | 17 (59) | 204 (56) |
| Marijuana and alcohol | 0 (0) | 21 (6) |
| Marijuana, no alcohol | 0 (0) | 4 (1) |
| Cocaine | 0 (0) | 9 (2) |
| Methamphetamine | 0 (0) | 4 (1) |
| Other drugs | 0 (0) | 10 (3) |
| Unknown | 6 (21) | |
| Reason for act | ||
| Can’t remember (includes intoxicated or blacked out) | 1 (3) | 78 (21) |
| Fight or argument with parent or relative | 11 (38) | 67 (18) |
| Fight or argument with boyfriend, girlfriend, or spouse | 7 (24) | 55 (15) |
| Depression | 1 (3) | 47 (13) |
| Family or home problems | 0 (0) | 28 (8) |
| Stress or a lot on the mind | 0 (0) | 25 (7) |
| Suicide or death of loved one, friend, or relative | 0 (0) | 18 (5) |
| Unknown | 1 (3) | 16 (4) |
| No reason | 0 (0) | 9 (3) |
| Fight with other, including bullying | 0 (0) | 8 (2) |
| Other | 1 (3) | 7 (2) |
| Trouble with the law | 0 (0) | 2 (< 1) |
| Peer pressure or copying | 0 (0) | 2 (< 1) |
| Divorce or separation | 0 (0) | 1 (< 1) |
| Loss of job | 0 (0) | 1 (< 1) |
| Trouble at school | 0 (0) | 1 (< 1) |
| Refused to answer | 7 (24) | 1 (< 1) |
Note. There were a total of 29 suicides and 433 suicide attempts among 366 individuals. If an individual had multiple events in the registry, we selected actual attempts over interrupted attempts, and the most lethal for summary here.
Twenty-one of the 29 deaths (72%) were among people younger than 25 years (mean = 22.6; SD = 8.9; median = 20). Hanging was the predominant suicide method at 90%, up from 80% for the period 2001 to 2006. Nineteen were male (66%) and 10 were female (34%), representing a larger percentage of the deaths occurring among females during this reporting period than in the prior period (15%). Among those aged 25 years or younger, female deaths (n = 4) increased from 16% of all suicide deaths in the period 2001 through 2006 to 44% (n = 10) in 2007 through 2012. For all ages, the majority of individuals were reportedly using alcohol at the time (n = 17; 59%) and experiencing interpersonal conflict (n = 18; 62%). Almost half (n = 14; 48%) had children, with a larger number of females (6 of 10; 60%) than males (8 of 19; 42%) reported to be parents. From 2001 to 2006, only 2 of 41 (5%), both of whom were male, were known to have had children. By year, suicide deaths fluctuated greatly over time (range = 2–10 per year).
Attempts were highest among those aged 15 to 19 years (n = 134; 37%), followed by those aged 20 to 24 years (n = 63; 17%), with an average age of 22.6 years (SD = 8.9; median = 19.8). The male-to-female ratio was close to 1:1 (males, n = 172 [47%]; females, n = 194 [53%]), similar to the ratio in the earlier time frame. The most common attempt methods were overdose (n = 161; 44%), hanging (n = 106; 29%), and laceration or cutting (n = 52; 14%). Almost three fourths (n = 268; 73%) self-reported that they were using substances at the time. More than half (56%) were using alcohol and 7% were using marijuana. The most commonly reported reasons were (1) can’t remember (n = 78; 21%), (2) conflict with family members (n = 67; 18%), (3) conflict with boyfriend or girlfriend (n = 55; 15%), and (4) depression (n = 47; 13%).
DISCUSSION
These data provide evidence that the White Mountain Apache suicide surveillance and prevention system reduced suicide deaths and attempts among adolescents, young adults, and adults. The tribally mandated surveillance system was critical to prevention, intervention, and evaluation. Whereas other national statistics remain unchanged or are increasing, Apache age-adjusted overall suicide rates have decreased by 38% (from 40.0/100 000 to 24.7/100 000). This effect was even more pronounced among young adults and adults, with a 60% drop among the 25- to 34-year-old group and a 37% drop among those aged 20 to 24 years. Suicide attempts also decreased—from 75 and 78 in 2007 and 2008, respectively, to 35 in 2012—for a population of 17 500 enrolled members.
These innovative data—from an initial period of strict surveillance that allowed the Apache to fund their comprehensive program to a period of intensive interventions—provide a unique opportunity for a natural experiment that allows comparison of rates from pre- to postimplementation. Other recent findings have provided preliminary evidence that a multitiered public health approach can have measurable effects in high-risk groups.24–27 For example, May et al.25 evaluated another comprehensive tribal program and showed significant decreases (73%) in the number of suicide gestures and attempts from 1988 (n = 72) to 2002 (n = 14), but not in deaths. (Their numbers of suicides remained small and steady over time, ranging from 2 to 4 per year.) The US Air Force Suicide Prevention Program evidenced drops in average quarterly suicide rates using data from 1981 to 2008 (2.4/100 000 during implementation vs 3.0/100 000 before; P < .01).24 Counties that implemented SAMHSA-funded gatekeeper training (states and AI/AN tribes) had 1.33 fewer deaths per 100 000 for ages 10 to 24 years from 2006 to 2009 than matched counties.26
Several other unique findings are worthy of further exploration. First, rates decreased in every age group except for those aged 10 to 14 years. This finding could be attributable to chance variation in a small sample (2 for both periods). However, other national data suggest that rates may be going up in this age range in certain subpopulations. Bridge et al.28 showed that young Black males, aged 5 to 11 years, were at increasing risk for suicide death (1993–1997 vs 2008–2012). Second, despite a slight decrease over their 2 reporting periods (from 107.8 to 101.9/100 000), Bridge et al.28 reported that the highest incidence of death and attempts was for youths aged 15 to 19 years, which calls for continued and creative prevention approaches.
The age group with the greatest positive change was those aged 20 to 44 years; we are possibly observing a cohort effect among those aged 20 to 24 years, who as adolescents were exposed to prevention interventions and then aged into young adulthood. In addition, the program trained large numbers of adults in Applied Suicide Intervention Skills Training and exposed them to widespread prevention training and media messaging.
Apache women, particularly young mothers, seem to be at increased risk, with 60% of females (6 of 10) who died reported to be parents. In addition, the male-to-female death ratio across all ages decreased from 5:1 to 2:1 across the 2 reporting periods, whereas nationally, this ratio stayed fairly constant at 4:1 from 2001 to 2012.1 It appears that the protective effect of having children is now outweighed by the challenges of young motherhood, coupled with a lack of coping skills and interpersonal conflict. The effects on the surviving children are a public health concern that must be addressed through future intervention. An alternative hypothesis is that our comprehensive program was more successful with males. Finally, deaths appear to follow a cyclical pattern, with “peaks” appearing every 3 years; longitudinal data in this and other American Indian communities would allow for further exploration of this potential trend.
Limitations
The study has several limitations. First, because this evaluation is not a randomized controlled trial, we cannot definitively conclude that the decrease in deaths and attempts is attributable to the Apache’s suicide prevention activities. The longitudinal and rigorous nature of the surveillance data combined with the timing of implementation, however, provide strength to the association between programming and outcomes. Furthermore, there are no other plausible hypotheses for the decrease (e.g., no other communitywide initiatives launched during this time or major sociodemographic or economic changes). Second, the Apache program has multiple parts and the individual effects of each cannot be dismantled; therefore, it is difficult to know what components are the most impactful. Third, even with aggregate data, our sample size was small and vulnerable to fluctuations, especially when broken down by age, making it difficult to demonstrate significant differences between the 2 periods. Fourth, the Whiteriver Service Unit user population is limited to those who have used its services at least once in the past 3 years, so the denominators in our rate calculations may be underestimates of the true total population.
Public Health Implications
This study provides clarity on areas of focus for comprehensive suicide intervention and prevention programs in this and other AI reservations with similar characteristics. The use of hanging in Apache suicide deaths increased from 80% to 90% over our study period (2001–2006 vs 2007–2012), whereas from 2007 to 2012, firearms accounted for approximately half (51%) of all US suicides, followed by suffocation or hanging (24%).1 Of note, most Apache homes have firearms, but they tend to be hunting rifles rather than handguns. As a result, restricting access to firearms in this community would not be an effective strategy, and restricting means of suicide by hanging (i.e., belts, cords, laces, and rope) is not a viable strategy because these materials are ubiquitous. Further, alcohol use co-occurred in more than half of all deaths and attempts. The role of alcohol demands further exploration—does it disinhibit the individual from fears or considerations that would protect from suicide? Is it used with this purpose or is it part of a larger risk profile? The most predominant specific triggers for both suicide death and attempts are fights with parents, relatives, or boyfriends or girlfriends. It is unclear how interpersonal conflict may interact with alcohol use. The focus of the Apache prevention efforts on coping and problem-solving skills seems well placed. However, there is continued need for research and interventions to build healthy intimate and familial relationships. The study team is currently conducting a social network analysis to study how interpersonal relationships, including conflict, influence Apache youths’ engagement in high-risk behaviors.
The fact that there were no deaths among individuals older than 49 years may indicate protective factors associated with older ages and traditional Apache cultural values. This highlights the continued importance of our Elders’ Curriculum, a resilience-focused, culturally based intervention for middle school students delivered by Apache elders. By contrast, suicide deaths in the general US population are most prevalent among males aged 45 years and older.2 The community’s decision to include elders in the advisory board guiding the suicide prevention program development and, more recently, to implement an Elders’ Curriculum focused on culturally driven protective factors identified by previous studies29–31 that targets the 10- to 15-year age group, is well supported by these data.
Conclusions
The current analysis makes a unique and innovative contribution to the suicide prevention field because of the accuracy, quality, and depth of local data that has been gathered since 2001, blended with the longevity of the comprehensive program driven by community needs and public health principles. The community surveillance system served a critical role in providing a foundation for prevention programming and evaluation.
ACKNOWLEDGMENTS
We are grateful to the Native American Research Centers in Health (NARCH) initiative, which provided grant support for the surveillance system from the National Institute of General Medical Science and Indian Health Service (grants U26IHS300013, U26IHS300286, and U26IHS300414; study principal investigators [PIs], J. W. and M. F. C, respectively; NARCH PI, Mariddie Craig) and the Substance Abuse and Mental Health Services Administration youth suicide prevention initiative (grants U79SM057835, U79SM059250, and U79SM061473; study PIs, J. W., A. B., and M. F. C, respectively).
This report honors the White Mountain Apache Tribe, Tribal Council and Health Board for their courage in addressing suicide and innovation in mandating community-based surveillance and implementing a comprehensive public health approach. We acknowledge the Apache Celebrating Life team for their tireless dedication to help their community. We also thank our SAMHSA program officer, Richard McKeon.
Note. The opinions expressed are those of the authors and do not necessarily reflect the views of the Indian Health Service or the Substance Abuse and Mental Health Services Administration.
HUMAN PARTICIPANT PROTECTION
The surveillance system is tribally mandated, which is the equivalent of human participants' approval. Analyses in this article are covered under this approval.
REFERENCES
- 1.Centers for Disease Control and Prevention. Web-based injury statistics query and reporting system (WISQARS). Updated 2005. Available at: http://www.cdc.gov/injury/wisqars. Accessed September 14, 2016.
- 2.CDC National Center for Injury Prevention and Control, Division of Violence Prevention. Suicide facts at a glance, 2012. Available at: https://stacks.cdc.gov/view/cdc/21865. Accessed September 14, 2016.
- 3.Health for the World’s Adolescents. A Second Chance in the Second Decade. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 4.Ensuring the Seventh Generation: Youth Suicide Prevention Toolkit. Portland, OR: National Indian Child Welfare Association; 2009. [Google Scholar]
- 5.Hicks J. Statistical data on death by suicide by Nunavut Inuit, 1920 to 2014. 2015. Available at: http://www.tunngavik.com/files/2015/09/2015-09-14-Statistical-Historical-Suicide-Date-Eng.pdf. Accessed September 14, 2016.
- 6.Minister of Public Works and Government Services. The Human Face of Mental Health and Mental Illness in Canada. Ottawa: Government of Canada; 2006. Chapter 12: Aboriginal mental health and well-being; pp. 159–179. [Google Scholar]
- 7.Herne MA, Bartholomew ML, Weahkee RL. Suicide mortality among American Indians and Alaska Natives, 1999–2009. Am J Public Health. 2014;104(suppl 3):S336–S342. doi: 10.2105/AJPH.2014.301929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wexler L, Chandler M, Gone JP et al. Advancing suicide prevention research with rural American Indian and Alaska Native populations. Am J Public Health. 2015;105(5):891–899. doi: 10.2105/AJPH.2014.302517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gray JS, McCullagh JA. Suicide in Indian country: the continuing epidemic in rural Native American communities. J Rural Ment Health. 2014;38(2):79–86. [Google Scholar]
- 10.Middlebrook DL, LeMaster PL, Beals J, Novins DK, Manson SM. Suicide prevention in American Indian and Alaska Native communities: a critical review of programs. Suicide Life Threat Behav. 2001;31(suppl):132–149. doi: 10.1521/suli.31.1.5.132.24225. [DOI] [PubMed] [Google Scholar]
- 11.Cwik MF, Barlow A, Goklish N et al. Community-based surveillance and case management for suicide prevention: an American Indian tribally initiated system. Am J Public Health. 2014;104(suppl 3):e18–e23. doi: 10.2105/AJPH.2014.301872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mullany B, Barlow A, Goklish N et al. Toward understanding suicide among youths: results from the White Mountain Apache tribally mandated suicide surveillance system, 2001–2006. Am J Public Health. 2009;99(10):1840–1848. doi: 10.2105/AJPH.2008.154880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tingey L, Goklish N, Larzelere-Hinton F et al. The White Mountain Apache model for suicide and self-injury surveillance and prevention: innovation in public health. IHS Prim Care Provid. 2013;38(1):1–4. [Google Scholar]
- 14.Ramsay R, Tanney B, Tierney R, Land W. ASIST(Applied Suicide Intervention Skills Training) trainer’s manual. 1999. Available at: https://www.livingworks.net/assets/Assets/Programs/ASIST/ASIST-review2010.pdf. Accessed September 14, 2016.
- 15.Cwik MF, Tingey L, Wilkinson R, Goklish N, Larzelere-Hinton F, Barlow A. Suicide prevention gatekeeper training: can they advance prevention in Indian country? Arch Suicide Res. 2016;20(3):402–411. doi: 10.1080/13811118.2015.1033122. [DOI] [PubMed] [Google Scholar]
- 16.Wyman PA, Brown CH, LoMurray M et al. An outcome evaluation of the sources of strength suicide prevention program delivered by adolescent peer leaders in high schools. Am J Public Health. 2010;100(9):1653–1661. doi: 10.2105/AJPH.2009.190025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.LaFromboise T, Howard-Pitney B. The Zuni life skills development curriculum: description and evaluation of a suicide prevention program. J Couns Psychol. 1995;42(4):479–486. [Google Scholar]
- 18.Cwik MF, Tingey L, Lee A et al. Development and piloting of a brief intervention for suicidal American Indian adolescents. Am Indian Alsk Native Ment Health Res. 2016;23(1):105–124. doi: 10.5820/aian.2301.2016.105. [DOI] [PubMed] [Google Scholar]
- 19.Asarnow JR, Baraff LJ, Berk M et al. An emergency department intervention for linking pediatric suicidal patients to follow-up mental health treatment. Psychiatr Serv. 2011;62(11):1303–1309. doi: 10.1176/appi.ps.62.11.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rotheram-Borus MJ, Piacentini J, Van Rossem R et al. Enhancing treatment adherence with a specialized emergency room program for adolescent suicide attempters. J Am Acad Child Adolesc Psychiatry. 1996;35(5):654–663. doi: 10.1097/00004583-199605000-00021. [DOI] [PubMed] [Google Scholar]
- 21.Tiwari RC, Clegg LX, Zou Z. Efficient interval estimation for age-adjusted cancer rates. Stat Methods Med Res. 2006;15(6):547–569. doi: 10.1177/0962280206070621. [DOI] [PubMed] [Google Scholar]
- 22.Indian Health Service. Trends in Indian Health. Vol. 2015. Rockville, MD: US Dept of Health and Human Services; 2014. Table 4.21: suicide deaths and death rates; p. 74. [Google Scholar]
- 23.Posner K, Oquendo MA, Gould M, Stanley B, Davies M. Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA’s pediatric suicidal risk analysis of antidepressants. Am J Psychiatry. 2007;164(7):1035–1043. doi: 10.1176/appi.ajp.164.7.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Knox KL, Pflanz S, Talcott GW et al. The US Air Force suicide prevention program: implications for public health policy. Am J Public Health. 2010;100(12):2457–2463. doi: 10.2105/AJPH.2009.159871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.May PA, Serna P, Hurt L, Debruyn LM. Outcome evaluation of a public health approach to suicide prevention in an American Indian tribal nation. Am J Public Health. 2005;95(7):1238–1244. doi: 10.2105/AJPH.2004.040410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walrath C, Garraza LG, Reid H, Goldston DB, McKeon R. Impact of the Garrett Lee Smith Youth Suicide Prevention Program on suicide mortality. Am J Public Health. 2015;105(5):986–993. doi: 10.2105/AJPH.2014.302496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Godoy Garraza L, Walrath C, Goldston DB, Reid H, McKeon R. Effect of the Garrett Lee Smith Memorial Suicide Prevention Program on suicide attempts among youths. JAMA Psychiatry. 2015;72(11):1143–1149. doi: 10.1001/jamapsychiatry.2015.1933. [DOI] [PubMed] [Google Scholar]
- 28.Bridge JA, Asti L, Horowitz LM et al. Suicide trends among elementary school-aged children in the United States from 1993 to 2012. JAMA Pediatr. 2015;169(7):673–677. doi: 10.1001/jamapediatrics.2015.0465. [DOI] [PubMed] [Google Scholar]
- 29.Cwik M, Barlow A, Tingey L et al. Exploring risk and protective factors with a community sample of American Indian adolescents who attempted suicide. Arch Suicide Res. 2015;19(2):172–189. doi: 10.1080/13811118.2015.1004472. [DOI] [PubMed] [Google Scholar]
- 30.Tingey L, Cwik MF, Goklish N et al. Risk pathways for suicide among Native American adolescents. Qual Health Res. 2014;24(11):1518–1526. doi: 10.1177/1049732314548688. [DOI] [PubMed] [Google Scholar]
- 31.Tingey L, Cwik M, Goklish N et al. Exploring binge drinking and drug use among American Indians: data from adolescent focus groups. Am J Drug Alcohol Abuse. 2012;38(5):409–415. doi: 10.3109/00952990.2012.705204. [DOI] [PubMed] [Google Scholar]