Abstract
Background:
In congenital adrenal hyperplasia (CAH) with ambiguous genitalia, assigning gender of rearing can be complex, especially If genitalia is highly virilized. Apart from karyotype, prenatal androgen exposure, patient's gender orientation, sociocultural, and parental influences play a role. The aim of this study was to assess gender dysphoria and psychosocial issues in patients of CAH raised as males and females.
Materials and Methods:
This is a cross-sectional study that includes patients (old and new) with CAH who were treated by us in the last 6 months. A semi-structured interview proforma was used to elicit history and psychosocial background of the patients. The clinical and biochemical details were noted. For psychological analysis, patients were screened for gender dysphoria using Parent Report Gender Identity Questionnaire for children <12 years and Gender Identity/Gender Dysphoria Questionnaire for Adolescents and Adults.
Results:
We analyzed 22 46 XX CAH patients among which, 3 were reared as males and 19 as females. Among the 19 patients reared as females, 17 patients showed no gender dysphoria. Two patients revealed gender dysphoria as indicated by their marginally low scores on the gender dysphoria assessment. However, in view of current literature and the age groups of the patients, behavior of the 6-year-old patient can be best understood as being tomboyish. Gender dysphoria in the 22-year-old can be explained by the dominance of psychosocial factors and not hormones alone. Among the three patients reared as males, two prepubertal were satisfied with their male gender identity. The third patient, aged 32 years, had gender dysphoria when reared as a male that resolved when gender was reassigned as female and feminizing surgery was done.
Conclusion:
Gender assignment in 46 XX CAH is guided by factors such as degree of virilization of genitalia, gender orientation, patient involvement, sociocultural, and parental influences.
Key words: Ambiguous genitalia, congenital adrenal hyperplasia, gender dysphoria
INTRODUCTION
For patients of congenital adrenal hyperplasia (CAH) with ambiguous genitalia (AG), the decision of gender assignment and sex of rearing can be complex, especially if the genitalia are highly virilized. While assigning gender, apart from karyotype and prenatal androgen exposure, sociocultural influences, and parental expectations play a role.
There have been debates on the role of gender in shaping an individual's mode of functioning – nature (pre- and post-natal androgen exposure, genetics) versus nurture (sex of rearing, parenting style). However, sex of rearing has been considered a promising predictor of an individual's gender identity.[1] Since gender is conventionally divided as being either a male or a female, unacceptability can arise if it lies in-between these two points.[2]
Being labeled “queer” or a transgender can become a major source of distress for the patients and their family. It can result in the individual being ostracized from all socio-familial events. One-third of 46 XX patients with disorders of sexual differentiation (DSD) tend to experience gender dissonance [3] with their biological sex.
Most of the 46 XX CAH patients raised as females tend to retain their chromosomal gender identity throughout their lives. However, one study reported that 10 out of 217 females, diagnosed with CAH and reared as women, showed some form of gender dissonance or identity confusion.[4,5] The difficulty in assigning gender particularly arises if the genitalia of the new-born patient is highly virilized. A literature review assessed studies on gender dysphoria and gender confusion in patients with 46 XX CAH reared as females. The majority of the patients carried forward their female gender identity in adulthood. A minute number (5.2%) reported dissatisfaction with their female gender. Hence, the authors concluded the need for assignment of female gender identity in CAH patients even in the face of highly virilized genitalia (Prader Stage IV or V).[6] However, there have been reports of successful male gender assignment in patients with 46 XX CAH and highly virilized genitalia, who have demonstrated adequate social and sexual functioning as males. These reports have challenged the notion of typically relying on internal genitalia (presence of uterus and ovaries) while assigning gender in these patients.[7,8] Thus the decision to rear 46XXCAH patients as male or female needs to be based on several factors.
Psychological assessment of patients with 46 XX CAH serves three major purposes. First, it helps gain insight about the distress experienced by the patient and their family. Second, it would help in understanding the impact of their distress on different facets of their lives. Third, it helps in determining their coping strategies. Hence, this study aims to gain insight into the psychosocial functioning, gender rearing, and gender dysphoria in patients of 46 XX CAH in Indian setup.
MATERIALS AND METHODS
This is a cross-sectional study in which patients of 46 XX CAH were enrolled. A diagnosis of CAH was made on the basis of history and examination, cytogenetic and hormonal analysis. Cytogenetic studies confirmed the karyotype as 46 XX. Diagnosis of salt-wasting CAH (SW-CAH) was made on the basis of genital ambiguity with history of diarrhea/vomiting in infancy with electrolyte imbalance, hypokalemia, and elevated 17-hydroxyprogesterone (OHP) levels. Diagnosis of simple virilizing CAH (SV-CAH) was made on the basis of the presence of AG/clitoromegaly with elevated 17 OHP levels without a history of salt wasting. Patients who presented at puberty with features of irregular periods, acne, hirsutism, and raised 17 OHP levels, a diagnosis of nonclassical CAH (NC-CAH) was made. Twenty-two patients diagnosed with 46 XX CAH were recruited from endocrinology OPD. Ethical clearance was obtained from the Institute Ethics Committee.
A semi-structured interview proforma was used to elicit history and psychosocial background of the patients. The clinical and biochemical details were noted. For psychological analysis, the patients were divided into two groups. The first group comprised children from 2.5 to 12 years. The second group comprised adolescents (12–18 years) and adults. All the 22 patients were screened for gender dysphoria using:
Parent Report Gender Identity Questionnaire (PR-GIQ) for Children [9] is a parent report assessment of problems in the gender identity development of children aged 2.5–12 years. For this purpose, parents are asked to 16 questions that cover a range of sex-typical behaviors of each gender. Each item is rated on five point scale on frequency of occurrence. Lower scores reflect more cross-gendered behavior. A mean score of 2.87 or below for boys and 2.67 or below for girls indicates the presence of gender dysphoria. This test offers excellent psychometric properties with negligible age effects. Specificity rate is 95% for the controls, and sensitivity rate for the probands is 86.8%
Gender Identity/Gender Dysphoria Questionnaire for Adolescents and Adults (GIDAA)[10] is an assessment tool used on adolescents and adults to assess gender dysphoria. It can be self-administered and consists of 27 questions. Each item is rated on a five point scale on the frequency of occurrence. A mean score of three or below indicates the presence of gender dysphoria. It displays a strong discriminant validity of 0.97 (Cronbach alpha coefficient) with 90.4% sensitivity for the gender identity patients and specificity of 99.7% for the controls.
To assess gender dysphoria, PR-GIQ was administered on the parents of patients who were 12 years of age and below. GIDAA was administered on patients who were above 12 years of age. The male version of these tests was used on patients reared as males and female version for those reared as females.
Since the patients were fluent in Hindi, the two questionnaires - PR-GIQ for children and GIDAA were translated in Hindi and back translated.
RESULTS
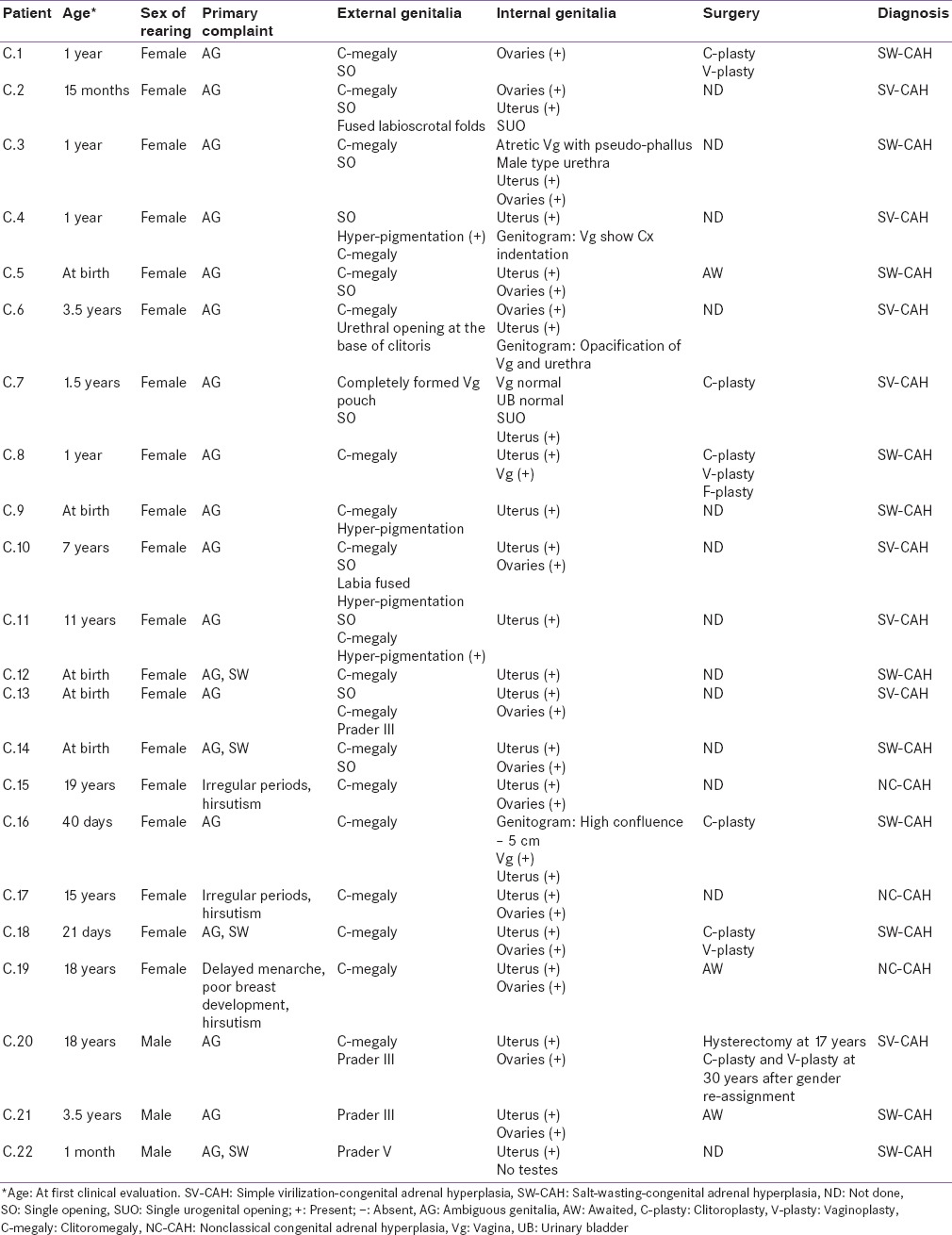
Age at first evaluation ranged from 3.5 to 32 years. Nineteen patients were reared as females and 3 as males. Table 1 summarizes the clinical presentation and diagnosis of patients. There were 11 patients with SW-CAH and 8 patients with SV-CAH and 3 with NC-CAH.
Table 1.
Clinical profile and diagnosis of patients
Among the 19 patients reared as females, most were well-adjusted as females and did not have gender dysphoria. Two patients showed marginally low scores for gender dysphoria by the tests applied [Table 2]. First patient, C.4, aged 6 years old, was being reared as a female and expressed her desire to be a boy. Since her score on PR-GIQ was marginally on the lower side, Draw-A-Person-Test (DAPT)[11] was performed on her to ascertain the extent of dissonance in her gender identity. DAPT is a projective test in which a subject is asked to draw a figure of anyone and any gender they like. DAPT has been extensively used to assess the cognitive and psychological characteristics of children and adults. According to the projective school of thought, drawings are assumed to be symbolic representations of the things in the unconscious that is usually suppressed. In general, drawing tests require no prior training and are often used as icebreakers as they help to reduce the anxiety of the child.[12] Our patient drew a figure of a 5-year-old boy named “Muni.” On questioning, Muni was the name of the patient's cousin she liked playing with. Since it was an opposite sex figure, it may point toward ambivalence or conflict regarding her sexual identity. Although, the validity of this test is often questioned as its interpretations are subjective and qualitative in nature. However, atypical drawings can be seen as strong indicators of maladjustment in an individual.
Table 2.
Gender dysphoria test findings

The second patient C.16, reared as a female in whom gender dysphoria was found by the tests applied, was aged 22. Though she was reared as a female, she wished to live as a male. On further enquiry, the patient showed depressive symptoms with inadequate sleep, reduced hunger, weight loss, and She also exhibited a very low self-esteem and body image disturbances. She was assessed by a psychiatrist, following which she was diagnosed with sub-syndromal depression under remission. She was advised to take psychiatric treatment to improve her condition.
Among the three patients reared as males, genitalia were Prader Grade III or V [Table 1]. Gender dysphoria was found in none at the time of this study [Table 2]. Among them, the first patient, C.20, aged 32, had successfully undergone gender reassignment as a female 2 years before this study was conducted and at present is living as a woman. Therefore female version of gender dysphoria score was applied. The second patient, C.21, aged 12, sought clearance for panhysterectomy before entering puberty. The third patient, C.22, aged 8 years, was satisfied with his male gender identity and had clearly stated to remain a boy. He had been admitted 2 years back for feminizing genitoplasty after counseling his parents about his chromosomal sex being female. However, the patient refused to undergo the surgery as he was completely satisfied in being a boy.
DISCUSSION
Majority of patients reared as females (17 out of 19) were well-adjusted. Out of the patients reared as female, two patients, C.16 and C.4 showed gender dysphoria by the scales applied. Patients C.16 and C.4, aged 22 and 6, reared as girls, were unsatisfied with their female gender identity. They like to dress themselves as males (pants and shirt) and enjoy male associated activities.
Mother of patient C.4 reported scolding the patient when she referred to herself as a boy. However, research has indicated that some behaviors of girls with CAH can be tomboyish, hence, it may not indicate a dissonance in the core gender identity. In a study, a prenatally hyperandrogenized sample of young girls with CAH did not show any masculinization of gender identity.[13] The drawing of an opposite sex figure on DAPT by the 6 year old C.4 also does not necessarily point toward gender dysphoria or emotional issues. If the child's drawing is neither typically male nor female, it may point towards some maladjustment. Undefined sex could be seen as an indicator of psychological difficulties or maladjustment.[14] Hence, for patient C.4, surgical procedures have been postponed until she attains puberty when she will be reassessed. Since she does not meet the criteria for gender identity disorder in childhood according to guidelines in ICD-10,[15] her behavior can be best viewed under the lens of being tomboyish.
Due to familial and social pressure, the second patient C.16 with gender dysphoria, aged 22, has not disclosed the dissonance in her gender identity to anyone. She has attempted to harm herself physically in the past due to being teased by her peers. As revealed by the patient's sister, she disliked her body and often doubted herself. This may have contributed to the patient not having any social circle, inadequate sleep cycle with anxiety and reduced hunger. The stress of her medical condition may have further led her to develop depression and low self-esteem. Since depression and self-esteem are negatively correlated to each other,[16] a psychiatric assessment and psychological support were sought. Due to the aforementioned complexities, her feminizing surgery has been postponed.
In a study of 70 CAH patients (both 46 XX and XY), 46 XX CAH patients scored higher on depression and anxiety scores accompanied with a poor quality of life as compared to controls.[17] Conversely, psychological distress, self-harming behavior, and suicidal tendencies were assessed by a group of researchers in different subgroups of DSD using standardized tests. Eleven 46 XX CAH patients, reared as females, were found to be less psychologically distressed with lower self-harming behavior than the rest of the subgroups. SW-CAH patients were more distressed than patients with simple virilizing CAH.[18] In our study, patient C.4 was SV-CAH, and patient C.16 was SW-CAH.
The psychoneuroendocrinological causative factors behind a typical and an atypical gender identity are still poorly understood. The exact roots of gender identity issues in patients with CAH are difficult to ascertain. It can perhaps be best understood as an interplay of prenatal androgenization, sex of rearing, and the sociocultural context.[19] For patient C.4, her tomboyish behavior at the age of 6 years, can be explained by the dominance of androgenizing hormones and interaction with her immediate peer circle.
Patient C.16, being 22 years old, also did not meet the criteria for GIDAA according to ICD-10.[15] Her gender confusion and psychological distress had more of societal and psychological underpinnings than the sole effect of hormones. On a social level, she liked playing cricket and staying out late at night, which is usually allowed in the case of boys. On a personal level, she envied the freedom and independence that boys her age are allowed. She disliked her feminine body along with undergoing the process of menstruation. She found it cumbersome, and it disrupted her daily activities. It also prevented her from pursuing cricket further. Her psychiatric consultation and counseling revealed high levels of anxiety and rumination regarding her future and financial independence. At present, she accompanies her father to work and is thinking of pursuing the same career line. The patient has undergone clitoroplasty as a child. She did not want any more surgery. Her feminizing genitoplasty has been deferred due to the aforementioned circumstances.
In a study done to ascertain the role of hormones to explain the masculine preferences and behavior of CAH patients, SW-CAH patients were compared with SV-CAH patients on their gender-interests and roles. Results suggested a stronger masculine orientation for the SW-CAH patients. This difference was attributed to the varying effects of prenatal androgenization. Hence, gender dysphoria and confusion cannot be solely attributed to psychosocial variables.[20,21,22]
Finding a suitable partner, sexual functioning and subfertility are some of the many sources that cause distress to the patients and their families.[21] Long-term exposure to negative conditions can compromise the coping mechanisms of these individuals that can take the form of mental illness and/or complete loss of self-confidence. Unacceptability, hostility, teasing, and discrimination from others can severely hamper an individual in academia, intimate relations, and occupation. As a result, it can sharply affect their overall quality of life. On the other hand involving the patient and family and ensuring support can go a long way in making them well-adjusted individuals.
Our study included 19 46 XX CAH patients reared as females who had clitoromegaly and/or AG. As girls with CAH grow, each age group has their particular concerns. There were five patients in the preschool age (C.1, 2, 3, 4 and 5). Their parents’ main concern was regarding their child's future. Mother of patient C.3 (aged 5 years) seeks ways to help her daughter from drawing unwanted attention by not having to use the school washroom by using disposable absorbent undergarments. Such alternatives are used by parents to avoid stigma and shame. In light of such problems, mother of patient C.3 is presently under treatment for depression and anxiety. Due to stigma and shame associated with AG, parents of patients C.3 and C.5 have decided to get their children operated for genitoplasty at another center despite being reassured that surgery at a later age proves to be more beneficial for the patient.[23]
There were 7 post pre-school patients in the prepubertal age group (C.6, 7, 8, 9, 10, 11 and 12). Due to being toilet-trained, they were not exposed to ridicule when attending school. They are being followed up for adequacy of medical treatment, height, growth, and counseling.
There were two patients in the pubertal age. The main concerns in this age were delayed menarche, delayed breast development, irregular periods, the proper dose of medication to ensure optimal growth and height, acne, and hirsutism. This was managed with optimizing therapy. Both the patients, C.13 and C.14, aged 14, were reared as females. They did not show signs of gender dysphoria and seemed well-adjusted apart from the abovementioned concerns. Since, rapport could not be established with patient C.13 during assessment as she had an extremely shy nature, PR-GIQ was administered on her elder sister to ascertain gender dysphoria that was not found.
There were five patients who were above 18 years of age (C.15, 16, 17, 18, and 19). Patient C.18, aged 29, mature and financially independent, approached us with the issue of bisexuality. As in the case of CAH patients, along with a tomboyish personality, it is not uncommon to find their sexual preferences to be less heterosexual.[24]
Being in a similar situation, patient C.19, aged 31, was concerned about her “masculine” way of conversing and walking as pointed out by her family members. She was advised by her family to learn to be more feminine otherwise it may pose a threat to finding a suitable marriage partner for her. At present, she is awaiting surgery before getting married.
Patient C.17, aged 28, educated and financially independent, is well-adjustment to her long-term intimate partner who is supportive despite knowing about her condition and they plan to settle down in the near future. Patient C.15, aged 21, did not show any signs of gender dissonance and/or psychological maladjustments.
Three patients C.20, C.21, and C.22, aged 8, 12, and 32, respectively, were reared as males. Patient C.20, at present 32 years old, was born with AG and had been reared as a male for the first 17 years of her life.
She was brought to medical attention by her parents at 17 years of age when she began her menstrual cycles. After investigations, the parents were counseled about the patient's sex being chromosomally female. However, the patient's father insisted on raising her as a boy, following which, a panhysterectomy was performed without the patient's involvement. Postsurgery, she was prescribed testosterone injections for the development of male secondary sexual characteristics. Due to her genital ambiguity and fear of being ridiculed, the patient had discontinued schooling. Therefore, in spite of belonging to a financially stable family, she remains uneducated.
Soon afterward, the patient realized her discomfort in being a male, but felt sexually attracted to them. She disliked using men's washroom or carry out male-associated tasks. She felt comfortable in being a woman, liked dressing up like a female, and felt a strong sense of purpose in doing female-associated activities such as stitching and embroidering clothes. She preferred travelling in ladies’ compartment in the metro. As a result, she decided to live her life as a female and thus, discontinued her testosterone injections. Her psychological assessment at that time revealed gender dysphoria as a male. Consequently, she had also strongly expressed her wish to become a female, following which, her gender reassignment was performed at the age of 30 years. She underwent feminizing genitoplasty despite little parental support. At present, she is satisfied with her new female gender identity and did not show gender dysphoria on the female version of GIDAA. However, due to unacceptability from the society and her father, in particular, she has been ostracized from attending familial and sociocultural events. Initially, she admitted feeling anxious and suffering from low self-esteem due to body image issues. However, with the passage of time and due to hormone replacement therapy with psychological support, she has become comfortable with herself. At present, she seeks a partner for marriage.
Patient C.21, aged 12 years (prepubertal), was brought by his family for masculinizing genital surgery. A psychiatry consultation with psychological assessment for the patient and family is being sought before acceptance could be given for the same as it involves panhysterectomy followed by lifelong testosterone replacement. The patient is also being counseled. Although, to rear a Phenotypically female CAH patient as a boy is an uncommon event according to the guidelines and standard, with the help of surgical procedures and hormone replacement, normal secondary sexual characteristics can be achieved.[7,8,25] A recent study [26] has shown increased psychiatric morbidity in CAH men. To further facilitate the process of psychological adjustment and a good quality of life, social support is required.[7]
Both C.21 and C.22, aged 12 and 8 years, respectively, are satisfied with their male gender identity and their families are supportive of this decision. They have been reared as boys since birth. These two prepubertal children are being followed up.
Fifth stage of “Ego Identity versus Role Confusion” in the psychosocial theory by Erik Erikson [27] elucidates the effects of dissonance in gender identity during the transition from childhood to adolescence. During this stage, a child begins to examine and understand the roles he/she will play as adults. They explore two crucial identities in depth – personal and occupational, and begin to form a personal identity based on the outcome of their experiences. Nevertheless, a failure to establish this sense of personal identity can lead to identity confusion and inadequacy. Thus, a failure to establish and conform to a socially-accepted gender identity can cause psychological maladjustment.
CONCLUSION
Out of the 19 patients reared as females, majority were well-adjusted and showed no gender dysphoria. Two patients revealed gender dysphoria as indicated by their marginally low scores on the gender dysphoria assessment. However, in view of current literature and the age groups of the patients, behavior of the 6-year-old patient can be best understood as being tomboyish and in the 22-year-old can be explained by the dominance of psychosocial factors and not hormones alone. Among the three patients reared as males, two prepubertal were satisfied with their male gender identity. However, since they are prepubertal, they are in follow-up, it remains to be seen how they progress in future. The third patient, aged 32, had gender dysphoria when reared as a male that resolved when feminizing surgery was done, and gender was reassigned as a female. Thus, gender assignment in 46 XX CAH and reassignment are guided by several factors that include the degree of virilization of genitalia, gender orientation, patient involvement, parental, and sociocultural influences.
Financial support and sponsorship
This work is funded by the Indian Council of Medical Research DHR/GIA/1/2014.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We acknowledge late Professor AC Ammini for her intellectual support.
REFERENCES
- 1.Berenbaum S. Psychological outcome in children with disorders of sex development: Implications for treatment and understanding typical development. Annu Rev Sex Res. 2006;17:1–38. [Google Scholar]
- 2.Cohen-Kettenis PT. Psychosocial and psychosexual aspects of disorders of sex development. Best Pract Res Clin Endocrinol Metab. 2010;24:325–34. doi: 10.1016/j.beem.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 3.Ercan O, Kutlug S, Uysal O, Alikasifoglu M, Inceoglu D. Gender identity and gender role in DSD patients raised as females: A preliminary outcome study. Front Endocrinol (Lausanne) 2013;4:86. doi: 10.3389/fendo.2013.00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Vries AL, Doreleijers TA, Cohen-Kettenis PT. Disorders of sex development and gender identity outcome in adolescence and adulthood: Understanding gender identity development and its clinical implications. Pediatr Endocrinol Rev. 2007;4:343–51. [PubMed] [Google Scholar]
- 5.Sandberg DE, Gardner M, Cohen-Kettenis PT. Psychological aspects of the treatment of patients with disorders of sex development. Semin Reprod Med. 2012;30:443–52. doi: 10.1055/s-0032-1324729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dessens AB, Slijper FM, Drop SL. Gender dysphoria and gender change in chromosomal females with congenital adrenal hyperplasia. Arch Sex Behav. 2005;34:389–97. doi: 10.1007/s10508-005-4338-5. [DOI] [PubMed] [Google Scholar]
- 7.Lee PA, Houk CP. Review of outcome information in 46 XX patients with congenital adrenal hyperplasia assigned/reared male: What does it say about gender assignment? Int J Pediatr Endocrinol. 2010;2010:982025. doi: 10.1155/2010/982025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma S, Gupta DK. Male genitoplasty for 46 XX congenital adrenal hyperplasia patients presenting late and reared as males. Indian J Endocrinol Metab. 2012;16:935–8. doi: 10.4103/2230-8210.102994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson LL, Bradley SJ, Birkenfeld-Adams AS, Kuksis MA, Maing DM, Mitchell JN, et al. A parent-report gender identity questionnaire for children. Arch Sex Behav. 2004;33:105–16. doi: 10.1023/b:aseb.0000014325.68094.f3. [DOI] [PubMed] [Google Scholar]
- 10.Singh D, Deogracias JJ, Johnson LL, Bradley SJ, Kibblewhite SJ, Owen-Anderson A, et al. The gender identity/gender dysphoria questionnaire for adolescents and adults: Further validity evidence. J Sex Res. 2010;47:49–58. doi: 10.1080/00224490902898728. [DOI] [PubMed] [Google Scholar]
- 11.Urban WH. The Draw-a-person Catalogue for Interpretative Analysis. Los Angeles: Western Psychological Services; 1963. [Google Scholar]
- 12.Bekhit NS, Thomas GV, Jolley RP. The use of drawing for psychological assessment in Britain: Survey findings. Psychol Psychother. 2005;78(Pt 2):205–17. doi: 10.1348/147608305X26044. [DOI] [PubMed] [Google Scholar]
- 13.Meyer-Bahlburg HF, Dolezal C, Baker SW, Carlson AD, Obeid JS, New MI. Prenatal androgenization affects gender-related behavior but not gender identity in 5-12-year-old girls with congenital adrenal hyperplasia. Arch Sex Behav. 2004;33:97–104. doi: 10.1023/b:aseb.0000014324.25718.51. [DOI] [PubMed] [Google Scholar]
- 14.Arteche A, Bandeira D, Hutz CS. Draw-a-person test: The sex of the first-drawn figure revisited. Arts Psychother. 2010;37:65–9. [Google Scholar]
- 15.World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization; 1992. [Google Scholar]
- 16.Sowislo JF, Orth U. Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychol Bull. 2013;139:213–40. doi: 10.1037/a0028931. [DOI] [PubMed] [Google Scholar]
- 17.Johannsen TH, Ripa CP, Mortensen EL, Main KM. Quality of life in 70 women with disorders of sex development. Eur J Endocrinol. 2006;155:877–85. doi: 10.1530/eje.1.02294. [DOI] [PubMed] [Google Scholar]
- 18.Schützmann K, Brinkmann L, Schacht M, Richter-Appelt H. Psychological distress, self-harming behavior, and suicidal tendencies in adults with disorders of sex development. Arch Sex Behav. 2009;38:16–33. doi: 10.1007/s10508-007-9241-9. [DOI] [PubMed] [Google Scholar]
- 19.Meyer-Bahlburg HF, Gruen RS, New MI, Bell JJ, Morishima A, Shimshi M, et al. Gender change from female to male in classical congenital adrenal hyperplasia. Horm Behav. 1996;30:319–32. doi: 10.1006/hbeh.1996.0039. [DOI] [PubMed] [Google Scholar]
- 20.Dittmann RW, Kappes MH, Kappes ME, Börger D, Meyer-Bahlburg HF, Stegner H, et al. Congenital adrenal hyperplasia. II: Gender-related behavior and attitudes in female salt-wasting and simple-virilizing patients. Psychoneuroendocrinology. 1990;15:421–34. doi: 10.1016/0306-4530(90)90066-i. [DOI] [PubMed] [Google Scholar]
- 21.Joseph AA, Shabir I, Marumadi E, Dada R, Ammini AC, Mehta M. Psychosexual outcomes in three siblings with partial androgen insensitivity syndrome: Impact of nature versus nurture. J Pediatr Endocrinol Metab. 2013;26:915–20. doi: 10.1515/jpem-2013-0154. [DOI] [PubMed] [Google Scholar]
- 22.Kukreti P, Kandpal M, Jiloha RC. Mistaken gender identity in non-classical congenital adrenal hyperplasia. Indian J Psychiatry. 2014;56:182–4. doi: 10.4103/0019-5545.130504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eckoldt-Wolke F. Timing of surgery for feminizing genitoplasty in patients suffering from congenital adrenal hyperplasia. Endocr Dev. 2014;27:203–9. doi: 10.1159/000363664. [DOI] [PubMed] [Google Scholar]
- 24.González R, Ludwikowski BM. Gender dysphoria in 46 XX persons with adrenogenital syndrome raised as females: An addendum. Front Pediatr. 2015;2:140. doi: 10.3389/fped.2014.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dasgupta R, Schnitzer JJ, Hendren WH, Donahoe PK. Congenital adrenal hyperplasia: Surgical considerations required to repair a 46 XX patient raised as a boy. J Pediatr Surg. 2003;38:1269–73. doi: 10.1016/s0022-3468(03)00287-2. [DOI] [PubMed] [Google Scholar]
- 26.Falhammar H, Frisén L, Norrby C, Hirschberg AL, Almqvist C, Nordenskjöld A, et al. Increased mortality in patients with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Endocrinol Metab. 2014;99:E2715–21. doi: 10.1210/jc.2014-2957. [DOI] [PubMed] [Google Scholar]
- 27.McLeod SA. Erik Erikson. 2013. [Last accessed on 2015 Dec 03]. Available from: http://www.simplypsychology.org/Erik-Erikson.html .


