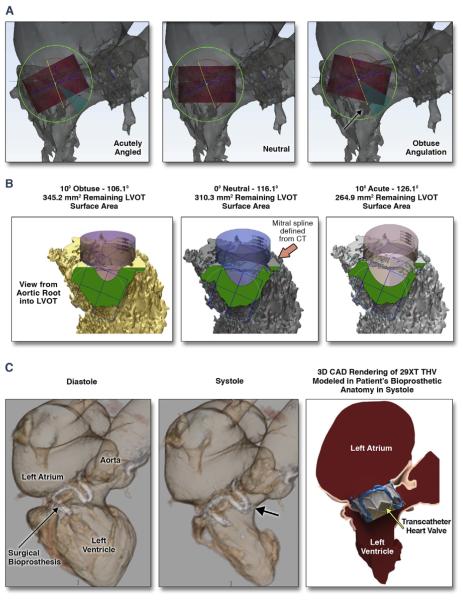
FIGURE 3. CT, Computer-Aided-Design, and 3D Print Analysis of the LVOT to Characterize and Quantify the Residual Post-TMVR “Neo-LVOT” Area Overcomes the Limitations of Traditional 2D Imaging Planes.
Preliminary data utilizing 2-dimensional (2D) echo imaging correlated acute angulation of the mitral aorta-outflow-angle (mAOA) with higher risk of LVOT obstruction compared with that of more obtuse mAOA. On the basis of our single-center experience, the association between mAOA and risk of LVOT obstruction was not reproducible (A and B). LVOT obstruction is not solely dependent on mAOA. Personalization and determination of feasibility of TMVR in patient-specific anatomy may not be accounted for if relying on 2D measurements of a 3D anatomy (A). CT and CAD 3DP analysis of the “neo-LVOT” surface area overcomes the limitations of traditional 2D imaging planes. THV implantation in the mitral position results in permanent anterior motion/displacement of the surgical/native anterior mitral leaflet. Both THV frame and permanent anterior motion/displacement can result in severe LVOT obstruction (C). The importance of understanding the application of this technology is the ability to test devices in patient-specific cardiac anatomy ex vivo for LVOT encroachment. Abbreviations as in Figure 1.