Abstract
Objective: To investigate the changes on self- and parental weight perceptions and parental communication with healthcare professionals (HCPs) in the United States during the mid-2000s period when the terminology changed for classifications of childhood obesity/overweight.
Methods: A repeated cross-sectional study was conducted with 6799 children aged 8–15 years with the National Health and Nutrition Examination Survey 2005–2014. BMI was calculated from objectively measured heights and weights, and children were classified as normal/underweight, overweight or obese, using the new terminology. Children reported their own weight status. Parents reported their child's weight status and reported how HCPs described their children's weight status. Logistic regressions were used to investigate changes in weight perceptions among overweight/obese children themselves and their parents and parental communication with HCPs about children's overweight/obesity status during the time of the terminology change.
Results: The proportion of parents told by HCPs about children's weight status increased for overweight children [6.8% in 2005–2006 to 18.8% in 2013–2014, p for trend (ptrend = 0.02)], and marginally increased between 2005–2006 (37.1%) and 2007–2008 (45.4%) for obese children (p = 0.09). However, parental perceptions for obese/overweight children did not change. Also, obese children's weight perception did not change, and the proportion of overweight children who perceived their weight status accurately declined in 2005–2012 (25.9%–16.4%, ptrend = 0.02).
Conclusions: Although the terminology change about childhood obesity/overweight was associated with increased communication about child's weight status by HCPs, the accuracy of weight perceptions among obese/overweight children or their parents did not improve or declined.
Keywords: : children, NHANES, obesity, overweight, perception, terminology change
Introduction
Childhood obesity poses a major public health concern globally. In the United States, approximately one-third of children aged 2–19 years are overweight or obese,1,2 and the prevalence of childhood obesity has more than quadrupled in school-age children and adolescents since 1971.3 Childhood obesity affects children's immediate and long-term well-being.4 With respect to immediate health effects, obese children are more likely to experience depression and psychosocial difficulties.5 With regard to long-term effects, obese children are at greater risk for developing life-threatening chronic conditions, such as diabetes,6 cardiovascular disease,7 and all-cause mortality.8,9
In 2005, the Institute of Medicine (IOM) published a report to address the epidemic of childhood obesity among healthcare professionals (HCPs). At that time, new terminology was introduced; “obesity” replaced “overweight” for children with BMI ≥95th percentile for age and sex or >30 kg/m2, and “overweight” replaced “at risk of overweight” for youth with BMI 85th to <95th percentiles for age and sex.10 This new terminology was implemented to effectively reinforce the importance of taking immediate action and the seriousness of obesity-related medical consequences. BMI in children reasonably correlates with direct measures of body fatness and much comorbidity, such as high blood pressure, insulin resistance, and increased lipid levels.10 In 2007, the Expert Committee published the evidence-based guidelines in all areas of obesity care in 2007 to be utilized by HCPs.11 The Expert Committee recommended that one of the best approaches for the HCP is to conduct routine assessments of all children at risk for obesity by plotting a BMI percentile on growth curve, and to have discussions with families regarding their children's weight statuses.11,12
Yet, the evidence suggests that the implementation of such clinical assessment on overweight and obesity children is not completed consistently.12,13 Healthcare systems often inhibit the HCPs from addressing overweight and obesity appropriately during clinical visits.13–15 Some of the obstacles to addressing childhood obesity in clinical settings include lack of reimbursement for lifestyle counseling,12–14 lack of time,13,14 lack of patient motivation,13 and fear of offending parents when identifying excess weight.13 In the past, the absence of a HCP comment on a child's weight status with a family has been identified as one of the strongest predictors of parental misclassification of their child's weight.12,16 Thus, it is important that HCPs make it a priority to assess weight in all children during the clinical visits and to communicate the results to parents in an easily understood and sensitive manner.12
Parental perceptions of their children's weight play an important role in obesity prevention and treatment; they have been shown to influence a child's eating habits, daily exercise pattern, and body weight perception.12,17–20 Parents' perception of their child's weight status can influence their decision to have their child participate in a pediatric weight control program.21 Children typically look at their parents as role models, food providers, and for guidance on healthy lifestyle development, all of which influence their risk of childhood obesity.20 Obesity treatments that include families are considered as one of the most successful interventions for childhood obesity.19,22 Programs that encourage parents to accept responsibility for implementing changes in their child's eating and exercise habits allow parents to positively influence their children's weight control efforts.19,23,24
However, while parental support on healthy behavior can positively influence children's weight status, there is a dissonance between parental perceptions and the actual weight status of their children.25–27 Research involving 355 child–parent pairs in Canada found that 38% of parents were not able to correctly classify their child's weight status.26 Similarly, The meta-analysis of 69 articles found that 50.7% of the parents with overweight or obese children underestimated the weight of their children.12 Furthermore, evidence suggests that parents with overweight or obese children are more likely to misperceive their child's weight status,27 and that children whose parents misperceived their weight were less likely to consume healthy diets compared with children with parents correctly perceiving their children's weight status.25
To prevent and treat childhood obesity, it is probably important for parents to have accurate perceptions of their children's weight statuses. In this study, we examined the trends in children's weight perceptions among children themselves, parents, and HCPs in the United States using the National Health and Nutrition Examination Survey (NHANES) data from 2005 to 2014.
Our conceptual hypotheses are as follows: the terminology change for classifying childhood obesity status would (1) widely increase urgency and seriousness among HCPs to actively address weight issues involving children, thus increasing accurate communication with parents about their children's weight status in the clinical setting; (2) improve the accuracy of parental perception of their children's weight status; and (3) increase the accuracy of self-perceived weight status among obese and overweight children.
Methods
Data Sources and Study Population
We conducted a repeated cross-sectional study analyzing the NHANES data collected from 2005 to 2014. The NHANES uses a nationally representative and multistage probability sample of the civilian, noninstitutionalized US population. Interview data were collected in the homes of study participants; anthropometric data were collected in mobile examination centers (MECs). More details about the NHANES study design and protocol are available on the NHANES website.28
This study included data from participants aged 8–15 years (n = 8011). We excluded those who did not participate in MEC examinations (n = 275) or whose height and/or weight information was missing (n = 54). In addition, we excluded participants if children themselves, their parents, or HCPs had missing information about perceptions of children's weight status (n = 432). We further excluded participants without information on family income level, the number of healthcare provider visits, or insurance coverage (n = 451), leading to a total sample of 6799 in our analyses. Due to the young age of our target study sample (8–15 years old), children's demographic information was provided by a proxy (mostly a parent); however, children provided their own weight perception. Among children aged 6–15 years from the 2005 to 2014 survey, the unweighted response rate of the household interview was 83.6% and that of the MEC examination was 80.6%29; the reported response rate age range of 6–15 years was the closest age range to that of our samples (8–15 years), among those whose response rates were obtainable from the response rate tables on the website.
Written informed consent was obtained from all participants or their parents. The NHANES protocol was approved by the National Center for Health Statistics (NCHS) Research Ethics Review Board.
Perception about Weight Status from Children, Parents, and HCPs
During the MEC examination, using the Computer-Assisted Personal Interviewing (CAPI) system, trained interviewers asked children about self-perception of weight status (“Do you consider yourself now to be fat or overweight, too thin, or about the right weight?”).30 In addition to the question directed to the children themselves, their parents were asked about their perception of their children's weight status (“Do you consider (the child) now to be overweight, underweight, or about the right weight?”).31 For these questions, we dichotomized the responses into “overweight” and “not overweight.” In addition, the parents were asked whether the HCPs had communicated information regarding their children's weight status (“Has a doctor or health professional ever told you that “CHILD'S NAME” was overweight?”).31 The responses to this question were dichotomized, indicating whether the healthcare provider communicated information to the parents about their children's overweight status.
Body Index and Main Definitions of Obesity and Overweight
Information about the child's age and sex was obtained during the home interviews. The child's height and weight were measured during the MEC examination. We calculated BMI percentile for age and sex using the CDC sex-specific 2000 BMI-for-age growth charts for the United States.32 According to the Expert Committee Recommendations in 2007,11 we categorized BMI percentile into three categories: normal weight or underweight (BMI <85th percentile), overweight (BMI 85th to <95th percentile), and obese (BMI ≥95th percentile or ≥30 in kg/m2).
Potential Confounders
We extracted data on potential confounders, including age, sex, race and ethnicity, family income, the number of healthcare provider visits, and insurance coverage. Race/ethnicity was classified into non-Hispanic white, non-Hispanic black, Mexican American, and others, including other Hispanics and multiracial participants. Among several income variables in the NHANES questionnaires, we used a ratio of family income to the poverty line [income-to-poverty ratio (IPR)], categorized into four categories: 4 of IPR or greater, 2 to <4 of IPR, 1 to <2 of IPR, and <1 of IPR. We grouped the number of healthcare provider visits over the past year into four categories: none, once, twice or three times, and four times or more. We also prepared a dichotomous variable about insurance coverage (covered or not covered by insurance).
Statistical Analyses
All statistical analyses were conducted using the survey suite of Stata (Version 12.1; StataCorp, College Station, TX) statistical procedures, which included survey weights that accounted for the complex survey design. Because all participants in this study were those who came to the MEC interviews, we used the sample weight specific to MEC participants. To conduct trend analyses, we combined five cycles of NHANES data: from 2005–2006 to 2013–2014.
Proportion of each weight category (“obesity,” “overweight,” and “normal weight or underweight”) was classified by BMI percentile for age and sex, and was calculated for each survey cycle, using the 2007 Expert Committee's obesity/overweight definition.11 Descriptive statistics on children's and families' characteristics were calculated separately for each weight category as well as survey cycle. Linear trends over time were assessed based on chi-squared tests for categorical variables and linear regressions for continuous variables. We also compared the characteristics between the weight categories across the survey cycle.
Next, we developed regression models to examine temporal time trends of children's weight perceptions among children, parents, and HCPs by an objectively measured weight category.33 We used logistic regression models to account for the dichotomous outcome variables (whether children and parents perceived the children to be overweight and whether HCPs communicated the children's overweight status with their parents). To account for nonlinear time trends by children's weight categories, we included interaction terms between survey cycle (categorical) and children's weight category (categorical). We also included dichotomous age category (8–11 years/12–15 years), sex, race/ethnicity, family income category, healthcare provider visit category, and insurance coverage as covariates. We then applied these models to calculate model-adjusted estimates of proportions of children, parents, and HCPs who perceived the children to be overweight (compared with not overweight) for each combination of objectively measured weight status and survey cycle. That is, we calculated hypothetical proportions assuming that all participants had been in one survey cycle category (e.g., 2005–2006), had traits of one actual weight category (e.g., obesity), and had the other characteristics (e.g., race/ethnicity) as they actually were.
To perform trend tests, we included the continuous survey cycle variable in the multiple logistic regression models instead of the categorical survey cycle variable, and we examined whether the coefficient of the survey cycle variable was significantly different from zero.
Following the examination of the overall trend of the perception for each survey cycle, post hoc analyses were conducted to examine the visually observed differences of the proportions between two time periods.
To investigate the trends about associations between obese/overweight child's perception and parental perception of the child's overweight status, we developed another model about child's perception predicted by the interaction term between parental perception and survey period and other covariates, including objectively measured BMI category (obesity or overweight), age category, sex, race/ethnicity, family income category, healthcare provider visits over past year, and insurance coverage, restricting analyses to obese/overweight children as determined by measured BMI. We then used the model to visualize the model-adjusted probability of children perceiving themselves as overweight by whether their parents considered the children to be overweight and by survey period. We also developed a model to investigate the association between parental perception about child's overweight status and the HCP perception, but only for cases where the children had been objectively classified as obese or overweight.
All analyses in this study used the significance level of 0.05.
Results
The proportions of obese or overweight children defined by the Expert Committee definition did not change significantly from 2005 to 2014 (Table 1). Mean age, the proportion of age in 12–15, and gender distribution did not differ by weight category. Non-Hispanic black and Mexican American participants were more likely to be overweight or obese than non-Hispanic white and other participants (other Hispanics and multiracials) (p < 0.001). The participants with lower family income were more likely to be overweight or obese than those with higher income (p < 0.001).
Table 1.
Characteristics of Study Samples by Weight Category and Survey Cycle, 2005–2014
| 2005–2006 | 2007–2008 | 2009–2010 | 2011–2012 | 2013–2014 | Total | p for trenda | p for comparison by weight categoryb | |
|---|---|---|---|---|---|---|---|---|
| Obesityc | ||||||||
| Unweighted sample, N | 368 | 290 | 250 | 284 | 289 | 1481 | ||
| Weighted proportion, % | 17.1 | 20.4 | 17.2 | 20.6 | 19.9 | 19.0 | ||
| Age, mean (SD), years | 11.6 (2.5) | 11.4 (2.2) | 11.4 (2.3) | 11.7 (1.9) | 11.7 (2.2) | 11.6 (2.2) | 0.32 | 1.00 |
| Age in 12–15, % | 52.5 | 47.7 | 45.9 | 57.0 | 51.6 | 51.2 | 0.32 | 0.81 |
| Female sex, % | 50.5 | 47.2 | 43.3 | 52.9 | 48.9 | 48.8 | 0.41 | 0.38 |
| Race and ethnicity,d % | ||||||||
| Non-Hispanic white | 46.3 | 53.7 | 48.9 | 48.8 | 46.3 | 48.9 | 0.79 | <0.001 |
| Non-Hispanic black | 21.0 | 16.2 | 20.1 | 16.6 | 14.8 | 17.5 | 0.31 | |
| Mexican American | 20.8 | 17.0 | 18.1 | 19.3 | 20.6 | 19.2 | 0.87 | |
| Otherse | 11.8 | 13.1 | 12.9 | 15.3 | 18.3 | 14.4 | 0.19 | |
| Family income category,d % | ||||||||
| 4 of IPR or greater | 14.8 | 20.0 | 24.5 | 13.9 | 16.4 | 17.7 | 0.70 | <0.001 |
| 2 to <4 of IPR | 30.7 | 25.4 | 20.2 | 24.6 | 31.9 | 26.7 | 0.87 | |
| 1 to <2 of IPR | 26.0 | 28.4 | 24.8 | 30.1 | 24.7 | 26.9 | 0.94 | |
| <1 of IPR | 28.4 | 26.1 | 30.4 | 31.3 | 27.0 | 28.7 | 0.85 | |
| Healthcare provider visits over past year,d % | ||||||||
| None | 14.1 | 13.9 | 11.9 | 10.4 | 8.9 | 11.7 | 0.05 | 0.14 |
| Once | 30.4 | 23.8 | 23.5 | 26.6 | 27.6 | 26.4 | 0.86 | |
| Twice or three times | 34.9 | 36.1 | 39.5 | 34.1 | 33.1 | 35.4 | 0.58 | |
| Four times or more | 20.6 | 26.1 | 25.1 | 29.0 | 30.4 | 26.5 | 0.10 | |
| No insurance, % | 17.9 | 10.7 | 7.4 | 9.9 | 5.5 | 10.2 | 0.01 | 0.07 |
| Overweightc | ||||||||
| Unweighted sample, N | 252 | 217 | 210 | 205 | 242 | 1126 | ||
| Weighted proportion, % | 15.8 | 17.4 | 16.3 | 16.2 | 16.0 | 16.4 | ||
| Age, mean (SD), years | 11.6 (2.2) | 11.7 (2.1) | 11.5 (2.0) | 11.3 (2.1) | 11.7 (2.1) | 11.6 (2.1) | 0.71 | — |
| Age in 12–15, % | 52.9 | 49.7 | 50.1 | 44.5 | 52.3 | 49.8 | 0.70 | |
| Female sex, % | 50.1 | 55.2 | 53.6 | 49.0 | 50.5 | 51.7 | 0.63 | — |
| Race and ethnicity,d % | ||||||||
| Non-Hispanic white | 63.4 | 59.6 | 56.2 | 55.3 | 46.2 | 56.2 | 0.06 | — |
| Non-Hispanic black | 12.4 | 13.7 | 13.5 | 13.9 | 16.3 | 13.9 | 0.40 | |
| Mexican American | 13.5 | 14.9 | 16.6 | 16.4 | 20.6 | 16.4 | 0.19 | |
| Otherse | 10.7 | 11.7 | 13.8 | 14.4 | 16.9 | 13.5 | 0.10 | |
| Family income category,d % | ||||||||
| 4 of IPR or greater | 27.0 | 23.3 | 23.1 | 26.2 | 19.3 | 23.8 | 0.41 | — |
| 2 to <4 of IPR | 35.6 | 32.0 | 31.5 | 25.1 | 22.7 | 29.4 | 0.03 | |
| 1 to <2 of IPR | 18.3 | 20.4 | 24.2 | 23.6 | 25.6 | 22.4 | 0.06 | |
| <1 of IPR | 19.1 | 24.4 | 21.2 | 25.1 | 32.4 | 24.4 | 0.08 | |
| Healthcare provider visits over past year,d % | ||||||||
| None | 15.5 | 13.5 | 10.2 | 9.9 | 14.0 | 12.6 | 0.30 | — |
| Once | 25.9 | 28.2 | 26.5 | 25.6 | 21.8 | 25.6 | 0.32 | |
| Twice or three times | 41.1 | 30.1 | 34.6 | 34.6 | 41.6 | 36.3 | 0.64 | |
| Four times or more | 17.5 | 28.2 | 28.6 | 29.9 | 22.7 | 25.4 | 0.20 | |
| No insurance, % | 10.8 | 13.1 | 11.8 | 6.7 | 10.9 | 10.6 | 0.45 | — |
| Normal weight or underweightc | ||||||||
| Unweighted sample, N | 1018 | 725 | 794 | 807 | 848 | 4192 | ||
| Weighted proportion, % | 67.1 | 62.2 | 66.6 | 63.2 | 64.1 | 64.6 | ||
| Age, mean (SD), years | 11.6 (2.3) | 11.6 (2.0) | 11.6 (2.0) | 11.6 (2.0) | 11.5 (2.0) | 11.6 (2.1) | 0.65 | — |
| Age in 12–15, % | 50.3 | 50.8 | 51.9 | 53.2 | 50.1 | 51.3 | 0.82 | |
| Female sex, % | 48.2 | 46.1 | 50.0 | 51.8 | 48.9 | 49.0 | 0.36 | — |
| Race and ethnicity,d % | ||||||||
| Non-Hispanic white | 63.1 | 61.6 | 63.1 | 59.7 | 58.1 | 61.1 | 0.37 | — |
| Non-Hispanic black | 13.5 | 12.6 | 11.3 | 13.0 | 13.3 | 12.7 | 1.00 | |
| Mexican American | 10.4 | 11.5 | 12.2 | 12.1 | 12.8 | 11.8 | 0.44 | |
| Otherse | 13.0 | 14.3 | 13.3 | 15.2 | 15.7 | 14.3 | 0.27 | |
| Family income category,d % | ||||||||
| 4 of IPR or greater | 31.5 | 29.9 | 29.7 | 28.9 | 27.8 | 29.6 | 0.51 | — |
| 2 to <4 of IPR | 34.5 | 26.1 | 27.9 | 28.9 | 29.1 | 29.4 | 0.25 | |
| 1 to <2 of IPR | 18.2 | 22.1 | 23.7 | 21.4 | 20.7 | 21.2 | 0.53 | |
| <1 of IPR | 15.8 | 21.9 | 18.7 | 20.7 | 22.4 | 19.8 | 0.15 | |
| Healthcare provider visits over past year,d % | ||||||||
| None | 14.2 | 13.3 | 12.0 | 11.8 | 10.6 | 12.4 | 0.10 | — |
| Once | 26.5 | 32.1 | 26.2 | 33.1 | 30.9 | 29.7 | 0.11 | |
| Twice or three times | 31.5 | 29.2 | 33.3 | 33.7 | 34.5 | 32.5 | 0.11 | |
| Four times or more | 27.8 | 25.4 | 28.6 | 21.4 | 24.0 | 25.4 | 0.03 | |
| No insurance, % | 9.1 | 9.5 | 8.3 | 9.5 | 5.3 | 8.4 | 0.12 | — |
Trends over time were assessed using chi-squared tests for linear trends for categorical variables and linear regressions for continuous variables.
Comparisons among weight categories were made using pooled samples across the study period.
Weight status was categorized using the definition by the Expert Committee in the United States; obesity (BMI ≥95th percentile for age and sex or ≥30 kg/m2), overweight (BMI 85th to <95th percentile), and normal weight or underweight (BMI <85th percentile).
Percentages do not sum to 100% due to rounding.
The category includes other Hispanics and other races, including multiracial participants.
IPR, income-to-poverty ratio.
Supplementary Tables S1–S3 (Supplementary Data are available online at www.liebertpub.com/chi) illustrate the relationships between the perceptions about children's weight status from children themselves, their parents, and HCPs (reported by the parents), while adjusting for covariates. For children, age of 12–15 and female sex were associated with higher probability of perceiving children themselves as overweight, while non-Hispanic black race/ethnicity (compared with non-Hispanic white) was associated with lower probability. For parents, female sex, Mexican American, and other races/ethnicities (compared with non-Hispanic white) were associated with higher probability of perceiving their children as overweight. Age of 12–15, non-Hispanic black, Mexican American, other races/ethnicities (compared with non-Hispanic white), and larger number of HCP visits were associated with higher probability of parent's report of having ever told that their children were overweight, and no insurance coverage was associated with lower probability.
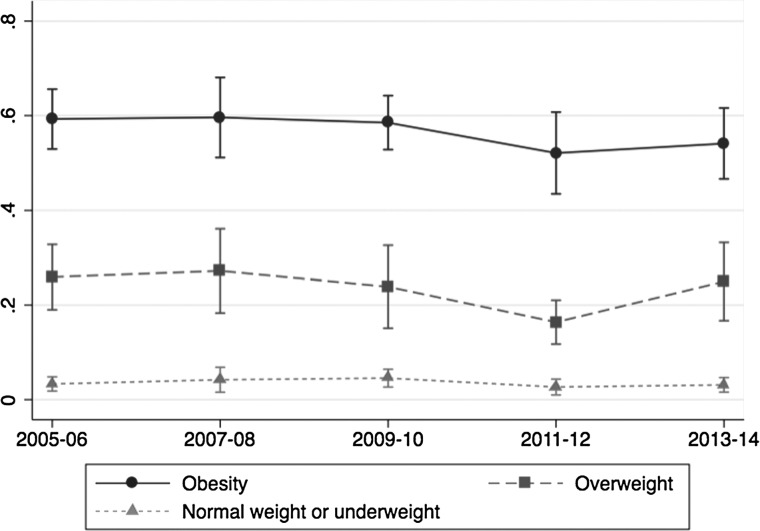
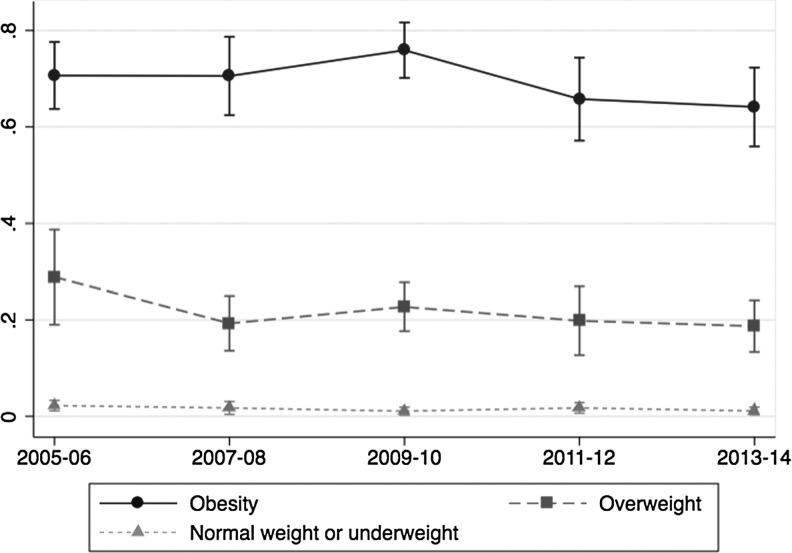
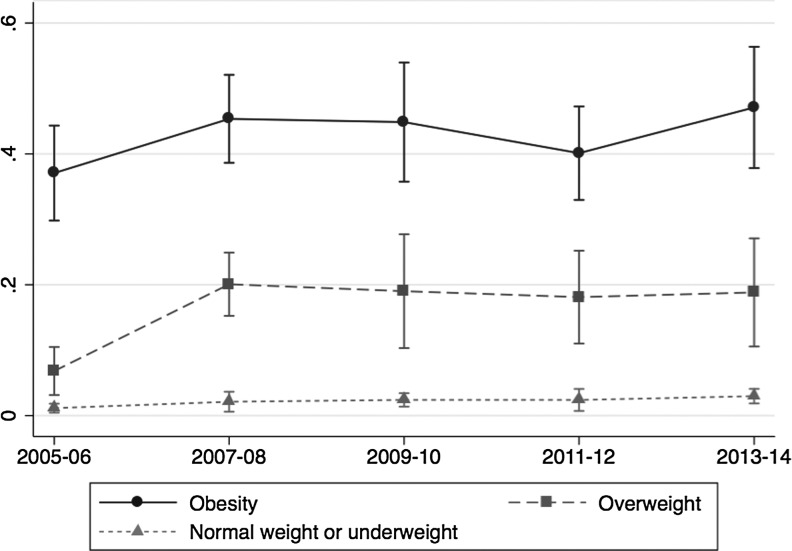
Figures 1–3 and Table 2 summarize the trends of weight status perceptions among children (Fig. 1), parents (Fig. 2), and communication by HCPs (Fig. 3) over time, using the aforementioned regression models. The proportion of obese children with correct weight perception did not change significantly over the study period (ptrend = 0.11). The proportion of overweight children with correct weight perception also did not change significantly from 2005 to 2014 (ptrend = 0.30), although there appears a decreasing trend from 2005–2006 toward 2011–2012, followed by a regain toward 2013–2014; a post hoc comparison of predicted proportions showed that the decrease from 25.9% in 2005–2006 toward 16.4% in 2011–2012 was statistically significant (p = 0.02), whereas the upward trend between 16.4% in 2011–2012 and 25.0% in 2013–2014 was marginally significant (p = 0.07).
Figure 1.
Trends of proportions of children aged 8–15 years who perceived themselves to be overweight, by children's weight category (normal weight or underweight, overweight and obesity) (%). Adjusted for age category, sex, race and ethnicity, family income category, healthcare provider visits over past year, and insurance coverage. The obesity/overweight definition by the Expert Committee was used to categorize weight status. Error bars represent 95% confidence intervals.
Figure 2.
Trends of proportions of children aged 8–15 years who were considered to be overweight by their parents, by children's weight category (normal weight or underweight, overweight and obesity) (%). Adjusted for age category, sex, race and ethnicity, family income category, healthcare provider visits over past year, and insurance coverage. The obesity/overweight definition by the Expert Committee was used to categorize weight status. Error bars represent 95% confidence intervals.
Figure 3.
Trends of proportions of parents (of children aged 8–15 years) who reported being informed of children's overweight status by healthcare professionals, by children's weight category (normal weight or underweight, overweight and obesity) (%). Adjusted for age category, sex, race and ethnicity, family income category, healthcare provider visits over past year, and insurance coverage. The obesity/overweight definition by the Expert Committee was used to categorize weight status. Error bars represent 95% confidence intervals.
Table 2.
Proportions of Children's and Parents' Perceptions and Parental Communication with Healthcare Professionals about Children's Overweight Status, Stratified by Children's Actual Weight Status
| 2005–2006 | 2007–2008 | 2009–2010 | 2011–2012 | 2013–2014 | p for trenda | |
|---|---|---|---|---|---|---|
| Obesity, BMI ≥95th percentileb | ||||||
| Proportion for obese children,c weighted % (unweighted n) | 17.1 (368) | 20.4 (290) | 17.2 (250) | 20.6 (284) | 19.9 (289) | — |
| Children's perception,d weighted % (unweighted n) | 59.3 (210) | 59.6 (174) | 58.5 (143) | 52.0 (149) | 54.1 (146) | 0.11 |
| Parents' perception,e weighted % (unweighted n) | 70.7 (260) | 70.5 (202) | 75.9 (187) | 65.8 (196) | 64.1 (198) | 0.13 |
| Communication with healthcare professionals,f weighted % (unweighted n) | 37.1 (152) | 45.4 (147) | 44.9 (122) | 40.1 (130) | 47.1 (146) | 0.21 |
| Overweight, BMI ≥85th or <95th percentileb | ||||||
| Proportion for overweight children,c weighted % (unweighted n) | 15.9 (252) | 17.4 (217) | 16.3 (210) | 16.2 (205) | 16.0 (242) | — |
| Children's perception,d weighted % (unweighted n) | 25.9 (71) | 27.2 (57) | 23.9 (52) | 16.4 (41) | 25.0 (56) | 0.30 |
| Parents' perception,e weighted % (unweighted n) | 28.9 (72) | 19.3 (49) | 22.7 (49) | 19.8 (44) | 18.7 (49) | 0.13 |
| Communication with healthcare professionals,f weighted % (unweighted n) | 6.8 (23) | 20.1 (40) | 19.0 (37) | 18.1 (33) | 18.8 (41) | 0.02 |
| Normal weight or underweight, BMI <85th percentileb | ||||||
| Proportion for normal or underweight children,c weighted % (unweighted n) | 67.1 (1018) | 62.2 (725) | 66.6 (794) | 63.2 (807) | 64.1 (848) | — |
| Children's perception,d weighted % (unweighted n) | 3.3 (28) | 4.2 (29) | 4.6 (34) | 2.7 (26) | 3.1 (30) | 0.47 |
| Parents' perception,e weighted % (unweighted n) | 2.2 (17) | 1.7 (14) | 1.1 (10) | 1.8 (13) | 1.1 (13) | 0.41 |
| Communication with healthcare professionals,f weighted % (unweighted n) | 1.1 (21) | 2.1 (17) | 2.4 (20) | 2.4 (19) | 3.0 (27) | 0.03 |
The p-values for trend were calculated from multivariable logistic regression models for dichotomous outcome variables (whether children and parents perceived the children to be overweight and whether health professionals communicated the children's overweight status with their parents), including objectively observed weight category (categorical), survey cycle (continuous), and their interaction terms as independent variables.
Weight status was categorized using the definition by the Expert Committee in the United States.
The proportions shown here are slightly different from those shown in Table 1 due to the missing data in the multiple logistic regression analyses.
The number of children who perceive their weight status correctly divided by the total number of children who are in each weight category (obese/overweight/normal or underweight).
The number of children whose parents correctly perceive children's weight status divided by the total number of children who are in each weight category (obese/overweight/normal or underweight).
The number of children whose parents answered that healthcare professionals communicated their children's overweight status divided by the total number of children who are in each weight category (obese/overweight/normal or underweight).
The proportion of parents with overweight/obese children who correctly perceived their children's weight status did not change significantly; the predicted proportions shifted from 70.7% in 2005–2006 to 64.1% in 2013–2014 among parents of obese children (ptrend = 0.13) and from 28.9% in 2005–2006 to 18.7% in 2013–2014 among parents of overweight children (ptrend = 0.13).
In contrast to the decreasing or static trends among children or their parents, the proportion of HCPs who communicated with the parents about their obese or overweight children's weight status showed upward trends. Especially, the proportion of HCPs who communicated with the parents about overweight children's weight status significantly increased from 6.8% in 2005–2006 toward 18.8% in 2013–2014 (ptrend = 0.02). A post hoc analysis showed that the increase between 2005–2006 (6.8%) and 2007–2008 (20.1%) was significant (p < 0.001). Although the overall trend was not significant as for that about obese children's weight status (ptrend = 0.21), a post hoc analysis showed that the increase between 2005–2006 (37.1%) and 2007–2008 (45.4%) was marginally significant (p = 0.09).
Children with normal weight or underweight rarely perceived themselves as overweight, and few parents considered their children to be overweight (all proportions <5% over the study period). Surprisingly, we found a significant increase in the proportion of parents of normal/underweight children reporting that HCPs had ever reported their child to be overweight from 1.1% in 2005–2006 to 3.0% in 2013–2014 (ptrend = 0.03).
The proportion of obese/overweight children who correctly perceived themselves to be overweight was higher when their parents perceived them to be overweight, compared with when their parents did not perceive them to be overweight, throughout the survey period (Supplementary Fig S1). The trend tests showed that the proportions did not increase or decrease significantly over time. Similarly, the proportion of obese/overweight children's parents who correctly perceived their children as overweight was consistently higher when HCPs informed them that their child was overweight, compared with when HCPs did not inform them that their child was overweight (Supplementary Fig S2). Among parents who had not been informed about their children's overweight status from HCPs, the proportion of parents perceiving their children to be overweight decreased from 45.9% in 2005–2006 to 27.9% in 2013–2014 (ptrend < 0.001). However, the proportion did not change among parents who had been informed of children's overweight status from HCPs (ptrend = 0.54).
Discussion
To our knowledge, this is the first study to examine the temporal trends of perceptions on children's weight status among children, parents, and HCPs concurrently, during a period that included the time when the Expert Committee changed the terminology for describing pediatric weight status. The observed trends in the proportion of weight perceptions raise interesting interpretations. The results indicate that IOM terminology change in 2005 and the 2007 Expert Committee's recommendations on childhood obesity had a positive effect on increasing HCP communication with parents about their children's weight status; however, it did not lead to the overall increases in proportions of accurate weight perceptions among children or parents. Ironically, the proportions of overweight children with accurate weight perception actually decreased from 2005–2006 to 2011–2012.
As shown in Table 2, 37.1%–47.1% of parents with obese children recalled being told by HCPs about their children's weight status. For overweight children, 6.8%–20.1% of parents reported such information over time. Although these proportions were lower than those of children and parents, the trends showed nonsignificant increase for obese children and significant increase for overweight children, which could be the result of the terminology change.
Additional analyses were conducted to investigate the potential associations between the perceptions of child weight status in HCPs, parents, and children. There was a significant decrease in accurate parental perceptions among those who did not communicate with HCPs about their children's overweight status (from 45.9% to 27.9%). The proposed hypotheses should not be rejected inasmuch as a significant portion of parents, who did receive information from HCPs about their children's weight status, reported accurate weight perceptions. The issue appears to be that parents are becoming less likely to be aware about their children's overweight status in the absence of correcting information from the HCPs, which undermined the intended effect of the terminology change overall by decreasing the proportion of parents with accurate perceptions of their children's weight status. This may be one of the reasons why the perceptions among children and their parents did not become more congruent over time.
Our analysis therefore confirms that interventions to facilitate the communication between HCPs and parents about their children's weight status are effective in increasing the accurate perception of overweight status among obese/overweight children and their parents.12 When parents are given a simple report outlining their child's BMI or weight classification, and general guidelines regarding diet and physical activity are provided, they become much more accurate in assessing their child's weight status.34 HCPs are in an ideal position to take steps to remedy the self- and parental misperceptions concerning children's weight status.12 When parental perceptions of their child's weight status are corrected, they are more likely to move forward to making the lifestyle changes.12,24 Therefore, HCPs need to prioritize assessing weight in all children at clinical visits and communicate the results to parents in an understandable and sensitive manner.12
We conclude that the pediatric weight status terminology change generated positive effects to raise awareness of childhood obesity epidemic among HCPs, which resulted in a small increase in the proportion of HCPs reporting children's weight status to their parents over the study period. The communication by a HCP about a child's weight status itself is an effective strategy to correct parental perception as evidenced by an increase in the odds of correct weight perceptions among parents with overweight/obese children whose weight status had been discussed by the HCP. However, over the same study period, there was a significant decrease in accurate parental perceptions among those parents receiving no such HCP communication. Such shift in parent perceptions may be due to a generational change in parental weight perception over time. Given that there are multiple barriers identified in the clinical settings, several strategies could have been integrated to supplement the impact of the terminology change. Such strategies include implementation of clinical information systems to allow a timely reminder for a routine screening, electronic medical records integration to ease BMI assessments, and appropriate reimbursement for obesity prevention visits.35
Several studies in the past have assessed the shifts of child's weight status focusing on each standpoint using the NHANES data. For example, Lu et al. investigated the shift of self-perceived body weight among adolescents from 1988–1994 to 2007–2012.36 Their results indicated that the probability of overweight or obese adolescents (aged 12–16 years) who perceived themselves to be overweight had declined over the time period.30 Their study treated 2007–2012 as one time block to compare with 1988–1994, rather than examining a more precise biennial trend. Similar analyses were performed for parents' perception about school-aged children (aged 6–11 years) by Hansen et al.37 and preschool children (aged 2–5 years) by Duncan et al.,38 concluding that there was a potential generational shift involving parental body weight perception about their children over the last few decades. In addition, several studies39–41 found that HCP notification about a child's unhealthy weight has increased significantly over time, based on NHANES data obtained between 1999 and 2014. Yet, the likelihood of being notified about a child's weight status by a HCP remained small. Hansen et al. reported that only 30% of overweight or obese children were notified about their obesity status by their HCP.39 A further complication from recent literature is evidence that adolescent misperception of weight status might protect them from future weight gain or from unhealthy weight-related behaviors and depression.42,43
Our study had several limitations. First, the repeated cross-sectional study design was observation and therefore did not permit assessment of causal direction as might have been possible with longitudinal data. Yet, the assessment on transitions of perceptions and connections between the perceptions from different perspectives at the population level during the time of the terminology change consists of interesting findings with important implications. Second, as described above, communication by HCPs about children's weight status was not a direct measurement. Instead, the measurement was obtained from the parents; thus, this may pose a recall bias. Third, because the terminology change on childhood overweight/obesity was first proposed by IOM in 2005,10 followed by the Expert Committee's recommendation in 2007,11 the exact time when HCPs actually experienced the terminology change is imprecise. Thus, it is possible that the perceptions observed in the survey cycle of 2005–2006 had already changed in response to the change in terminology. Finally, the US Preventive Services Task Force revised its recommendation on childhood obesity in 2010,44 which may have confounded our observations.
In conclusion, with nationally representative US data, we observed increases in communication by HCPs about children's weight status over the study period. Such results indicate that there was an impact on rising urgency and seriousness to address childhood obesity among HCPs, In fact, the largest increases in HCPs communicating children's weight status were observed between 2005–2006 and 2007–2008. However, such increases did not lead to the proportional increases in the accuracy of children's or parental perceptions of the children's weight status. Additional research is needed to understand better the barriers to accurate perception of children's weight status and to anticipate the likely costs and benefits of promoting HCP communication about the obese/overweight status of children in clinical settings.
Supplementary Material
Acknowledgments
T.S. was supported by the grant of National Center for Global Health and Medicine; W.J.M. was supported by grant 1P50HL105188#6094 from the US National Institutes of Health during the writing of this article. The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012;307:483–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fryar CD, Carroll MD, Ogden CL. Prevalence of Obesity Among Children and Adolescents: United States, Trends 1963–1965 Through 2011–2012. National Center for Health Statistics: Atlanta, GA, 2014 [Google Scholar]
- 4.Reilly J, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int J Obes 2011;35:891–898 [DOI] [PubMed] [Google Scholar]
- 5.Daniels SR, Arnett DK, Eckel RH, et al. Overweight in children and adolescents: Pathophysiology, consequences, prevention, and treatment. Circulation 2005;111:1999–2012 [DOI] [PubMed] [Google Scholar]
- 6.Bhargava SK, Sachdev HS, Fall CH, et al. Relation of serial changes in childhood body-mass index to impaired glucose tolerance in young adulthood. N Engl J Med 2004;350:865–875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Freedman DS, Mei Z, Srinivasan SR, et al. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: The Bogalusa Heart Study. J Pediatr 2007;150:12–17 [DOI] [PubMed] [Google Scholar]
- 8.Engeland A, Bjørge T, Tverdal A, et al. Obesity in adolescence and adulthood and the risk of adult mortality. Epidemiology 2004;15:79–85 [DOI] [PubMed] [Google Scholar]
- 9.Bjørge T, Engeland A, Tverdal A, et al. Body mass index in adolescence in relation to cause-specific mortality: A follow-up of 230,000 Norwegian adolescents. Am J Epidemiol 2008;168:30–37 [DOI] [PubMed] [Google Scholar]
- 10.Koplan J, Liverman CT, Kraak VI. Preventing Childhood Obesity: Health in the Balance. National Academies Press: Washington D.C., 2005 [PubMed] [Google Scholar]
- 11.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2007;120:S164–S192 [DOI] [PubMed] [Google Scholar]
- 12.Lundahl A, Kidwell KM, Nelson TD. Parental underestimates of child weight: A meta-analysis. Pediatrics 2014;133:e689–e703 [DOI] [PubMed] [Google Scholar]
- 13.Barlow SE, Bobra SR, Elliott MB, et al. Recognition of childhood overweight during health supervision visits: Does BMI help pediatricians? Obesity (Silver Spring) 2007;15:225–232 [DOI] [PubMed] [Google Scholar]
- 14.Boyle M, Lawrence S, Schwarte L, et al. Health care providers' perceived role in changing environments to promote healthy eating and physical activity: Baseline findings from health care providers participating in the healthy eating, active communities program. Pediatrics 2009;123:S293–S300 [DOI] [PubMed] [Google Scholar]
- 15.Klein JD, Sesselberg TS, Johnson MS, et al. Adoption of body mass index guidelines for screening and counseling in pediatric practice. Pediatrics 2010;125:265–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hernandez RG, Cheng TL, Serwint JR. Parents' healthy weight perceptions and preferences regarding obesity counseling in preschoolers: Pediatricians matter. Clin Pediatr (Phila) 2010;49:790–798 [DOI] [PubMed] [Google Scholar]
- 17.Hardy LR, Harrell JS, Bell RA. Overweight in children: Definitions, measurements, confounding factors, and health consequences. J Pediatr Nurs 2004;19:376–384 [DOI] [PubMed] [Google Scholar]
- 18.Patrick H, Nicklas TA. A review of family and social determinants of children's eating patterns and diet quality. J Am Coll Nutr 2005;24:83–92 [DOI] [PubMed] [Google Scholar]
- 19.Towns N, D'Auria J. Parental perceptions of their child's overweight: An integrative review of the literature. J Pediatr Nurs 2009;24:115–130 [DOI] [PubMed] [Google Scholar]
- 20.McKee C, Long L, Southward LH, et al. The role of parental misperception of child's body weight in childhood obesity. J Pediatr Nurs 2016;31:196–203 [DOI] [PubMed] [Google Scholar]
- 21.Taveras EM, Hohman KH, Price SN, et al. Correlates of participation in a pediatric primary care-based obesity prevention intervention. Obesity (Silver Spring) 2011;19:449–452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Epstein LH, Myers MD, Raynor HA, et al. Treatment of pediatric obesity. Pediatrics 1998;101:554–570 [PubMed] [Google Scholar]
- 23.Golan M, Fainaru M, Weizman A. Role of behaviour modification in the treatment of childhood obesity with the parents as the exclusive agents of change. Int J Obes Relat Metab Disord 1998;22:1217–1224 [DOI] [PubMed] [Google Scholar]
- 24.Rhee KE, De Lago CW, Arscott-Mills T, et al. Factors associated with parental readiness to make changes for overweight children. Pediatrics 2005;116:e94–e101 [DOI] [PubMed] [Google Scholar]
- 25.Almoosawi S, Jones AR, Parkinson KN, et al. Parental perception of weight status: Influence on children's diet in the Gateshead Millennium Study. PLoS One 2016;11:e0144931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.He M, Evans A. Are parents aware that their children are overweight or obese? Do they care? Can Fam Physician 2007;53:1493–1499 [PMC free article] [PubMed] [Google Scholar]
- 27.Rietmeijer-Mentink M, Paulis WD, van Middelkoop M, et al. Difference between parental perception and actual weight status of children: A systematic review. Matern Child Nutr 2013;9:3–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Published 2016. Updated February 24, 2016. Available at www.cdc.gov/nchs/nhanes Last accessed August28, 2016
- 29.Centers for Disease Control and Prevention. NHANES Response Rates and Population Totals. Published 2015. Updated October 30, 2015. Available at www.cdc.gov/nchs/nhanes/response_rates_cps.htm Last accessed August28, 2016
- 30.Centers for Disease Control and Prevention. WEIGHT HISTORY—WHQ Target Group: SPs 8–15 years. Published 2015. Updated August 6, 2015. Available at www.cdc.gov/nchs/data/nhanes/nhanes_13_14/WHQ_CAPI_H.pdf Last accessed August28, 2016
- 31.Centers for Disease Control and Prevention. EARLY CHILDHOOD—ECQ Target Group: SPs Birth to 15 Years. Published 2015. Updated August 6, 2015. Available at www.cdc.gov/nchs/data/nhanes/nhanes_13_14/ECQ_H.pdf Last accessed August28, 2016
- 32.Ogden CL, Kuczmarski RJ, Flegal KM, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: Improvements to the 1977 National Center for Health Statistics version. Pediatrics 2002;109:45–60 [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey: Analytic Guidelines, 2011–2012. Published 2013. Updated September 30, 2013. Available at www.cdc.gov/nchs/data/nhanes/analytic_guidelines_11_12.pdf Last accessed August28, 2016
- 34.West DS, Raczynski JM, Phillips MM, et al. Parental recognition of overweight in school-age children. Obesity (Silver Spring) 2008;16:630–636 [DOI] [PubMed] [Google Scholar]
- 35.Davis MM, Gance-Cleveland B, Hassink S, et al. Recommendations for prevention of childhood obesity. Pediatrics 2007;120:S229–S253 [DOI] [PubMed] [Google Scholar]
- 36.Lu H, Tarasenko YN, Asgari-Majd FC, et al. More overweight adolescents think they are just fine: Generational shift in body weight perceptions among adolescents in the U.S. Am J Prev Med 2015;49:670–677 [DOI] [PubMed] [Google Scholar]
- 37.Hansen AR, Duncan DT, Tarasenko YN, et al. Generational shift in parental perceptions of overweight among school-aged children. Pediatrics 2014;134:481–488 [DOI] [PubMed] [Google Scholar]
- 38.Duncan DT, Hansen AR, Wang W, et al. Change in misperception of child's body weight among parents of American preschool children. Child Obes 2015;11:384–393 [DOI] [PubMed] [Google Scholar]
- 39.Hansen AR, Duncan DT, Baidal JA, et al. An increasing trend in health care professionals notifying children of unhealthy weight status: NHANES 1999–2014. Int J Obes 2016. [Epub ahead of print]; DOI: 10.1038/ijo.2016.85 [DOI] [PubMed] [Google Scholar]
- 40.Perrin EM, Skinner AC, Steiner MJ. Parental recall of doctor communication of weight status: national trends from 1999 through 2008. Arch Pediatr Adolesc Med 2012;166:317–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rossen LM, Tarasenko YN, Branum AM, et al. Abdominal adiposity and caregiver recall of healthcare provider identification of child overweight in the United States, 2001–2010. Child Obes 2013;9:418–426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sonneville KR, Thurston IB, Milliren CE, et al. Helpful or harmful? Prospective association between weight misperception and weight gain among overweight and obese adolescents and young adults. Int J Obes 2016;40:328–332 [DOI] [PubMed] [Google Scholar]
- 43.Gray WN, Crawford MJ, Follansbee-Junger K, et al. Associations between actual and perceived weight and psychosocial functioning in children: The importance of child perceptions. Child Obes 2012;8:147–154 [DOI] [PubMed] [Google Scholar]
- 44.US Preventive Services Task Force. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics 2010;125:361–367 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.