Abstract
Purpose
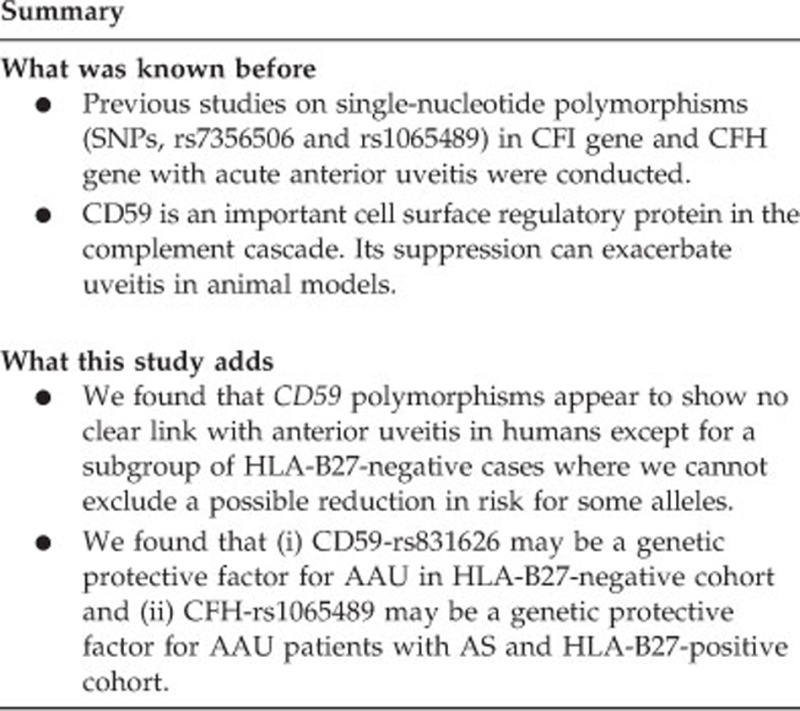
CD59 complement regulator and complement factor H (CFH) have important roles in complement activation pathways, which are known to affect the development of uveitis. The present study was performed to investigate whether an association exists between CD59 and CFH genetic polymorphisms and acute anterior uveitis (AAU).
Methods
A total of 600 individuals (300 patients diagnosed with AAU and 300 healthy controls) were recruited for this case–control study. Five single-nucleotide polymorphisms (SNPs) in CD59 (rs831626, rs12272807, rs831625, rs11585, and rs12576440) and CFH-rs1065489 were genotyped using Sequenom MassARRAY technology. Allele and genotype frequencies were statistically compared between patients and controls using χ2 test. Analyses were stratified for gender, human leukocyte antigen (HLA)-B27, and ankylosing spondylitis (AS) status.
Results
No significant association was found between any of the six polymorphisms and AAU. In HLA-B27-negative AAU patients, the frequencies of the G allele and GG homozygosity were lower in CD59-rs831626 when compared with controls (P=0.032). There were also significant decreases in the frequencies of T allele and TT homozygosity in CFH-rs1065489 in AAU patients with AS compared with controls (P=0.002). Furthermore, the frequencies of the T allele and TT homozygosity in CFH-rs1065489 were lower in the AAU male patients with AS compared with controls (P=0.015).
Conclusion
Our results revealed that SNPs CD59-rs831626 and CFH-rs1065489 were associated with the susceptibility of AAU. The influence on AAU could be gender specific and dependent on the HLA-B27 and AS status. No positive results were found in the overall group.
Introduction
Uveitis is a sight-threatening intraocular inflammatory disease that includes a diverse group of subtypes and is a major cause of visual impairment and blindness.1 It can be subdivided according to the following phenotypes: anterior uveitis (AU), intermediate uveitis, posterior uveitis, and panuveitis.1 Acute anterior uveitis (AAU) is the most common form of uveitis, with human leukocyte antigen (HLA)-B27-associated uveitis being the most common etiology of AAU.2 Moreover, there is strong association between ankylosing spondylitis (AS) and those patients with AAU, with approximately 15–50% developing AS.3
The exact pathogenesis of AAU is still unclear, but accumulating evidence has demonstrated that the disease is immune mediated and influenced by various endogenous factors.4, 5 For instance, studies have shown that single-nucleotide polymorphisms (SNPs) in TNF and their associated receptors are associated with AAU.6 The levels of CCL2, CCL5, and their receptors have also been found to be significantly correlated with the severity of inflammation in AAU patients.7 Moreover, the influence of genetic polymorphisms on uveitis might depend on the patient's HLA-B27 status.8 Thus, there is robust evidence showing that genetic factors have an important role in the development of AAU.
The complement system includes important innate factors that orchestrate endogenous immunological and inflammatory processes. It can be further divided into classical, lectin, and alternative pathways. Unwanted activities of the complement system have been found in association with various immune-related diseases.5 Recently, genetic studies have shown that polymorphisms within the complement system are associated with uveitis. Thompson et al9 revealed that carriage of the complement factor H (CFH) Y402H polymorphism in both alleles is associated with an increased risk for posterior uveitis and panuveitis presentation. To this end, Yang et al10 have reported that polymorphisms in both CFH and complement factor B are associated with AU. Complement factor I, which is a serine protease in the complement cascade, has been shown to be associated with AAU.11
As CD59 is a membrane-bound human complement regulatory protein, it has an important role in the terminal pathway of the complement cascade.12 CD59 binds to the C5b678 complex to prevent recruitment of C9. This subsequently prevents pore formation in order to regulate the formation of MAC. CD59 is expressed on most human cells, including the uveal tract and all layers of the retina.12, 13 The CD59 gene has also been shown to be associated with some immune-related diseases.14 To this end, suppression of complement regulatory proteins exacerbates experimental autoimmune anterior uveitis.15 CFH is a major regulatory protein in the complement system and it can limit the activation of C3 in the alternative pathway.12 Yang et al have reported that CFH-rs1065489 was associated with AU.8
Herein, for the purpose to have better understanding of the role of CD59, we investigated the association between CD59 polymorphisms and AAU. Moreover, CFH-rs1065489 was also genotyped for a replication study and deeper stratified analyses.
Materials and methods
Study subjects
A total of 300 AAU patients and 300 healthy adult controls were recruited in this study. All patients and controls were Han Chinese. We recruited the subjects during the period from 2009 to 2013, and all the subjects were from Division of Uveitis, The Eye Hospital of Wenzhou Medical University. The definition of AAU was based on the Standardization Uveitis Nomenclature classification, and the course of the disease was within 3 months. The subjects presented both for the first time and recurrent disease. Patients were diagnosed with AS using a CT analysis of the sacroiliac joint. Patients were excluded who had any other types of uveitis such as intermediate uveitis, posterior uveitis, and panuveitis including Vogt–Koyanagi–Harada syndrome, Behcet syndrome or where AAU was secondary to other intraocular inflammations. We investigated the family histories of each case, so we ensure that all the cases were unrelated to each other and to the controls. The controls were recruited from the eye clinics, The Eye Hospital of Wenzhou Medical University. All the controls were without history of AU or AS definitely. The controls were unrelated to the cases according to the family history. The HLA-B27 status was not tested in the controls. Previous studies reported that the background rate of HLA-B27 positive in Chinese population is 2.97%.16 This study was approved by the ethics committee of The Eye Hospital of Wenzhou Medical University. All participants gave their informed consent. The study procedures followed all ethical human guidelines established by the Declaration of Helsinki.
DNA extraction and genotyping
Genomic DNA was extracted from peripheral blood using a conventional DNA extraction kit (Simgen, Hangzhou, China) according to the manufacturer's instructions. A Nanodrop 2000 (Thermal Fisher Scientific, Wilmington, DE, USA) was utilized for quantifying all genomic DNA. Five SNPs (rs831626, rs12272807, rs831625, rs11585, and rs12576440) in CD59 and CFH-rs1065489 were genotyped using the Sequenom MassARRAY technology platform with iPLEXGOLD chemistry (Sequenom, San Diego, CA, USA). Genotyping analysis was performed using the iPLEX Gold SNP genotyping kit (Sequenom) as well as the software and equipment provided by the MassARRAY platform (Sequenom).
Statistical analysis
Hardy–Weinberg equilibrium was tested by χ2 test for genotype frequencies of the selected SNPs in the control group. Either the χ2 test or the Fisher's exact test was used to compare allelic and genotypic frequencies between AAU and controls. Dominant and recessive models were applied in the association analysis. Stratified analyses based on gender, AS, and HLA-B27 status were also performed. Odds ratios (ORs) and 95% confidence intervals (95% CI) were also calculated. P-value of <0.05 was considered statistically significant.
Results
Clinical observations
Of the 300 patients with AAU, 64.0% were men and 36.0% were women. The mean age of AAU patients was 40.9 years; 291 subjects were tested for HLA-B27, of whom 80.4% were positive and 19.6% were negative. Total 202 patients underwent CT examination and 39.6% were diagnosed with AS. The 300 control subjects included 66.0% males and 34.0% females. Thus, the gender ratio was approximately equal between both groups. The mean age of the controls was 69.5 years. The detailed clinical characteristics are presented in Table 1.
Table 1. Clinical characteristics of the investigated subjects.
|
AAU patients |
Controls |
|||
|---|---|---|---|---|
| n (range) | % | n (range) | % | |
| Number | 300 | 300 | ||
| Age (years) | 40.9 (6–79) | 69.5 (60–88) | ||
| Male | 192 | 64.0 | 198 | 66.0 |
| Female | 108 | 36.0 | 102 | 34.0 |
| HLA-B27 positive | 234 | 80.4 | NA | NA |
| HLA-B27 negative | 57 | 19.6 | NA | NA |
| AS complicated | 80 | 39.6 | NA | NA |
| AS not complicated | 122 | 60.4 | NA | NA |
Abbreviations: AAU, acute anterior uveitis; AS, ankylosing spondylitis; NA, not available.
Association of SNPs with AAU and stratified by gender and HLA-B27 status
All six genotyped SNPs in controls successfully conformed to Hardy–Weinberg equilibrium. No significant associations in either allelic or genotypic frequencies for the six SNPs were detected between AAU patients and controls (Table 2). Among the 300 AAU patients, 291 subjects were tested for HLA-B27, of which 234 (80.4%) were positive (156 males and 78 females) and 57 (19.6%) were negative (31 males and 26 females). In HLA-B27-negative AAU patients, there was a decreasing tendency in the frequencies of the G allele and GG homozygosity in CD59-rs831626 compared with controls (P=0.032, OR=0.53, 95% CI=0.302–0.956) (Table 3).
Table 2. Comparison of allele and genotype frequencies in AAU patients and controls.
| Gene | SNP | Genotype | AAU (n=300) | Controls (n=300) | P-value |
|---|---|---|---|---|---|
| CD59 | rs831626 | GG/AG/AA | 14/96/188 | 11/110/179 | 0.672 |
| rs12272807 | TT/CT/CC | 15/103/181 | 16/103/181 | 0.945 | |
| rs831625 | GG/CG/CC | 51/139/108 | 47/141/112 | 0.679 | |
| rs11585 | TT/CT/CC | 11/114/174 | 14/113/173 | 0.784 | |
| rs12576440 | GG/AG/AA | 0/27/272 | 0/27/273 | 1 | |
| CFH | rs1065489 | TT/GT/GG | 71/141/87 | 87/141/72 | 0.074 |
Abbreviations: AAU, acute anterior uveitis; SNP, single-nucleotide polymorphism.
Table 3. Comparison of allele and genotype frequencies in patients with AAU vs control subjects stratified by HLA-B27 status.
| Gene | SNP | Genotype | HLA-B27-positive AAU (n=234) | HLA-B27-negative AAU (n=57) | Controls (n=300) | P-valuea | P-valueb |
|---|---|---|---|---|---|---|---|
| CD59 | rs831626 | GG/AG/AA | 11/84/138 | 2/11/44 | 11/110/179 | 0.824 | 0.032 |
| rs12272807 | TT/CT/CC | 12/80/142 | 3/21/33 | 16/103/181 | 1.0 | 0.807 | |
| rs831625 | GG/CG/CC | 39/106/88 | 8/30/19 | 47/141/112 | 0.95 | 0.835 | |
| rs11585 | TT/CT/CC | 9/91/134 | 2/20/35 | 14/113/173 | 0.942 | 0.629 | |
| rs12576440 | GG/AG/AA | 0/23/211 | 0/4/53 | 0/27/273 | 0.772 | 0.804 | |
| CFH | rs1065489 | TT/GT/GG | 51/115/68 | 18/24/15 | 87/141/72 | 0.049 | 1.0 |
Abbreviations: AAU, acute anterior uveitis; CFH, complement factor H; SNP, single-nucleotide polymorphism.
P-values <0.05 considered to be statistically significant are shown in bold.
P-value for patients who were HLA-B27 positive vs controls.
P-value for patients who were HLA-B27 negative vs controls.
When the analyses were stratified on the basis of gender, there were no significant associations detected in either allelic or genotypic frequencies for the five CD59 SNPs and CFH-rs1065489 between (i) male AAU patients compared with male controls or (ii) female AAU patients compared with female controls (Table 4).
Table 4. Comparison of allele and genotype frequencies of CD59 and CFH SNPs in patients with AAU vs control subjects stratified by gender.
| Gene | SNP | Genotype | Male AAU patients (n=191) | Male controls (n=197) | Female AAU patients (n=107) | Female controls (n=101) | P-valuea | P-valueb |
|---|---|---|---|---|---|---|---|---|
| CD59 | rs831626 | GG/AG/AA | 10/55/125 | 7/73/117 | 4/41/62 | 4/37/60 | 0.428 | 0.907 |
| rs12272807 | TT/CT/CC | 11/69/111 | 12/61/124 | 4/33/70 | 4/41/56 | 0.493 | 0.234 | |
| rs831625 | GG/CG/CC | 32/84/74 | 27/100/70 | 19/54/34 | 19/41/41 | 1 | 0.427 | |
| rs11585 | TT/CT/CC | 8/78/105 | 9/77/111 | 3/35/69 | 5/35/61 | 0.933 | 0.468 | |
| rs12576440 | GG/AG/AA | 0/17/174 | 0/16/181 | 0/10/97 | 0/10/91 | 0.860 | 0.646 | |
| CFH | rs1065489 | TT/GT/GG | 45/92/54 | 55/96/46 | 26/48/33 | 31/44/26 | 0.222 | 0.281 |
Abbreviations: AAU, acute anterior uveitis; CFH, complement factor H; SNP, single-nucleotide polymorphism.
P-value for male AAU patients vs male controls.
P-value for female AAU patients vs female controls.
When the analyses of HLA-B27-positive and HLA-B27-negative AAU patients were further stratified on the basis of gender, no significant association in either allelic or genotypic frequencies was detected for the six SNPs (Supplementary Table S1).
Association between SNPs and AAU stratified by AS status
Among the 300 AAU patients, 202 patients underwent CT examination and 80 (39.6%) were diagnosed with AS (65 males and 15 females), with 122 (60.4%) found to be negative for AS (70 males and 52 females). When analyzed on the basis of AS status, there were no significant differences in either allelic or genotypic frequencies for any of the five SNPs in CD59 between AAU patients either with AS or without AS when compared with control subjects (Table 5). Notably, there was a significant decrease in the frequencies of T allele and TT homozygosity in CFH-rs1065489 in AAU patients with AS compared with controls (P=0.002, OR=0.572, 95% CI=0.401–0.817) (Table 5).
Table 5. Comparison of allele and genotype frequencies of CD59 and CFH SNPs in patients with AAU vs control subjects stratified by AS status.
| Gene | SNP | Genotype | AAU patients with AS (n=80) | AAU patients without AS (n=122) | Controls (n=300) | P-valuea | P-valueb |
|---|---|---|---|---|---|---|---|
| CD59 | rs831626 | GG/AG/AA | 5/28/47 | 7/40/74 | 11/110/179 | 0.670 | 0.927 |
| rs12272807 | TT/CT/CC | 8/31/41 | 4/34/84 | 16/103/181 | 0.077 | 0.112 | |
| rs831625 | GG/CG/CC | 10/35/35 | 23/55/43 | 47/141/112 | 0.274 | 0.534 | |
| rs11585 | TT/CT/CC | 6/33/41 | 2/42/78 | 14/113/173 | 0.225 | 0.145 | |
| rs12576440 | GG/AG/AA | 0/5/75 | 0/10/112 | 0/27/273 | 0.594 | 0.719 | |
| CFH | rs1065489 | GG/GT/TT | 32/34/14 | 37/60/25 | 72/141/87 | 0.002 | 0.058 |
Abbreviations: AAU, acute anterior uveitis; AS, ankylosing spondylitis; CFH, complement factor H; SNP, single-nucleotide polymorphism.
P-values <0.05 considered to be statistically significant are shown in bold.
P-value for AAU patients who were with AS vs controls.
P-value for AAU patients who were without AS vs controls.
The analyses of AAU patients with and without AS were then stratified on the basis of gender. In AAU male patients with AS, there was a lower proportion of the T allele and TT homozygosity in CFH-rs1065489 when compared with male controls (P=0.015, OR=0.604, 95%CI=0.403–0.907) (Supplementary Table S3).
There were also no significant associations in either allelic or genotypic frequencies for the all six SNPs between (i) male AAU patients without AS as compared with male controls or (ii) female AAU patients without AS as compared with female controls (Supplementary Table S4).
Discussion
Some studies have been conducted to report the association between polymorphisms in CD59 gene and age-related macular degeneration.17 However, it is still not clear whether CD59 influences the uveitis. In this study, we analyzed five SNPs in CD59 in Chinese population. Furthermore, a replication study of CFH-rs1065489 and AAU was also performed in this study.
In our study, no significant association was found between any of the six polymorphisms and AAU. The negative finding indicated that CD59 and CFH polymorphisms may not be associated with AAU. The possible reason is that any association may be obscured by the strength of the association with HLA-B27 or other factors so that a larger study would be needed. And the negative finding of CFH kept with previous report.8 Here, we showed that correlations of CD59-rs831626 and CFH-rs1065489 between AAU could be influenced by HLA-B27 status.18 HLA-B27 was the first factor proven to be associated with AU. Therefore, we analyzed the SNPs stratified for HLA-B27 status. Interestingly, in the HLA-B27-negative cohort, the G allele and GG homozygosity of CD59-rs831626 may be protective allele or genotype to AAU. HLA-B27 is unique HLA molecule for its association with AAU and other HLA-B27-related inflammatory diseases.18 The prominent B pocket of HLA-B27 in the antigen-binding groove is unique among all the HLA class I molecules, which may be critical for the binding of the hypothetical uveitogenic/arthritogenic peptide.19 In previous study, HLA-B27-positive AAU is a distinct clinical entity with characteristic clinical features that is usually distinguishable from its HLA-B27-negative cohorts.18 Besides, we also found that there was a trend toward lower T allele frequency in CFH-rs1065489 in HLA-B27-positive patients compared with controls (P=0.049). The finding for CFH also showed a trend supporting the previous finding, even though this is not strictly statistically significant.
AS is an inflammatory disorder of unknown origin, which primarily affects the axial skeleton, peripheral joints, and extra-articular structures.20 The most common extra-articular manifestation of AS is AAU.21 Thus, the SNPs were also analyzed depending on AS status. It is a crucial finding that the T allele and TT homozygosity in CFH-rs1065489 can reduce the risk of AAU in Chinese cohort with AS.
In the previous studies, gender can probably affect AAU in HLA status.22 Therefore, we tried to analyze HLA status and AS status stratified by gender. It is an interesting finding that CFH-rs1065489 was associated with the susceptibility to AAU in the Chinese male cohort with AS. The result indicates that the T allele and TT homozygosity of CFH-rs1065489 were demonstrated as protective allele or genotype in AAU.
Our study still has several limitations. First, the HLA-B27 and AS status was not tested in the controls. As our study showed, HLA -B27 status is such a strong association with AU; and therefore, it is deserved to divide the control subjects into groups by HLA-B27 and AS status in our further study. In addition, there was a significant different level of age between AAU patients and control subjects. As we known, age can probably affect the incidence of AAU. Finally, the relatively small sample size in the subgroup analyses will reduce the statistical power of the study, and therefore some modest associations could not be detected. Furthermore, we found that KIAA1549L is in linkage disequilibrium with the CD59, and a series of CFHR genes to CFH should be also investigated in our future studies.
In conclusion, this study demonstrates that the CD59-rs831626 and CFH-rs1065489 might be correlated with AAU depending on HLA-B27 and AS status. In our study, we found that the strength of association on CD59 is fairly weak, while the CFH-rs1065489 T allele is much stronger. To the best of our knowledge, the association between CD59 polymorphisms and AAU was investigated for the first time. The association between CFH-rs1065489 and AAU stratified for AS status was not reported previously. Our findings suggest that the influence of the complement genes on AAU could be dependent on HLA-B27 and AS status. The interaction between complement genes and HLA-B27 or AS in AAU patients should be further investigated.
Acknowledgments
We appreciate all patients and family members for their participation in this study. This study was supported by the National Key Basic Research Program (2013CB967502 to Z-BJ), National Natural Science Foundation of China (81371059 to Z-BJ), Zhejiang Provincial Natural Science Foundation of China (LR13H120001 to Z-BJ), Zhejiang Provincial Natural Science Foundation of China (LY15H120003 to YW), Key Research Program of the Eye hospital (YNZD201402 to YW), Wenzhou Science and Technology Foundation (Y20140358 to X-FH) and Innovation Research Program of the Eye hospital (YNCX201507 to X-FH).
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on Eye website (http://www.nature.com/eye)
Supplementary Material
References
- Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol 2005; 140(3): 509–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang JH, Wakefield D. Uveitis: a global perspective. Ocul Immunol Inflamm 2002; 10(4): 263–279. [DOI] [PubMed] [Google Scholar]
- Monnet D, Breban M, Hudry C, Dougados M, Brezin AP. Ophthalmic findings and frequency of extraocular manifestations in patients with HLA-B27 uveitis: a study of 175 cases. Ophthalmology 2004; 111(4): 802–809. [DOI] [PubMed] [Google Scholar]
- Nussenblatt RB, Gery I. Experimental autoimmune uveitis and its relationship to clinical ocular inflammatory disease. J Autoimmun 1996; 9(5): 575–585. [DOI] [PubMed] [Google Scholar]
- Yang MM, Lai TY, Luk FO, Pang CP. The roles of genetic factors in uveitis and their clinical significance. Retina 2014; 34(1): 1–11. [DOI] [PubMed] [Google Scholar]
- Xiang Q, Chen L, Fang J, Hou S, Wei L, Bai L et al. TNF receptor-associated factor 5 gene confers genetic predisposition to acute anterior uveitis and pediatric uveitis. Arthritis Res Ther 2013; 15(5): R113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chui JJ, Li MW, Di Girolamo N, Chang JH, McCluskey PJ, Wakefield D. Iris pigment epithelial cells express a functional lipopolysaccharide receptor complex. Invest Ophthalmol Vis Sci 2010; 51(5): 2558–2567. [DOI] [PubMed] [Google Scholar]
- Yang MM, Lai TY, Tam PO, Chiang SW, Ng TK, Rong SS et al. Association of CFH and SERPING1 polymorphisms with anterior uveitis. Br J Ophthalmol 2013; 97(11): 1475–1480. [DOI] [PubMed] [Google Scholar]
- Thompson IA, Liu B, Sen HN, Jiao X, Katamay R, Li Z et al. Association of complement factor H tyrosine 402 histidine genotype with posterior involvement in sarcoid-related uveitis. Am J Ophthalmol 2013; 155(6): 1068–1074 e1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang MM, Lai TY, Tam PO, Chiang SW, Ng TK, Liu K et al. Association of C2 and CFB polymorphisms with anterior uveitis. Invest Ophthalmol Vis Sci 2012; 53(8): 4969–4974. [DOI] [PubMed] [Google Scholar]
- Wang Y, Huang XF, Yang MM, Cai WJ, Zheng MQ, Mao G et al. CFI-rs7356506 is a genetic protective factor for acute anterior uveitis in Chinese patients. Br J Ophthalmol 2014; 98(11): 1592–1596. [DOI] [PubMed] [Google Scholar]
- Noris M, Remuzzi G. Overview of complement activation and regulation. Semin Nephrol 2013; 33(6): 479–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebrahimi KB, Fijalkowski N, Cano M, Handa JT. Oxidized low-density-lipoprotein-induced injury in retinal pigment epithelium alters expression of the membrane complement regulatory factors CD46 and CD59 through exosomal and apoptotic bleb release. Adv Exp Med Biol 2014; 801: 259–265. [DOI] [PubMed] [Google Scholar]
- Sivasankar B, Longhi MP, Gallagher KM, Betts GJ, Morgan BP, Godkin AJ et al. CD59 blockade enhances antigen-specific CD4+ T cell responses in humans: a new target for cancer immunotherapy? J Immunol 2009; 182(9): 5203–5207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha P, Bora PS, Bora NS. The role of complement system in ocular diseases including uveitis and macular degeneration. Mol Immunol 2007; 44(16): 3901–3908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Hongyan YP, Huang Xiangkun. The association of various forms of anterior uveitis with HLA-B27 antigen and its clinical implication. Chin Ophthal Res 2000; 18(3):197–196. [Google Scholar]
- Cipriani V, Matharu BK, Khan JC, Shahid H, Stanton CM, Hayward C et al. Genetic variation in complement regulators and susceptibility to age-related macular degeneration. Immunobiology 2012; 217(2): 158–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang JH, McCluskey PJ, Wakefield D. Acute anterior uveitis and HLA-B27. Surv Ophthalmol 2005; 50(4): 364–388. [DOI] [PubMed] [Google Scholar]
- Parham P. Structure of class-I MHC molecules: HLA-B27 and disease. Scand J Rheumatol 1990; 87(9): 11–20. [DOI] [PubMed] [Google Scholar]
- Calin A, Kennedy LG, Edmunds L, Will R. Familial versus sporadic ankylosing spondylitis. Two different diseases? Arthritis Rheum 1993; 36(5): 676–681. [DOI] [PubMed] [Google Scholar]
- Derhaag PJ, de Waal LP, Linssen A, Feltkamp TE. Acute anterior uveitis and HLA-B27 subtypes. Invest Ophthalmol Vis Sci 1988; 29(7): 1137–1140. [PubMed] [Google Scholar]
- Torres S, Borges S, Artiles A. HLA-B27 and clinical features of acute anterior uveitis in Cuba. Ocul Immunol Inflamm 2013; 21(2): 119–123. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


