Abstract
Background
The classification of alcohol use disorder has changed over the past century. Now, the conceptualization of alcohol dependence is still controversial. Accumulating evidence has shown the reliability and validity for the diagnosis of alcohol dependence in the ICD‐10 and DSM‐IV. However, the meaning and association of the respective diagnostic items, which are descriptive of representative symptoms, have hardly been examined. The core symptom of substance use disorder has been debated in various situations, but has never been elucidated logically.
Methods
We consecutively registered 192 patients with alcohol‐related problems who visited our hospital for the first time during a certain period. The relations and principal components among the checked items of the ICD‐10 diagnostic criteria were examined statistically.
Results
Three diagnostic items in the ICD‐10 were strongly correlated with each other and were thought to form the core symptoms of alcohol dependence: “strong desire,” “difficulties in controlling,” and “neglect of pleasures.” One major physical phenomenon, “withdrawal,” seemed to complement the core symptoms in the diagnosis of alcohol dependence. Another physical phenomenon, “tolerance,” was demonstrated to be a relatively independent item. The principal component analysis also demonstrated that the diagnostic item “difficulties in controlling” had the maximum component loading value, followed by 2 items, “neglect of pleasures” and “strong desire.”
Conclusions
The core symptomatic elements in the diagnosis of alcohol dependence were statistically suggested in this study. Knowledge of the relations and components among the diagnostic items of alcohol dependence might also be applicable to other forms of substance use dependence and behavioral addiction.
Keywords: Alcohol Dependence, Core Symptoms, ICD‐10, Principal Component, Analysis, Hepatic Markers
Diagnostic constructs that can be applied to repetitive substance use have developed over the past century. Various historical conceptualizations of substance use disorders have resulted in the International Classification of Diseases (ICD) and the Diagnostic and Statistical Manual Disorders (DSM; Saunders, 2006). The diagnoses of substance use disorders are psychometrically robust and clinically useful. In the current diagnostic and classification system, these disorders are defined and delineated on a phenomenological basis. Nevertheless, many alternative, even competing, schools of thought exist with regard to the nature of these conditions (Saunders, 2006). A detailed conceptualization of substance use disorders would be helpful in portraying the nature of these conditions.
The diagnostic criteria for substance use disorders have changed over several decades. The ICD‐10, completed in 1992, was modified based on the Edward & Gross conceptualization, which was published in 1976 as a provisional description of alcohol dependence syndrome (Edwards and Gross, 1976; Li et al., 2007; Saunders, 2006). The ICD has consistently accepted dependence syndrome as the central disease of substance use disorders. Meanwhile, the ICD has been naturally influenced by the DSM criteria. Outline of diagnostic guideline for dependence syndrome according to the ICD‐10 consists of 6 items: a strong desire or sense of compulsion (strong desire), difficulties in controlling substance‐taking behavior (difficulties in controlling), a physiological withdrawal state (withdrawal), evidence of tolerance (tolerance), progressive neglect of alternative pleasures or interests (neglect of pleasures), and persisting with substance use despite overtly harmful consequences (harmful consequences). The definitions of dependence syndromes in the ICD‐10 and DSM‐IV are psychometrically similar, and the differences are relatively small. The main conceptual difference is that in the ICD‐10, dependence syndrome includes the cognitive item, craving (strong desire).
Since its first publication in 1952, the DSM has been reviewed and revised several times. The first and second editions of the DSM grouped substance use disorders under the category of personality disorders and neurosis (Li et al., 2007). In the third edition (DSM‐III), published in 1980, substance use disorders were classified separately for the first time. Afterward, substance use disorders were conceptualized as a disease entity. A distinction was made between substance abuse and dependence in the DSM‐III. This distinction was retained in the DSM‐IV, which was published in 1994. Several studies examined the validity of distinctions between normality and abuse and between abuse and dependence. However, some studies found that a 1‐factor model fit the criteria best (Borges et al., 2010; Keyes et al., 2011; Saha et al., 2006; Shmulewitz et al., 2010). A unidimensionality was found for substance abuse and dependence in the DSM‐IV criteria with the exception of legal problems, indicating that dependence and the remaining abuse criteria share the same underlying condition (Hasin et al., 2013; Saha et al., 2006). Other studies supported models with 2 or more factors, although these factors did not accord with the DSM‐IV distinction between abuse and dependence (Grant et al., 2007; Harford and Muthen, 2001; Nelson et al., 1999). Therefore, substance abuse and dependence have been integrated into substance‐related disorders in the DSM‐5, which was published in 2013 (American Psychiatric Association, 2013). The meaning of craving as a criterion has been discussed, although craving has already been included in the dependence criteria in the ICD‐10. In preliminary studies, the addition of craving yielded a better continuous measure that differentiates individuals with and without alcohol problems along an alcohol use disorder continuum (Keyes et al., 2011; Murphy et al., 2014). The switch from the DSM‐IV to the DSM‐5 changed the prevalence of individuals with alcohol‐related problems and successfully incorporated diagnostic orphans into the diagnostic realm in primary studies (Agrawal et al., 2011; Bartoli et al., 2015).
Evidence regarding the reliability and validity of the ICD‐10 and DSM criteria for the diagnosis of alcohol use disorder has been accumulating (Grant et al., 2007; Hasin, 2003). The test–retest reliability of ICD‐10 dependence or DSM‐IV dependence for a variety of psychoactive substances was relatively high, with a kappa coefficient of 0.7 to 0.9 (kappa values of 0.75 and higher are interpreted as indicating excellent reliability, while kappa values of 0.60 to 0.74 indicate good reliability). However, the reliability of ICD‐10 “harmful use” or DSM‐IV “abuse” was notably lower than the reliability of dependence (Hasin, 2003). Similarly, while the validity of dependence against clinical and nonclinical data has been shown to be relatively high, the validity of harmful use or abuse has been substantially lower than dependence (Grant et al., 2007; Hasin, 2003; Saunders, 2006). The reliability and validity of the diagnostic instruments and constructed interviews for alcohol and drug dependence in the ICD‐10 and DSM have also been demonstrated (Dawson et al., 2012; Gerdner and Wickstrom, 2015; Ustun et al., 1997). Although the reliability and validity of the diagnosis of alcohol dependence have been proven, the magnitude of each criterion for the diagnosis of alcohol dependence has hardly been investigated. The contributions of the respective symptoms in alcohol dependence and abuse in the DSM‐IV to capture alcohol use disorders have been addressed in large general population samples in the United States using item response theory analysis (Dawson and Grant, 2010; Dawson et al., 2010; Saha et al., 2006). These studies have discussed whether dimensionality is required to assess subjects with alcohol problems and ordered relative severity of individual criteria. However, the diagnostic roles of the symptomatic items have never been discussed from the viewpoint of core symptoms.
The core symptoms of substance use disorder have been debated in various situations. Core features describe the “whatness” of a mental disorder and can be defined as the symptoms and constructs that index the internal dysfunction underlying the pathology rather directly (Martin et al., 2014). Craving, withdrawal, and tolerance have been empirically emphasized as candidates for the central element of substance use disorder (De Bruijn et al., 2004; Edwards and Gross, 1976; Hasin et al., 2000). The candidate symptoms have been proven to be predictors or risk factors of alcohol use disorder (Corbin et al., 2013; Hasin et al., 2000; Schneekloth et al., 2012). The relevance of these symptoms to the dependence mechanism has also been individually examined from genetic and neurobiological perspectives (Agrawal et al., 2013; Heinz et al., 2009; Hu et al., 2008; Seo and Sinha, 2014). However, evidence supporting candidates for the core symptoms has never been logically endorsed by practical methods. The core symptoms of substance dependence need to be identified, and which of the respective symptomatic items are really essential for the diagnosis of substance dependence should be verified.
For this purpose, the clarification of the associations among the respective symptomatic items and the identification of the core symptomatic component for the diagnosis of alcohol dependence are key research questions. We attempted to analyze statistically the correlations and magnitudes of the 6 representative symptomatic items for alcohol dependence in the ICD‐10, which were endorsed by treatment‐seeking patients. The ICD‐10 is commonly used at psychiatric clinics in Japan. In addition, the 6 items in the ICD‐10 will be integrated into 3 items in the proposed criteria for alcohol dependence in the ICD‐11 (Tyburski et al., 2014). Contrary to the DSM, the ICD criteria intend to refine and elaborate the concept of dependence. Thus, an analysis of the symptomatic items in the ICD‐10 seemed suitable for the present study.
Materials and methods
This study targeted treatment‐seeking patients visiting our hospital, the National Hospital Organization, Kurihama Medical and Addiction Center. The hospital is located near Tokyo and is recognized as a treatment center for addiction and dependence in Japan. The patients utilized various routes to treatment in the hospital. Some patients were refereed by physicians in general hospitals, where they had been followed for physical problems caused by excessive drinking. Some patients were brought by their spouses, who obtained the required information about alcohol treatment on the Internet. Some patients voluntarily visited our hospital following the recommendations of their bosses and colleagues or their relatives.
We consecutively registered patients with alcohol‐related problems between the ages of 22 and 90 years who had visited our hospital for the first time between January and March 2012. The 6 symptomatic items of the ICD‐10 criteria for alcohol dependence were checked at the time of the first visit in each case. The diagnostic criteria were ascertained on the basis of a nonstandardized psychiatric evaluation by 5 skilled specialists in alcohol treatment. We focused on the data in these study periods and collected the data 1 year later, because the data were filled without unreasonable leakage and considered to be more reliable.
One hundred and ninety‐two patients with alcohol‐related problems who had visited our hospital for the first time were registered successively in the present study. We attempted to evaluate all the patients according to the 6 symptomatic items of the ICD‐10 criteria for alcohol dependence. However, 9 patients could not be evaluated. Some of the patients did not have sufficient verbal communication abilities because of severe drunkenness or serious dementia. Others were uncooperative and refused medical interventions, as they had been forced to visit the hospital by their families.
All the patients also received laboratory examinations on the same day of their visit. Markers reflecting alcohol consumption, such as serum Aspartate Aminotransferase (AST), Alanine Aminotransferase (ALT), and Gamma‐Glutamyl Transpeptidase (GGT), were measured and used in the assessment. The median levels of these hepatic enzymes were calculated for groups classified according to the number of checked diagnostic items.
The correlations of the checked symptomatic items among the ICD‐10 diagnostic criteria were then examined statistically using chi‐square tests for the categorical variables. In this study, the null hypothesis that the presence of 1 criterion would not affect the likelihood of another was assumed. Thus, a smaller p value indicated stronger evidence that the 2 criteria were not independent of each other. The component loading of the respective ICD‐10 diagnostic criteria was analyzed using a categorical principal component analysis. The correlations between the median of the hepatic biomarkers and the number of the checked diagnostic items were analyzed using Spearman's rank correlation coefficients. The data analysis was performed using SPSS 19.0 software (IBM Corp., Armonk, NY). A significant level of p < 0.01 was used throughout the study. A level of 0.01 < p < 0.05 was considered to indicate a weak correlation in the study.
Results
Of the 192 patients, 183 patients were evaluated using the ICD‐10 criteria. The 183 subjects who were evaluated according to the ICD‐10 criteria were interviewed with regard to their alcohol intake, smoking habits, and other background characteristics (Table 1). Overall, 142 of the subjects were male and 41 were female. The average age of male patients (55.5 years) was significantly older than that of female patients (47.1 years). Two‐thirds of the subjects were smokers. About 20% of the subjects were divorced. Over 20% of the subjects were unemployed, and one‐third of the female subjects were housewives.
Table 1.
Baseline Characteristics of the Subjects Presented According to Sex
| Characteristics | Average ± SD or Frequency (%) | p | |||
|---|---|---|---|---|---|
| Sex | Total, 183 | Male, 142 (77.6%) | Female, 41 (22.4%) | ||
| Age (years) | 53.6 ± 14.5 | 55.5 ± 14.2 | 47.1 ± 13.5 | 0.001 | |
| Age at first drink (years) | 17.5 ± 3.1 | 17.4 ± 3.0 | 17.9 ± 3.2 | 0.303 | |
| Age at start of habitual drinking (years) | 25.4 ± 8.8 | 24.6 ± 8.0 | 28.2 ± 11.0 | 0.065 | |
| Smoking (%) | Smoking | 122 (66.7) | 99 | 23 | 0.059 |
| Cessation | 20 (10.9) | 17 | 3 | ||
| Nonsmoking | 39 (21.3) | 25 | 14 | ||
| Marriage (%) | Married | 106 (57.9) | 79 | 27 | 0.513 |
| Divorced | 37 (20.2) | 30 | 7 | ||
| Unmarried | 31 (16.9) | 26 | 5 | ||
| Bereaved | 3 (1.6) | 3 | 0 | ||
| Cohabitating | 5 (2.7) | 3 | 2 | ||
| Occupation (%) | Full time | 78 (42.6) | 66 | 12 | <0.001 |
| Part time | 10 (5.5) | 6 | 4 | ||
| Retired | 37 (20.2) | 34 | 3 | ||
| Unemployed | 42 (23.0) | 34 | 8 | ||
| Housewife | 14 (7.7) | 0 | 14 | ||
| Student | 1 (0.5) | 1 | 0 | ||
The titles of the columns are represented by the first letters of abbreviated labels of the respective criteria. Bold numbers indicate a significant correlation between the diagnostic items, while italicized numbers indicate a weak connection.
The number of checked items for the 183 patients with alcohol‐related problems are shown in Fig. 1. Overall, 162 patients satisfied the alcohol dependence criteria, since they had met 3 or more of the ICD‐10 criteria at some time during the previous year. The remaining 21 patients did not meet the criteria for alcohol dependence. Patients with 5 criteria were the most common (Fig. 1). Next, the proportion of patients exhibiting each diagnostic criterion was examined (Fig. 2). The criterion “difficulties in controlling” was the most widely observed criterion among the subjects. Over 60% of the subjects exhibited evidence of “tolerance.” Only half of the subjects exhibited the diagnostic item of “withdrawal.”
Figure 1.
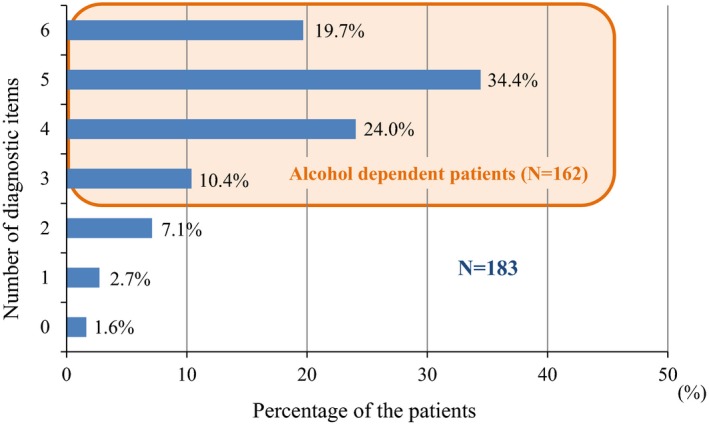
Percentage of each number of diagnostic items observed at the time of first visit among patients with alcohol‐related problems.
Figure 2.
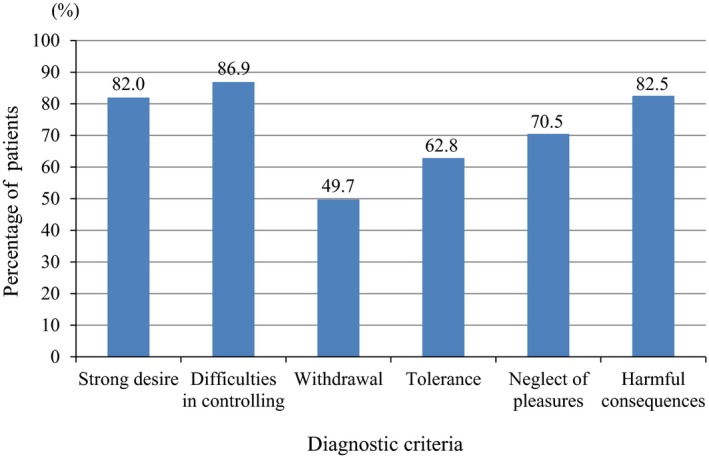
Percentage of patients corresponding to each diagnostic criterion.
We investigated the statistical relations among the checked diagnostic items in the ICD‐10 criteria. The correlations among the respective criteria were calculated by determining the p values (Table 2). In the table, bold numbers indicate a significant correlation between 2 items, while italicized numbers indicate a weak connection. The r values were calculated simultaneously and are described in parentheses in Table 2. Since categorical binary variables (0 or 1) were used in the analysis, the r values were relatively small.
Table 2.
Statistical Correlations Among the Observed Diagnostic Items According to the ICD‐10 Criteria Expressed by the p Values With the r Values in Parentheses
| Diagnostic items | S | D | W | T | N | H |
|---|---|---|---|---|---|---|
| Strong desire | – | 0.001 (0.239) | 0.004 (0.211) | 0.276 (0.081) | 0.008 (0.195) | 0.534 (0.046) |
| Difficulties in controlling | – | 0.002 (0.225) | 0.064 (0.137) | <0.001 (0.281) | 0.001 (0.247) | |
| Withdrawal | – | 0.389 (0.064) | 0.026 (0.164) | 0.257 (0.084) | ||
| Tolerance | – | 0.02 (0.172) | 0.655 (0.033) | |||
| Neglect of pleasures | – | 0.018 (0.175) | ||||
| Harmful consequences | – |
The titles of the columns are represented by the first letters of abbreviated labels of the respective criteria. Bold numbers indicate a significant correlation between the diagnostic items, while italicized numbers indicate a weak connection.
A correlation diagram was drawn based on the statistical correlations shown in Table 2 (Fig. 3). Significant correlations are indicated by solid lines, while a weak connection concerned with “tolerance” is indicated by the dotted line. Three diagnostic items in the ICD‐10—“strong desire,” “difficulties in controlling,” and “neglect of pleasures”—were strongly correlated with each other. In particular, “difficulties in controlling” was significantly correlated with 4 other items, which was the largest number of correlations: “strong desire,” “withdrawal,” “neglect of pleasures,” and “harmful consequences.” Therefore, the diagnostic item “difficulties in controlling” was regarded as having 4 arms and was placed in the center of the correlation diagram. “Tolerance” was the only item not correlated with “difficulties in controlling.”
Figure 3.
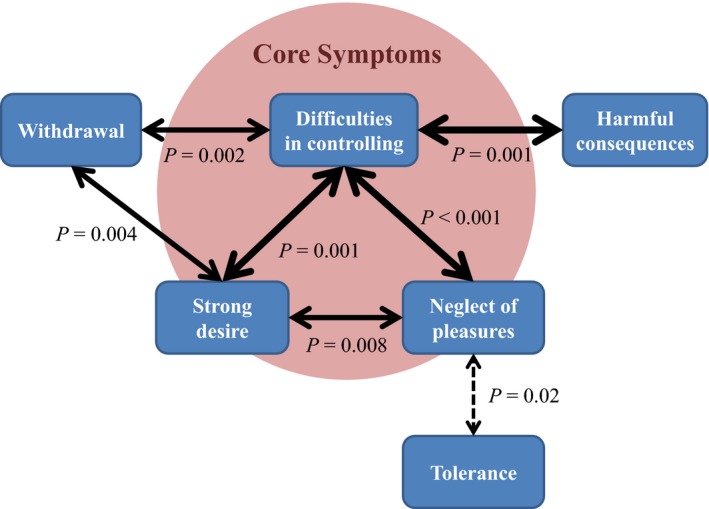
Correlation diagram showing diagnostic criteria items.
“Strong desire” was significantly correlated with 3 diagnostic items, which was the second largest number of correlations: “difficulties in controlling,” “withdrawal,” and “neglect of pleasures.” “Neglect of pleasures” was significantly correlated with 2 other diagnostic items (“strong desire” and “difficulties in controlling”) and was weakly connected with 3 items (“withdrawal,” “tolerance,” and “harmful consequences”; Table 2). “Neglect of pleasures” was the only item that was connected in some manner with all 5 other items.
Two diagnostic items, “withdrawal” and “harmful consequences,” were not as strongly correlated with the former 3 items (“strong desire,” “difficulties in controlling,” and “neglect of pleasures”). “Withdrawal” had 2 arms, indicating correlations with “strong desire” and “difficulties in controlling.” “Harmful consequences” had only 1 arm, indicating a correlation with “difficulties in controlling” in the correlation diagram. The last diagnostic item, “tolerance,” was minimally correlated with the other diagnostic items and was demonstrated to be a relatively independent item.
Furthermore, we performed a categorical principal component analysis to confirm the validity of the correlation diagram among the diagnostic criteria. The eigenvalue of the primary component was more than 1.0 (Table 3). This result means that the primary component could be largely attributed to the explanatory elements for patients with alcohol‐related problems. The primary component reasonably consisted of 6 diagnostic items in the ICD‐10 criteria. The component loading of the 6 items is shown in Table 3. The value for “difficulties in controlling” was highest and was more than 0.7. The importance of the diagnostic item “difficulties in controlling” for the diagnosis of alcohol dependence was also endorsed by this analysis. The value for “neglect of pleasures” was second to that of “difficulties in controlling.” “Strong desire” had the third largest score in the primary component loading analysis. The component loading value of “tolerance” was lowest and was <0.4.
Table 3.
Principal Component Analysis of the ICD‐10 Diagnostic Criteria
| Component | Eigenvalue | Proportion (%) |
|---|---|---|
| Primary component | 1.831 | 30.519 |
| Secondary component | 0.995 | 16.589 |
| Diagnostic items | Primary component loading |
|---|---|
| Strong desire | 0.549 |
| Difficulties in controlling | 0.711 |
| Withdrawal | 0.531 |
| Tolerance | 0.362 |
| Neglect of pleasures | 0.643 |
| Harmful consequences | 0.445 |
The validity was needed to endorse the judgments of assessors by using another method. All the patients received blood examinations when they visited our hospital for the first time. Hepatic markers, such as AST, ALT, and GGT, play a clinical role in the detection of drinking‐associated complications and comorbid conditions that may increase the risk of drinking (Conigrave et al., 2003). The medians of these markers were compared among groups that were classified according to the number of checked diagnostic items (Fig. 4). The number of diagnostic items was significantly correlated with elevated AST (p = 0.001), ALT (p = 0.016), and GGT (p < 0.001) values. These results indicate that the number of checked items validly reflected the severity of alcohol dependence and alcohol‐related problems.
Figure 4.
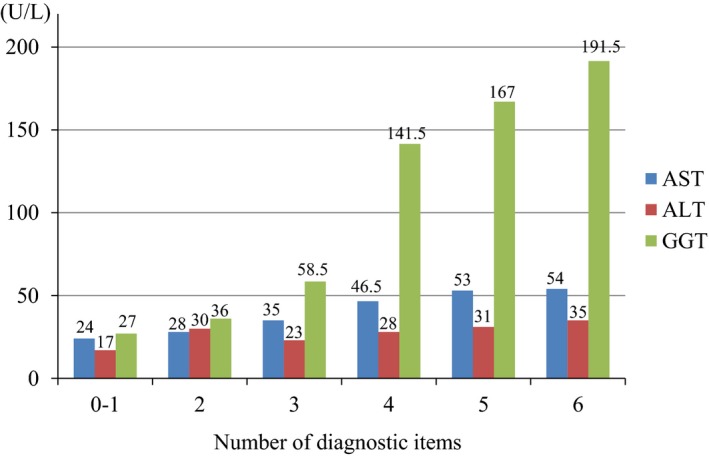
Median values of hepatic markers classified according to the number of checked diagnostic items.
Discussion
This study targeted treatment‐seeking patients with alcohol problems and statistically evaluated the correlations and magnitudes of checked diagnostic items of alcohol dependence in the ICD‐10. To our knowledge, it is the first study to address the diagnostic items endorsed by experienced treatment specialists and assess the characteristics of the diagnostic items targeting treatment‐seeking patients. The validity of the endorsed diagnostic items was confirmed by hepatic markers in the blood that were concurrently examined.
As mentioned in the introduction, a unidimensional concept of substance use disorder has been widely held based on a great deal of evidence, and a single diagnostic criterion was adopted in the DSM‐5 (Hasin, 2015). The principal component analysis in this study also indicated that the 6 criteria items formed a single broad superordinate factor. This finding did not contradict previously reported work (Saha et al., 2006; Borges et al., 2010).
Three diagnostic items in the ICD‐10, “strong desire,” “difficulties in controlling,” and “neglect of pleasures,” were strongly correlated with each other and were considered to form the core symptoms for the diagnosis of alcohol dependence. In particular, the diagnostic item “difficulties in controlling” was the most broadly observed among the subjects and was placed in the center of the correlation diagram. Moreover, the principal component analysis also demonstrated that “difficulties in controlling” had the highest component loading value, followed by “neglect of pleasures” and “strong desire.” These results did not conflict with the theory that the diagnostic items “strong desire,” “difficulties in controlling,” and “neglect of pleasures” form the core symptoms for the diagnosis of alcohol dependence. Since “neglect of pleasures” was connected with the other 5 items and had the second largest component value, “neglect of pleasures” was thought to play an important role in the diagnosis of alcohol dependence, as was “difficulties in controlling.” “Strong desire” had 3 correlations with other diagnostic items and a particularly strong correlation with “difficulties in controlling.” Certainly, a strong desire is considered to easily lead to difficulties in controlling drinking based on clinical impressions. Thus, a strong desire has been integrated into the diagnostic item “difficulties in controlling substance‐taking behavior” in the proposed ICD‐11 criteria (Tyburski et al., 2014). The present results also indicated that “strong desire” was fairly cooperative with “difficulties in controlling.”
The strong desire or sense of compulsion, that is, craving, has been discussed as a substance use disorder criterion. This symptom was included among the dependence criteria in the ICD‐10, but was excluded in the DSM‐IV. Evidence of craving as a treatment target for alcohol use disorder has been accumulating (O'Brien, 2005; Schneekloth et al., 2012; Subbaraman et al., 2013). Recently, anticraving drugs, such as naltrexone and nalmefene, have been shown to be effective for the reduction of drinking and the maintenance of abstinence in the pharmacological treatment of alcohol use disorder (Garbutt et al., 1999; O'Brien, 2005; Paille and Martini, 2014). Support for craving as a criterion comes indirectly from behavioral, imaging, and genetic studies (Heinz et al., 2009; Seo and Sinha, 2014). On the other hand, whether craving should be included as a criterion has remained uncertain, because craving can persist long into remission (Li et al., 2015; Pickens et al., 2011). While the psychometric benefit in adding a craving criterion has been equivocal, the opinion that craving may become important as a biological treatment target has prevailed. A craving criterion was thus included for substance use disorder in the DSM‐5 (American Psychiatric Association, 2013) and was found to be included among the core diagnostic items in the present study.
The diagnostic item “withdrawal” was somewhat correlated with the former 3 items and seemed to complement the core symptoms in the diagnosis of alcohol dependence. In fact, “withdrawal” had intermediate component loading values. Withdrawal syndrome has been considered the key element in characterizing alcohol dependence. Indeed, withdrawal syndrome facilitates more drinking to relieve uncomfortable withdrawal sensations and leads to the development of dependency. A great deal of evidence regarding the biological mechanism of withdrawal syndrome has been accumulated using various study methods (Moonat et al., 2010; Pandey et al., 2008). The biological mechanism of withdrawal suggests that the development of withdrawal syndrome depends on the amount of recently consumed substance and the clinical characteristics of individuals (Eyer et al., 2011). Although withdrawal syndrome certainly contributes to the development of dependency, the syndrome might not play a central role in the diagnosis of alcohol dependence and might rather complement the diagnostic role of the core symptomatic items. Actually, only half of the subjects exhibited the diagnostic item “withdrawal” in this study.
The last diagnostic item, “tolerance,” was minimally related to the other diagnostic items and was demonstrated to be a relatively independent item. “Tolerance” was shown to have the lowest component loading value among the 6 criteria in the ICD‐10. These results suggested that the diagnostic item “tolerance” has a minimal contribution to the diagnosis of alcohol dependence. Tolerance develops over the time course of repeated drinking episodes and might play an important role in the escalation to heavy drinking and the formation of alcohol dependence (Corbin et al., 2013; Ghezzi et al., 2013; Hu et al., 2008). Although acquired tolerance predicts alcohol‐related problems and facilitates the development of dependency (Corbin et al., 2013; Schuckit et al., 2008), whether or not evidence of tolerance exists might not be essential for a diagnosis. When patients with alcohol‐related problems visit a hospital, a definite diagnosis of alcohol dependence is performed from a cross‐sectional viewpoint. The acquired tolerance of the patients might have been lost at the time of the hospital visit because of their poor physical conditioning or age‐related declines (Ziolkowski et al., 1995). A previous factor analysis suggested that tolerance, withdrawal syndrome, and impaired control items could be identified as separate factors (Muthen et al., 1993). The evidence of this previous factor analysis targeting current drinkers was compatible with the results of the present study targeting treatment‐seeking patients with alcohol‐related problems.
In the present study, the percentages of diagnostic items that were exhibited differed substantially (Fig. 2). The percentages of the checked items “strong desire,” “difficulty in controlling,” and “harmful consequences” were each over 80%. The percentage of “neglect of pleasures” was about 70%. Unexpectedly, the percentage of “withdrawal” did not reach 50% and was less than those of the other diagnostic items. The proportion of endorsed diagnostic items had been examined using data from the 1991 to 1992 National Longitudinal Alcohol Epidemiologic Survey (NLAES) and the 2001 to 2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), which featured a representative sample of U.S. adults (Dawson and Grant, 2010; Dawson et al., 2010). We cannot easily compare the present study with these analyses performed in the United States, however, because the analyses were based on self‐reports and targeted past‐year drinkers and individuals with past‐year alcohol use disorder and because they were analyzed using the diagnostic items for alcohol dependence and abuse in the DSM‐IV. Nevertheless, the proportion of “difficulties in controlling” endorsed by treatment‐seeking patients in this study was prevalent, as well as the corresponding items in the DSM‐IV reported in these large‐scale studies in the United States. The proportions of 2 physiological items, “withdrawal” and “tolerance,” endorsed in this study were lower than that of “difficulties in controlling,” and these findings were similar to the results of the previous U.S. studies. While the proportions of “neglect of pleasures” and “harmful consequences” were quite high in the present study, the corresponding criteria in the DSM‐IV were rather less prevalent and had high severity threshold parameters in the analyses of the collected data from NESARC (Dawson et al., 2010). The difference seems to be mainly attributable to differences in the subjects among the studies. The diagnostic items “neglect of pleasures” and “harmful consequences” latently reflect alcohol‐related problems suffered by the subjects and their families that drove the subjects to visit hospitals. Therefore, treatment‐seeking patients might have a tendency to endorse the items, “neglect of pleasures” and “harmful consequences.” In particular, the diagnostic item “harmful consequences” depends on the subjects’ circumstances, because they must be made aware of the nature or extent of the harm caused by their drinking by people who are familiar to them. If subjects who have suffered from physical or psychological problems and have realized that their problems are caused by drinking continue to have difficulties in controlling their drinking, they are very likely to involve diagnostic items “difficulties in controlling” and “harmful consequences.” Therefore, “harmful consequences” was only significantly correlated with “difficulties in controlling” and might only supplement the diagnostic role of “difficulties in controlling.”
Our study design created some methodological limitations. The first limitation was the accuracy with which the ICD‐10 assessment could be conducted. All the subjects were assessed by 5 specialists, each with experience treating hundreds or thousands of alcohol‐dependent patients. Although the diagnostic standard based on the ICD‐10 criteria differs slightly in each case, the difference would be less noticeable in a large sample. Actually, the validity of the assessment was objectively confirmed by correlations between hepatic markers and the number of checked items. Second, all the patients including those who did not meet the criteria for alcohol dependence were analyzed in this study. When 162 alcohol‐dependent patients among the 183 subjects were analyzed separately, the correlation among the 6 diagnostic items was obscured (data not shown), partly because the increase in the proportions of endorsed diagnostic items masked the correlations. However, the 21 patients who did not meet 3 or more criteria had visited our hospital because of serious alcohol‐related problems such as insomnia, depression, cognitive dysfunction, blackouts, violence, or drunken driving. The ICD‐10 criteria for alcohol dependence do not always cover patients with severe alcohol problems. Thus, it seemed reasonable to include them in the present analysis. Third, the criteria that reflect the consequences of substance use are substantially conditioned by social and cultural circumstances (Martin et al., 2014; Room, 2006). The consequences are explicit for the diagnostic item “harmful consequences” and implicit to varying extents for “neglect of pleasures,” most notably for “increased amount of time” around the substance. Where the substance is readily and widely available, the issue of time spent seems irrelevant to informants (Room, 2006). Alcohol consumption is very acceptable in Japanese society. Drinking parties are common activities that are used to strengthen social and business ties. Therefore, the evaluation of diagnostic thresholds for the items “neglect of pleasures” and “harmful consequences” might be influenced by a higher societal tolerance in the present study, compared with the thresholds in other countries. Fourth, the present study explored the core symptoms from only 6 symptomatic items represented in the ICD‐10. The representative 6 items have inherited the elements suggested by Edwards and Gross (1976) and have been developed to capture the precise criteria of alcohol dependence. The representative 6 items have been rigorously resolved into more symptomatic elements (Dawson and Grant, 2010; Muthen et al., 1993). Whereas the use of multiple symptom items would be desirable of yielding more reliable and valid criterion measures, the inclusion of highly correlated symptom items contributes little above and beyond the existent criteria items (Dawson and Grant, 2010). Nevertheless, caution is needed to ensure that the core symptomatic items were indicated based only on what was assessed. It would be necessary to be careful of the possibility of allosteric symptomatic items. Fifth, the core characteristics of alcohol dependence should be determined based on all accumulated evidence to generalize across diverse samples. This study was based on a relatively small Japanese clinical sample and might have contained many severe cases. Actually, since about 20% of the subjects were divorced and over 20% of the subjects were unemployed, the subjects’ social positions were thought to be relatively unstable. Other studies targeting larger samples of treatment‐seeking patients or heavy drinkers in other countries are anticipated. Sixth, we examined the correlation of symptoms using manual calculations partly because only 6 symptomatic items were targeted and analyzed in the present study. Recently, new statistical approaches, such as network theory and graph theory, have been increasingly used to address symptom networks (Boschloo et al., 2015). These techniques have been used in the field of substance use disorders (Rhemtulla et al., 2016). Since these new methods would be very helpful for identifying items that appear to influence each other among numerous factors, these methods seem to be promising for addressing the relations and centrality of symptoms and for revising our conceptualization of psychiatric disorders and comorbidities. Seventh, a recent study exhibited a low consistency in the ordering of the severity of individual criteria for alcohol use disorders across studies (Lane et al., 2016). The diagnostic instruments that were used were found to be a large source of this inconsistency. Although the diagnostic criteria for alcohol dependence in the ICD‐10 were used in this study, studies using different diagnostic instruments might undermine the reproducibility of the present study. Therefore, further studies using other methodological variables, such as samples and assessment instruments, would help to advance research in this area.
The present study explored the core diagnostic items associated with patients visiting a treatment center. The statistical analysis demonstrated the strong correlations of 3 diagnostic items, “strong desire,” “difficulties in controlling,” and “neglect of pleasures.” The loading values of the 3 diagnostic items quantitatively gained a large share in the principal component analysis. The core symptomatic elements in the diagnosis of alcohol dependence were statistically suggested in this study. We speculated that the relations and components among the diagnostic items of alcohol dependence might also be applicable to other forms of substance use dependence and behavioral addiction.
Declarations of Competing Interest
None.
Acknowledgments
We are grateful to the following researchers for their contributions to this study: Hitoshi Maesato, MD, Hideki Nakayama, MD, Hisakazu Nakayama, MD, Tsuyoshi Takimura, MD.
The copyright line for this article was changed on 07 October 2016 after original online publication.
References
- Agrawal A, Heath AC, Lynskey MT (2011) DSM‐IV to DSM‐5: the impact of proposed revisions on diagnosis of alcohol use disorders. Addiction 106:1935–1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal A, Wetherill L, Bucholz KK, Kramer J, Kuperman S, Lynskey MT, Nurnberger JI Jr, Schuckit M, Tischfield JA, Edenberg HJ, Foroud T, Bierut LJ (2013) Genetic influences on craving for alcohol. Addict Behav 38:1501–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders, 5th ed American Psychiatric Publishing, Arlington, VA. [Google Scholar]
- Bartoli F, Carra G, Crocamo C, Clerici M (2015) From DSM‐IV to DSM‐5 alcohol use disorder: an overview of epidemiological data. Addict Behav 41:46–50. [DOI] [PubMed] [Google Scholar]
- Borges G, Ye Y, Bond J, Cherpitel CJ, Cremonte M, Moskalewicz J, Swiatkiewicz G, Rubio‐Stipec M (2010) The dimensionality of alcohol use disorders and alcohol consumption in a cross‐national perspective. Addiction 105:240–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boschloo L, Van Borkulo CD, Rhemtulla M, Keyes KM, Borsboom D, Schoevers RA (2015) The network structure of symptoms of the diagnostic and statistical manual of mental disorders. PLoS One 10:E0137621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conigrave KM, Davies P, Haber P, Whitfield JB (2003) Traditional markers of excessive alcohol use. Addiction 98:31–43. [DOI] [PubMed] [Google Scholar]
- Corbin WR, Scott C, Leeman RF, Fucito LM, Toll BA, O'Malley SS (2013) Early subjective response and acquired tolerance as predictors of alcohol use and related problems in a clinical sample. Alcohol Clin Exp Res 37:490–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Grant BF (2010) Should symptom frequency be factored into scalar measures of alcohol use disorder severity? Addiction 105:1568–1579. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Saha TD, Grant BF (2010) A multidimensional assessment of the validity and utility of alcohol use disorder severity as determined by item response theory models. Drug Alcohol Depend 107:31–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Smith SM, Saha TD, Rubinsky AD, Grant BF (2012) Comparative performance of the audit‐c in screening for DSM‐IV and DSM‐5 alcohol use disorders. Drug Alcohol Depend 126:384–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bruijn C, Korzec A, Koerselman F, Van Den Brink W (2004) Craving and withdrawal as core symptoms of alcohol dependence. J Nerv Ment Dis 192:494–502. [DOI] [PubMed] [Google Scholar]
- Edwards G, Gross MM (1976) Alcohol dependence: provisional description of a clinical syndrome. Br Med J 1:1058–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyer F, Schuster T, Felgenhauer N, Pfab R, Strubel T, Saugel B, Zilker T (2011) Risk assessment of moderate to severe alcohol withdrawal‐predictors for seizures and delirium tremens in the course of withdrawal. Alcohol Alcohol 46:427–433. [DOI] [PubMed] [Google Scholar]
- Garbutt JC, West SL, Carey TS, Lohr KN, Crews FT (1999) Pharmacological treatment of alcohol dependence: a review of the evidence. JAMA 281:1318–1325. [DOI] [PubMed] [Google Scholar]
- Gerdner A, Wickstrom L (2015) Reliability of ADDIS for diagnoses of substance use disorders according to ICD‐10, DSM‐IV and DSM‐5: test‐retest and inter‐item consistency. Subst Abuse Treat Prev Policy 10:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghezzi A, Krishnan HR, Lew L, Prado FJ 3rd, Ong DS, Atkinson NS (2013) Alcohol‐induced histone acetylation reveals a gene network involved in alcohol tolerance. PLoS Genet 9:E1003986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Muthen BO, Yi HY, Hasin DS, Stinson FS (2007) DSM‐IV alcohol dependence and abuse: further evidence of validity in the general population. Drug Alcohol Depend 86:154–166. [DOI] [PubMed] [Google Scholar]
- Harford TC, Muthen BO (2001) The dimensionality of alcohol abuse and dependence: a multivariate analysis of DSM‐IV symptom items in the national longitudinal survey of youth. J Stud Alcohol 62:150–157. [DOI] [PubMed] [Google Scholar]
- Hasin D (2003) Classification of alcohol use disorders. Alcohol Res Health 27:5–17. [PMC free article] [PubMed] [Google Scholar]
- Hasin D (2015) DSM‐5 SUD diagnoses: changes, reactions, remaining open questions. Drug Alcohol Depend 148:226–229. [PubMed] [Google Scholar]
- Hasin DS, O'Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, Compton WM, Crowley T, Ling W, Petry NM, Schuckit M, Grant BF (2013) DSM‐5 criteria for substance use disorders: recommendations and rationale. Am J Psychiatry 170:834–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D, Paykin A, Meydan J, Grant B (2000) Withdrawal and tolerance: prognostic significance in DSM‐IV alcohol dependence. J Stud Alcohol 61:431–438. [DOI] [PubMed] [Google Scholar]
- Heinz A, Beck A, Grusser SM, Grace AA, Wrase J (2009) Identifying the neural circuitry of alcohol craving and relapse vulnerability. Addict Biol 14:108–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu W, Saba L, Kechris K, Bhave SV, Hoffman PL, Tabakoff B (2008) Genomic insights into acute alcohol tolerance. J Pharmacol Exp Ther 326:792–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Krueger RF, Grant BF, Hasin DS (2011) Alcohol craving and the dimensionality of alcohol disorders. Psychol Med 41:629–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane SP, Steinley D, Sher KJ (2016) Meta‐analysis of DSM alcohol use disorder criteria severities: structural consistency is only ‘skin deep’. Psychol Med 46:1769–1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li TK, Hewitt BG, Grant BF (2007) The alcohol dependence syndrome, 30 years later: a commentary. The 2006 H David Archibald Lecture. Addiction 102:1522–1530. [DOI] [PubMed] [Google Scholar]
- Li P, Wu P, Xin X, Fan YL, Wang GB, Wang F, Ma MY, Xue MM, Luo YX, Yang FD, Bao YP, Shi J, Sun HQ, Lu L (2015) Incubation of alcohol craving during abstinence in patients with alcohol dependence. Addict Biol 20:513–522. [DOI] [PubMed] [Google Scholar]
- Martin CS, Langenbucher JW, Chung T, Sher KJ (2014) Truth or consequences in the diagnosis of substance use disorders. Addiction 109:1773–1778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moonat S, Starkman BG, Sakharkar A, Pandey SC (2010) Neuroscience of alcoholism: molecular and cellular mechanisms. Cell Mol Life Sci 67:73–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy CM, Stojek MK, Few LR, Rothbaum AO, Mackillop J (2014) Craving as an alcohol use disorder symptom in DSM‐5: an empirical examination in a treatment‐seeking sample. Exp Clin Psychopharmacol 22:43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen BO, Hasin D, Wisnicki KS (1993) Factor analysis of ICD‐10 symptom items in the 1988 National Health Interview Survey on Alcohol Dependence. Addiction 88:1071–1077. [DOI] [PubMed] [Google Scholar]
- Nelson CB, Rehm J, Ustun TB, Grant B, Chatterji S (1999) Factor structures for DSM‐IV substance disorder criteria endorsed by alcohol, cannabis, cocaine and opiate users: results from the WHO reliability and validity study. Addiction 94:843–855. [DOI] [PubMed] [Google Scholar]
- O'Brien C P (2005) Anticraving medications for relapse prevention: a possible new class of psychoactive medications. Am J Psychiatry 162:1423–1431. [DOI] [PubMed] [Google Scholar]
- Paille F, Martini H (2014) Nalmefene: a new approach to the treatment of alcohol dependence. Subst Abuse Rehabil 5:87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandey SC, Ugale R, Zhang H, Tang L, Prakash A (2008) Brain chromatin remodeling: a novel mechanism of alcoholism. J Neurosci 28:3729–3737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickens CL, Airavaara M, Theberge F, Fanous S, Hope BT, Shaham Y (2011) Neurobiology of the incubation of drug craving. Trends Neurosci 34:411–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhemtulla M, Fried EI, Aggen SH, Tuerlinckx F, Kendler KS, Borsboom D (2016) Network analysis of substance abuse and dependence symptoms. Drug Alcohol Depend 161:230–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Room R (2006) Taking account of cultural and societal influences on substance use diagnoses and criteria. Addiction 101:31–39. [DOI] [PubMed] [Google Scholar]
- Saha TD, Chou SP, Grant BF (2006) Toward an alcohol use disorder continuum using item response theory: results from the national epidemiologic survey on alcohol and related conditions. Psychol Med 36:931–941. [DOI] [PubMed] [Google Scholar]
- Saunders JB (2006) Substance dependence and non‐dependence in the Diagnostic and Statistical Manual of Mental Disorders (DSM) and the International Classification of Diseases (ICD): can an identical conceptualization be achieved? Addiction 101:48–58. [DOI] [PubMed] [Google Scholar]
- Schneekloth TD, Biernacka JM, Hall‐Flavin DK, Karpyak VM, Frye MA, Loukianova LL, Stevens SR, Drews MS, Geske JR, Mrazek DA (2012) Alcohol craving as a predictor of relapse. Am J Addict 21:S20–S26. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Smith TL, Hesselbrock V, Bucholz KK, Bierut L, Edenberg H, Kramer J, Longacre E, Fukukura T, Kalmijn J, Danko GP, Trim R (2008) Clinical implications of tolerance to alcohol in nondependent young drinkers. Am J Drug Alcohol Abuse 34:133–149. [DOI] [PubMed] [Google Scholar]
- Seo D, Sinha R (2014) The neurobiology of alcohol craving and relapse. Handb Clin Neurol 125:355–368. [DOI] [PubMed] [Google Scholar]
- Shmulewitz D, Keyes K, Beseler C, Aharonovich E, Aivadyan C, Spivak B, Hasin D (2010) The dimensionality of alcohol use disorders: results from israel. Drug Alcohol Depend 111:146–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS, Lendle S, Van Der Laan M, Kaskutas LA, Ahern J (2013) Cravings as a mediator and moderator of drinking outcomes in the combine study. Addiction 108:1737–1744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyburski EM, Sokolowski A, Samochowiec J, Samochowiec A (2014) New diagnostic criteria for alcohol use disorders and novel treatment approaches—2014 update. Arch Med Sci 10:1191–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ustun B, Compton W, Mager D, Babor T, Baiyewu O, Chatterji S, Cottler L, Gogus A, Mavreas V, Peters L, Pull C, Saunders J, Smeets R, Stipec MR, Vrasti R, Hasin D, Room R, Van Den Brink W, Regier D, Blaine J, Grant BF, Sartorius N (1997) WHO study on the reliability and validity of the alcohol and drug use disorder instruments: overview of methods and results. Drug Alcohol Depend 47:161–169. [DOI] [PubMed] [Google Scholar]
- Ziolkowski M, Maludzinska E, Gruss T, Rybakowski J, Volpicelli JR (1995) Decrease in alcohol tolerance: clinical significance in alcohol dependence. Drug Alcohol Depend 39:33–36. [DOI] [PubMed] [Google Scholar]


