Abstract
PURPOSE
To evaluate osteoporosis knowledge and learning needs in healthcare professionals working with patients who have experienced or are at risk of fracture.
SETTING
Multisite teaching hospital, Hamilton, Ontario.
SAMPLE
Healthcare professionals working in the fracture clinics, orthopaedics, rehabilitation, and nuclear medicine department.
METHOD
Completion of an Osteoporosis Knowledge Questionnaire and questions about learning needs and preferences.
RESULTS
The major areas of knowledge deficit in this study were with topics related to health promotion and management specific to calcium needs and medications.
CONCLUSIONS
The range of scores on the Osteoporosis Knowledge Questionnaire and the low scores on key questions suggest that there are opportunities to increase osteoporosis knowledge across a broad spectrum of healthcare providers.
Introduction
Osteoporosis has been defined as a skeletal disorder characterized by compromised bone strength, predisposing a person to an increased risk of fracture (2000). The annual cost of care associated with hip fracture in Canada has been estimated at $650 million (Wiktorowicz, Goeree, Papaioannou, Adachi, & Papadimitropoulos, 2001). In the United States, this figure is significantly higher with estimates as high as $13.8 billion (Ray, Chan, Thamer, & Melton, 1997). Fragility fractures also impose human costs including limited mobility, pain, and increased mortality (Adachi et al., 2001; Papaioannou et al., 2002). A history of prior fracture has been shown to be an independent predictor of subsequent fractures at any site (Kanis et al., 2004). Therefore, it is essential that individuals who experience a fragility fracture are assessed and treated for osteoporosis. Therapeutic options can reduce the number of new vertebral compression fractures by 40–60% within the first year in individuals with a fracture (Brown & Josse, 2002). However, many fragility fracture patients are being overlooked when it comes to appropriate osteoporosis management (Giangregorio, Papaioannou, Cranney, Zytaruk, & Adachi, 2006; Papaioannou et al., 2004).
Educating patients and healthcare providers about osteoporosis may play a pivotal role in improving osteoporosis management after fragility fracture. The 2000 National Institutes of Health Consensus Conference on Osteoporosis identified as one of its priorities “the need to study the most effective method of educating the public and healthcare professionals about the diagnosis and treatment of osteoporosis” (Consensus Development Panel, 2000). An environmental scan can be used to better understand the current knowledge and behavior and inform interventions aimed at changing behavior (Cook, Montori, McMullin, Finfer, & Rocker, 2004). Although osteoporosis knowledge in physicians and nurses has been assessed, few studies have investigated osteoporosis knowledge and information needs in healthcare providers who specifically treat patients with fragility fractures (Werner, 2005).
Fracture prevention and treatment requires a multi-disciplinary approach; a number of different types of healthcare professionals are involved not only in patient treatment but also in the education of patients and their caregivers. Nurses, physiotherapists, occupational therapists, pharmacists, nuclear medicine technicians, and dieticians are part of a multidisciplinary team that is involved in the diagnosis, treatment, and rehabilitation of fragility fracture patients. No research to date has explored osteoporosis knowledge and information needs in healthcare professionals who are directly involved in the management of patients with fragility fractures. Having an educated multidisciplinary team of front-line staff who understand osteoporosis and its management may provide additional opportunities for fragility fracture patients or other individuals at risk to be educated about osteoporosis management, which may ultimately result in improved treatment and adherence, and a reduction in fracture rates.
If educational materials about osteoporosis are to be developed, they should be tailored to the needs of the nurses and other healthcare professionals to improve the impact and effectiveness of the materials. Understanding current osteoporosis knowledge and the needs of health-care professionals with respect to osteoporosis knowledge would provide a framework for the development of educational interventions. Although levels of osteoporosis knowledge have been reported previously in nurses and nursing students, there was no assessment of learning needs and preferences (Berarducci, 2004; Berarducci, Lengacher, & Keller, 2002; Chen, Yu, Wang, Cheng, & Huang, 2005; Ziccardi, Sedlak, & Doheny, 2004). The purpose of this study was to evaluate osteoporosis knowledge and learning needs of a multidisciplinary group of nurses and other healthcare professionals who work in areas providing care for patients who often have osteoporosis and fractures, and to facilitate the development of a knowledge-transfer strategy designed with the ultimate goal of improving osteoporosis management after fracture.
Methods
Sample/Setting
The setting for the study was a large multisite hospital in Ontario, Canada. Healthcare providers were eligible for the study if they worked in areas that served patients with osteoporosis or fractures. This included staff from fracture clinics, orthopaedics and rehabilitation wards, and in nuclear medicine.
A convenience sample of all healthcare providers working in these areas was drawn between November 2005 and February 2006. Healthcare providers were invited to participate in the study by the local nurse clinician educator and via advertisement. They were informed that the study was a needs assessment to inform future educational interventions, and efforts were made to include staff on all shifts. All participants provided written informed consent prior to entering the study. The study was approved by the Research Ethics Board at Hamilton Health Sciences.
Instruments
Each participant completed a questionnaire with four components. The first component included a series of demographic questions and the second an assessment of osteoporosis knowledge using a modified version of the Osteoporosis Knowledge Questionnaire (OKQ) (Berarducci et al., 2002). The OKQ is a 22-item, multiple-choice questionnaire designed to assess knowledge of osteoporosis and associated preventative measures, and has been described previously (Berarducci et al.).
Although a number of questionnaires to test osteoporosis knowledge have been developed (Werner, 2005), the OKQ was chosen because it was designed to test osteoporosis knowledge in nurses; there are none that have been validated in a broader spectrum of healthcare providers. The questions in the OKQ address several osteoporosis-related topics; epidemiology, risk factors, disease manifestations, and prevention and treatment strategies. The OKQ has been demonstrated to have sufficient content validity (r = .95).
The original instrument was also modified in the following ways: (a) Question 1 was modified to reflect Canadian osteoporosis prevalence statistics; (b) a question was added to evaluate whether healthcare providers understood that patients with fractures were at risk of future fractures; (c) Question 20 was removed because exercise related to bone health was addressed in two other questions; and (d) a “Don’t Know” option was included in all OKQ quiz questions to reduce guessing.
The third component of the questionnaire included a series of questions about the sources of information they have used previously to learn about osteoporosis, their preferred sources of information, and what information they felt they needed to learn more about (see Table 1). The fourth component of the questionnaire was the Calcium Calculator, where participants had to indicate how many servings of each food on a list of calcium-containing foods they had eaten the day before. Sample portion sizes were provided. Calcium intake in milligrams (mg) was calculated based on the number of portions and the calcium content of each item.
Table 1.
Information Needs and Preferences Questions
| Question | Options Provided |
|---|---|
| Have you used any of the following to learn more about osteoporosis? | Yes/no to the following: pamphlets, patient-based cases, hospital newsletter, magazine or journal articles, websites, posters, mentorship, presentations at work, presentations offsite, other |
| If you decided you wanted to learn more about osteoporosis, what are the ways that you would most prefer to get that information? Please check only your top 3 preferred methods. | Top 3 of the following: pamphlets, patient-based cases, hospital newsletter, magazine or journal articles, websites, posters, mentorship, presentations at work, presentations offsite, other |
| We want to know what kinds of information you need. Below is a list of osteoporosis-related topics. Please check off if you feel you absolutely need more information about the topic, you might like to have more information about the topic, or if you don’t need more information about the topic. |
|
| If you had to choose the osteoporosis-related topic you would most like information about, what would it be? | Free text |
| Are there any other sources of information or resources that you think you need to care for osteoporosis patients properly? | Free text |
Analysis
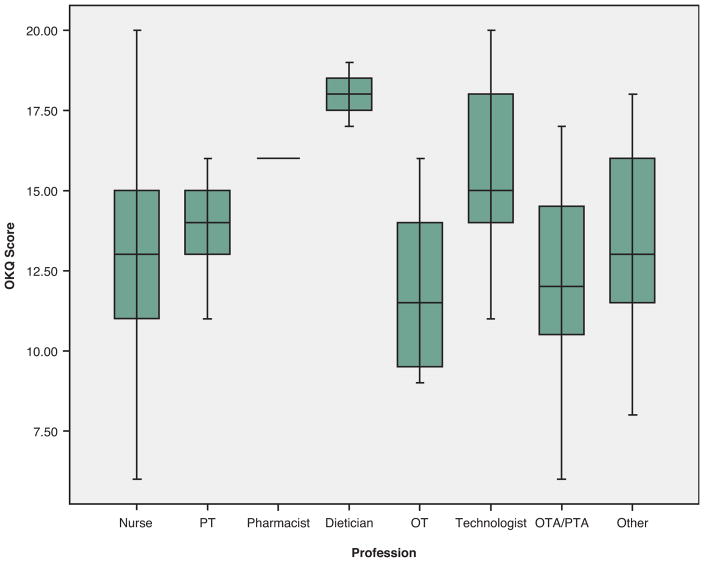
Demographic characteristics, scores on the osteoporosis knowledge test, and responses to osteoporosis information needs questions were summarized using descriptive summary measures: expressed as mean (standard deviation) for continuous variables; and number (percent) for categorical variables. The ranges of scores for individuals of each category of profession were depicted in a box and whisker plot (SPSS 14.0 for Windows).
Results
Participants
One hundred and twenty-nine individuals agreed to participate among a total of 179 staff (79% response rate). With the exception of the nuclear medicine staff, the majority of respondents were from fracture clinics and orthopaedic and rehabilitation units. Table 2 summarizes characteristics of the study population. The majority of participants were women (90%) and were full-time employees (71%). When asked to estimate what proportion of their patients had osteoporosis, most participants (73%) reported that at least 50% of their patients had osteoporosis, and 29% of participants reported that 75% of their patients were affected. A family history of osteoporosis or of hip fracture was reported in 40 and 14% of health professionals in the current study, respectively. The time taken to complete all the components was 20–30 min.
Table 2.
Characteristics of Study Participants
| Mean age (SD), range | 40.9 (10.2), 36–60 |
| Number of females (%) | 115 (90) |
| Occupation | |
| Nurse | 63 |
| Therapists (physiotherapist) | 11 |
| Nuclear medicine technologist | 12 |
| Ultrasound technologist | 2 |
| Pharmacist | 2 |
| Dietician | 3 |
| Dietetic assistant | 3 |
| Nursing/medical/OT students/clerks | 6 |
| Orthopaedic technologist | 2 |
| OT/PT assistants | 8 |
| Social workers | 3 |
| Speech language pathologist | 1 |
| Therapeutic recreation specialist | 1 |
| Clinician educator | 2 |
| Other | 2 |
| Average number of years as HCP (range) | 15.1 (0–40) |
| Highest level of education completed | |
| High school | 4 |
| College | 69 |
| University | 45 |
| Masters’ | 11 |
| Family history of osteoporosis (%) | 52 (40.3)a |
| Family history of hip fracture (%) | 18 (14.0)b |
| Diagnosis of osteoporosis (%) | 5 (3.9) |
| Mean daily milligram calcium (SD), range | 1,270 (711), 50–3,475 |
Therapist category = physical therapist and occupational therapist; HCP = healthcare provider; OKQ = Osteoporosis Knowledge Questionnaire.
Sixteen participants reported they did not know if they had a family history of osteoporosis.
Five participants reported they did not know if they had a family history of hip fracture.
Osteoporosis Knowledge
Out of a total possible score of 22, the mean (SD) score on the OKQ was 13.4 (3.0), and the scores ranged from 6 to 20. More than 90% of the participants were able to correctly identify the definition of osteoporosis, that stretching is not a weight-bearing exercise, that dairy products are the best available source of dietary calcium, and that treatments are available to prevent bone loss (see Table 3). More than 70% of the participants understood that fragility fractures are a risk factor for future fractures, loss of height may be an indicator of osteoporosis, bone densitometry is used to diagnose osteoporosis, prednisone increases osteoporosis risk, and recognized which exercises were weight bearing.
Table 3.
Participant Responses on Osteoporosis Knowledge Questionnaire (OKQ)
| Question (correct response bold) | Percent Correct | Percent Don’t Know |
|---|---|---|
What percentage of Canadian women over the age of 50 will develop osteoporosis?
|
8.5 | 37.2 |
2. Women begin to lose bone mass at what age?
|
38.0 | 9.3 |
3. Which of the following does not increase the risk of developing osteoporosis?
|
58.9 | 18.6 |
4. The most serious fracture caused by osteoporosis that can be life threatening is:
|
55.0 | 7.8 |
5. What is the recommended daily intake of calcium for women aged 40 to 49 who are still menstruating?
|
16.3 | 30.2 |
6. Food products (e.g., orange juice) fortified with calcium generally provide approximately how much calcium per serving:
|
10.1 | 60.5 |
7. Which of the following is considered the best preserver of bone mass in women?
|
31.0 | 22.5 |
8. Osteoporosis literally means:
|
92.2 | 2.3 |
9. Which of the following may be a sign of osteoporosis?
|
79.8 | 6.2 |
10. If you use sunscreen or avoid direct sun exposure, which of the following is the recommended amount of daily vitamin D intake needed to help absorb calcium?
|
52.7 | 38.8 |
11. Which of the following is NOT an example of weight-bearing exercise?
|
94.6 | 1.6 |
12. Which of the following medicines is used to treat osteoporosis?
|
58.9 | 29.5 |
13. Which of the following is the best source of dietary calcium?
|
92.2 | 2.3 |
14. Currently, the most widely accepted method to determine whether or not you have osteoporosis is:
|
86.8 | 5.4 |
15. It is best to take calcium supplements (pills):
|
50.4 | 27.9 |
16. Which of the following most accurately describes measures to prevent osteoporosis?
|
93.8 | 3.9 |
17. Taking certain medicines for long periods of time may increase your risk for developing osteoporosis. An example of such a medicine is:
|
72.9 | 23.3 |
18. Taking hormone replacement (estrogen) after menopause may:
|
69.8 | 14.0 |
19. Which of the following statements is NOT correct?
|
30.2 | 23.3 |
20. Once a woman begins to lose bone mass:
|
92.2 | 5.4 |
21. Which group of activities best describes weight-bearing exercise?
|
87.6 | 2.3 |
22. Which of the following is CORRECT?
|
72.9 | 13.2 |
There were a number of questions where more than 25% of the participants responded that they did not know the answer; the prevalence of osteoporosis, the recommended daily intake of calcium, the amount of calcium in fortified products, the recommended intake of vitamin D, the medications used to treat osteoporosis, and how best to take calcium (see Table 3). Only 38% of the respondents correctly identified that bone loss begins in the third decade. Question 7 asked what the best preserver of bone mass was in women; in the original questionnaire, the correct answer was estrogen, although it may be argued that bisphosphonates is also a valid response. However, only 31 and 5.4% of the respondents identified estrogen and bisphosphonates, respectively, as the best preserver of bone mass in women. The remaining respondents chose calcium (33.3%), vitamin D (7.8%), or “Don’t Know” (22.5%) as their response to Question 7.
According to the responses on the Calcium Calculator portion of the questionnaire, the mean (SD) daily calcium intake among healthcare providers surveyed was 1270 (711) mg, range 50–3,475 mg (see Table 2).
There was considerable variability among scores within profession categories, with the exception of dieticians and pharmacists, where there were only two and three of each, respectively. A box and whisker plot that portrays the range of scores across work groups is shown in Figure 1 (see Taking the Mystery out of Research for information on reading box and whisker plots).
Figure 1.
Scores on OKQ for each Profession Category
PT = physical therapist
OT = occupational therapist
Technologist includes nuclear medicine technologists (12), ultrasound technologists (2) and orthopedic technicians (2)
Taking the Mystery Out of Research. Box and Whisker Plots: Displaying Mean, Interquartile Range, and Range.
A challenge for researchers is to present their findings so that it will be useable and understandable to the reader. Often visual representations assist the reader in understanding the findings, especially when groups are being compared. A box and whisker plot is a useful visual representation when (a) large numbers of observations are measured on an interval scale (the distance between points on the scale are equal, such as test scores, temperatures), (b) when two or more groups being compared, and (c) when the scores are not normally distributed.
The box and whisker plot (also called a box plot) allows immediate visualization of the center and spread of the scores. The statistics presented include the median (center) and two measures of spread or variability, the interquartile range and the overall range of scores. The components of the box and whisker plot are illustrated below.
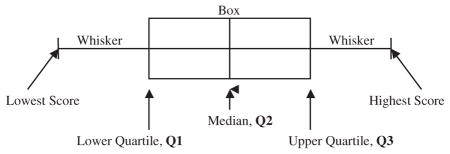
The median represents the midpoint or the center of the scores. In calculating a median, scores are arranged in order of magnitude, and the middle number is the median. It is marked by the vertical line inside the box. For an odd number of data elements or scores, the median is the middle number. For an even number of scores, the median is computed as the mean of the middle two numbers. Thus, for the scores of (70, 72, 78, 84, 86, 88, 90), the median score is 84. For the scores of (70, 72, 78, 84, 86, 88, 90, 92), the median is the mean of the middle two numbers, 88 and 86. So, in this case, the median is 87. In a box and whisker plot, the median is represented by the vertical line inside the box.
The interquartile range is a measure of spread or dispersion. It is the difference between the 75th percentile or the third quartile (called Q3) and the 25th percentile or first quartile (called Q1). The formula for the interquartile range is therefore Q3 – Q1. To calculate Q3, take the median of the upper half of the data. To calculate Q1, take the median of the lower half of the data. In a box and whisker plot, the ends of the box represent the lower and upper quartiles.
The range is a measure of dispersion and represents the difference between the lowest and highest scores in the data set. The range is calculated by subtracting the smallest score from the largest score. In a box and whisker plot, the whiskers are the two lines outside the box that extend to the highest and lowest data scores.
In the article by Giangregorio, a box plot (Figure 1) is used to visually display the osteoporosis knowledge findings for the different professional categories. This allows for a quick comparison of the median, interquartile range, and range for the different professional categories.
One can see from the box and whisker plot summarizing the osteoporosis data that the dieticians had the highest median score (18) followed by pharmacists, technologists, physical therapists, nurses, OTA/PTAs, and then OTs. By examining the position of the median score in the box, it can be seen that sometimes the median is in the center of the box (as with nursing), indicating equal dispersion of scores on either side of the median, or the median can be off-centered (as with technologists), indicating smaller variability in one of the quartiles. In examining the technologists group, the median score was 15. The second quartile scores had little variability all with scores of 14 or 15. The third quartile scores had greater variability with scores ranging from 15 to 18.
Looking at the representation of the dispersion findings, it can be seen that there was no variability in scores for the pharmacist group (median 16). Smaller dispersion was seen for the dietician group (interquartile range of 1 and total range of 2) and physical therapists (interquartile range from 13 to 15 (2) and total range from 11 to 16 (range of 5)). Nursing had the largest range from 6 to 20 (range of 14) with the interquartile range or 50% of scores between 11 and 15.
The box and whisker plot is an effective way to present the findings from this study and allows the reader to quickly compare the professional categories findings.
Osteoporosis Information Needs and Preferences
The proportion of participants reporting prior use of various sources of osteoporosis information are as follows: pamphlets (42.6%), patient-based cases (38.8%), hospital newsletter (10.1%), magazine or journal articles (69.0%), Web sites (30.2%), posters (30.2%), mentorship (6.2%), and presentations at work (45.0%), and presentations offsite (20.2%). When asked what ways they would most prefer to get information about osteoporosis, the sources most frequently cited were work presentations, magazine or journal articles, and pamphlets. The osteoporosis topics that participants cited most frequently as the topics they would most like information about were prevention, new research, and treatment-related information including benefits and risks of medications, nutrition/supplements. Thirty-one (11%) participants responded to a question asking what other information or resources they needed to care for patients; responses included requests for information or resources to give to patients regarding osteoporosis, requests for in-service education or presentations, and requests for more time per patient and additional educational tool and resources.
Discussion
The current study revealed that there are gaps in osteoporosis knowledge among nurses and other health professionals working with individuals who are at risk of osteoporotic fracture or have had a fracture. The major areas of knowledge deficit in this study were the topics related to health promotion and management of patients with osteoporosis. Large gaps were identified in the following areas: (a) the prevalence of osteoporosis; (b) the recommended daily intake of calcium; (c) how much calcium is usually in fortified products; (d) the recommended intake of vitamin D; (e) that bisphosphonates are used to treat osteoporosis; and (f) that calcium should be taken in divided doses with meals. In addition, many respondents did not know that bone loss begins in the third decade or that estrogen or bisphosphonates are the best preservers of bone mass in women. Most respondents knew the definition of osteoporosis, that treatment is available, that dairy products were the best source of calcium, and that stretching does not qualify as a weight-bearing exercise.
The average score on the OKQ (13.4) among this heterogeneous group of healthcare professionals was similar to the average scores reported previously among nurses and nursing students (Berarducci, 2004; Berarducci et al., 2002). However, the group surveyed for the current study was of healthcare professionals who specifically work with patients with fractures or those who are at risk of fractures, and one would expect that there would be fewer gaps in their osteoporosis knowledge. Consistent with the current study, previous studies investigating osteoporosis knowledge using the OKQ in nurses and nursing students demonstrated large gaps in nutrition-related items (i.e., recommended calcium intake, amount of calcium in fortified foods, how to take calcium supplements), physiology-related items (i.e., at what age bone loss begins, best preserver of bone in women), and osteoporosis prevalence (Berarducci; Berarducci et al.). Interestingly, 40% of the participants had a family history of osteoporosis and 14% had a family history of hip fracture; the gaps in participants’ osteoporosis knowledge may also have personal relevance.
In two recent studies exploring the educational needs of physicians in the management of osteoporosis, the importance of a prior fracture as a risk factor for future fractures was not well recognized by many family physicians (Jaglal, Carroll, et al., 2003; Jaglal, McIsaac, et al., 2003). Given that having a fracture is an independent risk factor for future fractures (Kanis et al., 2004), we added a question to the OKQ to determine if healthcare professionals knew that having a fragility fracture increased the risk of future fractures. More than 70% of the participants answered this question correctly, and they could recognize other clinical risk factors associated with osteoporosis (height loss, prednisone use). Although this is a relatively high percentage, it translates into about 30% of care providers in this study not understanding the risk of prior fragility fractures, which could place patients at risk in terms of handling and patient management.
In the current study, the pharmacists and the dieticians scored higher on the OKQ compared to the other professional categories (see Figure 1). Interestingly, the technologists’ median score on the OKQ was higher than that of the other professional categories with the exception of the pharmacists and the dieticians. The majority of the technologists were from nuclear medicine departments and regularly performed bone density scans; the higher scores may be due to frequent exposure to patients at risk of osteoporosis and fracture or their participants in osteoporosis-related accreditation programs. The relatively high levels of knowledge among nuclear medicine technologists is encouraging; however, many individuals who suffer fragility fracture do not get referred for bone density screening and therefore would not have an opportunity to be flagged for osteoporosis management at this point of contact (Giangregorio et al., 2006).
In examining the nursing score, it must be noted that we also did not distinguish between registered nurses and registered practical nurses when dividing staff into employment categories, which may explain the large variability in scores among this category. Based on the number of registered practical nurses working in the relevant areas, it is estimated that one third of the 63 nurses surveyed were registered practical nurses.
A number of participants requested patient-related resources, including educational information for patients on osteoporosis, and more time per patient, suggesting that nurses and other healthcare professionals would like to play a larger role in assisting with patient education. For patients to get the greatest value from education, the educator needs to have a high degree of familiarity with the subject matter (Gold & McClung, 2006). Perhaps an educational intervention developed for staff should be coupled with educational resources for the staff to provide for patients and to facilitate patient self-management.
The current study aimed to inform future interventions in nurses and other healthcare professionals working in the relevant hospital areas. Performing an environmental scan to understand the current knowledge and behavior is an essential step toward changing the behavior (Cook et al., 2004). The group of healthcare professionals surveyed reported previously using a number of sources for obtaining information about osteoporosis, with magazine or journal articles, presentations at work, and pamphlets cited by the largest percentage of respondents. Further, work presentations, magazine or journal articles, and pamphlets were reported to be the most preferred sources of information by the group surveyed. The topics that participants wanted more information about were consistent with the topics that were identified as gaps in osteoporosis knowledge, that is, prevention, new research, and treatment-related information including benefits and risks of medications, nutrition/supplements. Therefore, future interventions in this group should use a multifaceted approach to address the knowledge gaps identified in the current study. Previous interventions aimed at improving osteoporosis management have often been directed at physicians and/or patients (Cuddihy et al., 2004; Hawker, Rideout, Ricupero, Jaglal, & Bogoch, 2003; Majumdar et al., 2004), as historically the attending physician has been considered responsible for closing the care gap between fragility fractures and osteoporosis management. However, the adoption of knowledge translation models among all of the multidisciplinary healthcare team members may be more effective for closing the gap between evidence and practice when it comes to identifying and educating patients at risk of future fracture (Davis et al., 2003).
A few study limitations should be acknowledged. Although all nurses and other health professionals in the relevant hospital areas were invited to participate and multiple sessions were held over the study period to accommodate as many staff as possible, there were individuals that chose not to participate or were not able to participate at the times that the sessions were scheduled. It must also be emphasized that the outcome variable of interest in this study was knowledge of osteoporosis. Although knowledge is a requisite for behavior specific to health promotion and disease management, higher knowledge levels do not assure that health promotion and management behaviors of practitioners will be different.
In summary, healthcare professionals working with patients who are at risk of fracture are informed of osteoporosis risk factors and know that treatment options are available; however, there are noteworthy gaps in their osteoporosis knowledge that need to be addressed using a multifaceted approach. A multidisciplinary team that is well informed about osteoporosis and its management can play a role in the prevention of future fractures by recognizing the patients at risk and facilitating patient education and self-management.
Acknowledgments
This research was made possible by a grant-in-aid from the Fracture? Think Osteoporosis! Program–Hamilton Health Sciences and Merck Frosst. We would like to thank Ruth McCallum and Hamilton Health Sciences’ clinician educators for their help with this study, and all of the staff who participated.
Contributor Information
L. Giangregorio, Assistant Professor, Department of Kinesiology, University of Waterloo, Waterloo, Canada, Adjunct Scientist, Toronto Rehabilitation Institute, Toronto, Canada, and Adjunct Assistant Professor, McMaster University, Hamilton, Ontario.
Pauline Fisher, Clinical Nurse Specialist, Hamilton Health Sciences, Hamilton, Canada.
A. Papaioannou, Professor, Department of Medicine, Hamilton Health Sciences-McMaster University, Hamilton, Canada.
J. D. Adachi, Professor, Department of Medicine, St. Joseph’s Healthcare-McMaster University, Hamilton, Canada.
References
- Adachi JD, Ioannidis G, Berger C, Joseph L, Papaioannou A, Pickard L, et al. The influence of osteoporotic fractures on health-related quality of life in community-dwelling men and women across Canada. Osteoporosis International. 2001;12:903–908. doi: 10.1007/s001980170017. [DOI] [PubMed] [Google Scholar]
- Berarducci A. Senior nursing students’ knowledge of osteoporosis. Orthopaedic Nursing. 2004;23:121–127. doi: 10.1097/00006416-200403000-00009. [DOI] [PubMed] [Google Scholar]
- Berarducci A, Lengacher CA, Keller R. The impact of osteoporosis continuing education on nurses’ knowledge and attitudes. Journal of Continuing Education in Nursing. 2002;33:210–216. doi: 10.3928/0022-0124-20020901-06. [DOI] [PubMed] [Google Scholar]
- Brown JP, Josse RG. 2002 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. Canadian Medical Association Journal. 2002;167:S1–S34. [PMC free article] [PubMed] [Google Scholar]
- Chen IJ, Yu S, Wang TF, Cheng SP, Huang LH. Knowledge about osteoporosis and its related factors among public health nurses in Taiwan. Osteoporosis International. 2005;16:2142–2148. doi: 10.1007/s00198-005-2015-0. [DOI] [PubMed] [Google Scholar]
- Consensus Development Panel. National Institutes of Health Consensus Development Conference Statement: Osteoporosis prevention, diagnosis and therapy. Rockville, MD: National Institutes of Health; 2000. [Google Scholar]
- Cook DJ, Montori VM, McMullin JP, Finfer SR, Rocker GM. Improving patients’ safety locally: Changing clinician behaviour. Lancet. 2004;363:1224–1230. doi: 10.1016/S0140-6736(04)15955-2. [DOI] [PubMed] [Google Scholar]
- Cuddihy MT, Amadio PC, Gabriel SE, Pankratz VS, Kurland RL, Melton LJ., III A prospective clinical practice intervention to improve osteoporosis management following distal forearm fracture. Osteoporosis International. 2004;15(9):695–700. doi: 10.1007/s00198-004-1597-2. [DOI] [PubMed] [Google Scholar]
- Davis D, Evans M, Jadad A, Perrier L, Rath D, Ryan D, et al. The case for knowledge translation: Shortening the journey from evidence to effect. BMJ. 2003;327:33–35. doi: 10.1136/bmj.327.7405.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giangregorio L, Papaioannou A, Cranney A, Zytaruk N, Adachi JD. Fragility fractures and the osteoporosis care gap: An international phenomenon. Seminars in Arthritis and Rheumatism. 2006;35:293–305. doi: 10.1016/j.semarthrit.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Gold DT, McClung B. Approaches to patient education: Emphasizing the long-term value of compliance and persistence. American Journal of Medicine. 2006;119:S32–S37. doi: 10.1016/j.amjmed.2005.12.021. [DOI] [PubMed] [Google Scholar]
- Hawker G, Rideout R, Ricupero M, Jaglal S, Bogoch E. The impact of a simple fracture clinic intervention in improving the diagnosis and treatment of osteoporosis in fragility fracture patients. Osteoporosis International. 2003;14:171–178. doi: 10.1007/s00198-003-1377-4. [DOI] [PubMed] [Google Scholar]
- Jaglal SB, Carroll J, Hawker G, McIsaac WJ, Jaakkimainen L, Cadarette SM, et al. How are family physicians managing osteoporosis? Qualitative study of their experiences and educational needs. Canadian Family Physician. 2003;49:462–468. [PMC free article] [PubMed] [Google Scholar]
- Jaglal SB, McIsaac WJ, Hawker G, Carroll J, Jaakkimainen L, Cadarette SM, et al. Information needs in the management of osteoporosis in family practice: An illustration of the failure of the current guideline implementation process. Osteoporosis International. 2003;14:672–676. doi: 10.1007/s00198-003-1421-4. [DOI] [PubMed] [Google Scholar]
- Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35:375–382. doi: 10.1016/j.bone.2004.03.024. [DOI] [PubMed] [Google Scholar]
- Majumdar SR, Rowe BH, Folk D, Johnson JA, Holroyd BH, Morrish DW, et al. A controlled trial to increase detection and treatment of osteoporosis in older patients with a wrist fracture. Annals of Internal Medicine. 2004;141:366–373. doi: 10.7326/0003-4819-141-5-200409070-00011. [DOI] [PubMed] [Google Scholar]
- Papaioannou A, Giangregorio L, Kvern B, Boulos P, Ioannidis G, Adachi JD. The osteoporosis care gap in Canada. BMC Musculoskeletal Disorders. 2004;5:11. doi: 10.1186/1471-2474-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papaioannou A, Watts NB, Kendler DL, Yuen CK, Adachi JD, Ferko N. Diagnosis and management of vertebral fractures in elderly adults. American Journal of Medicine. 2002;113:220–228. doi: 10.1016/s0002-9343(02)01190-7. [DOI] [PubMed] [Google Scholar]
- Ray NF, Chan JK, Thamer M, Melton LJ. Medical expenditures for the treatment of osteoporotic fractures in the United States. Journal of Bone and Mineral Research. 1997;12:24–35. doi: 10.1359/jbmr.1997.12.1.24. [DOI] [PubMed] [Google Scholar]
- Werner P. Knowledge about osteoporosis: Assessment, correlates and outcomes. Osteoporosis International. 2005;16:115–127. doi: 10.1007/s00198-004-1750-y. [DOI] [PubMed] [Google Scholar]
- Wiktorowicz ME, Goeree R, Papaioannou A, Adachi JD, Papadimitropoulos E. Economic implications of hip fracture: Health service use, institutional care and cost in Canada. Osteoporosis International. 2001;12:271–278. doi: 10.1007/s001980170116. [DOI] [PubMed] [Google Scholar]
- Ziccardi SL, Sedlak CA, Doheny MO. Knowledge and health beliefs of osteoporosis in college nursing students. Orthopaedic Nursing. 2004;23:128–133. doi: 10.1097/00006416-200403000-00010. [DOI] [PubMed] [Google Scholar]