Abstract
Purpose
Obstructive sleep apnea is a prevalent sleep disorder among older adults. Oral appliances are increasingly prescribed as therapy for obstructive sleep apnea. Adherence to oral appliance therapy is highly variable. Based on value-expectancy theory and other social psychological theories, adherence to oral appliance therapy may be influenced by patients’ perceived effectiveness of the therapy, self-efficacy, and availability of social support. We examined these perceptions among older adults with obstructive sleep apnea who were prescribed oral appliance therapy.
Methods
We mailed surveys to all patients aged > 65 years who had been prescribed oral appliance therapy for obstructive sleep apnea over the prior 36 months at a Veterans Affairs medical center. We examined frequencies for items assessing perceived effectiveness, self-efficacy, and social support for nightly use of oral appliances from friends, family, or healthcare staff).
Findings
Thirty-nine individuals responded (response rate 30%; mean age 71 (+/− 6) years; 97% male). Thirty-six percent of the respondents perceived regular use of oral appliance therapy to be effective in managing obstructive sleep apnea; 39% agreed that they felt confident about using oral appliances regularly; 41% felt supported by people in their life in using oral appliance therapy; and 38% agreed healthcare staff will help them use their oral appliance regularly. This was despite our finding that more than half (65%) of patients believed they would use their oral appliance regularly.
Implications
Although oral appliance therapy is increasingly prescribed for obstructive sleep apnea, only about one-third of older adults perceive it to be an effective treatment, are confident about oral appliance use, or believe they will receive needed support. Future research is needed to better understand older adults’ perceptions so that interventions can be designed to improve the effectiveness of oral appliances, their self-efficacy for using oral appliances, and their social support for this therapy, which may, in turn, improve oral appliance therapy adherence.
Keywords: Sleep Apnea Syndromes, Patient Reported Measures, Oral Appliance Therapy, Attitude to Health
Introduction
Obstructive sleep apnea is prevalent among older adults.1 In a large multi-center study, approximately one-fifth of adults 65 years or older had sleep study findings consistent with obstructive sleep apnea.2 Oral appliances are increasingly prescribed as therapy for obstructive sleep apnea. The most common types of appliances are mandibular advancement devices and tongue retaining devices.3 Mandibular advancement devices treat sleep apnea by advancing the mandible forward to expand airway size.3 Custom fabricated mandibular advancement devices are manufactured in a laboratory according to dental impressions and the dentist prescriber’s requested advancement positions. These devices are titratable, allowing for small adjustments/advancements of the mandible. Prefabricated devices are made in large quantity without a specific patient in mind and subsequently, may be molded or shaped for a specific patient in a dental clinic setting. These prefabricated devices may also be titratable. Tongue retaining devices fit over the tongue and advance the tongue forward.3 Tongue advancement may be achieved through slight negative pressure in the lingual compartment of the device.4 Oral appliances are commonly used in lieu of a positive airway pressure device in the treatment of obstructive sleep apnea, particularly in patients unable to tolerate positive airway pressure due to symptoms such as claustrophobia or in patients who prefer a smaller medical device that does not require electricity.3
Although positive airway pressure therapy is considered first-line treatment for obstructive sleep apnea, oral appliance therapy may be considered for those unable to tolerate positive airway pressure therapy. A systematic review and meta-analysis of oral appliances for obstructive sleep apnea found that oral appliance therapy reduces the apnea-hypopnea index (AHI) by 7 events per hour compared to control appliances.5 Several studies have compared oral appliance and positive airway pressure therapy, and one meta-analysis of these studies found that although both therapies reduce the AHI significantly, positive airway pressure devices produce a larger reduction in AHI than oral appliances (25/hour versus 9/hour)68 Another meta-analysis found that positive airway pressure devices decrease the AHI by 6 events per hour and improve the oxygen nadir (lowest oxygen saturation value) by 2.9% compared to oral appliances.5 Oral appliance therapy may improve clinical outcomes such as blood pressure. A meta-analysis found that oral appliance therapy is associated with a 1.7 mm Hg decrease in diastolic blood pressure.7 Moreover, studies suggest that patients who use oral appliances are often satisfied with their therapy.8 These data support the use of oral appliances for those unable to tolerate positive airway pressure.
Similar to positive airway pressure therapy, patients who use oral appliances may experience side effects. Oral appliances may cause dry mouth, excessive salivation, discomfort, and malocclusion, which can be barriers to regular use of the oral appliances. Furthermore, because oral appliances for obstructive sleep apnea are removable, successful therapy requires patients to remember to reinsert the appliance nightly prior to going to sleep.33 Unfortunately, adherence to oral appliance therapy for obstructive sleep apnea is highly variable.9, 10
Consistent with value-expectancy theories of behavior (which posit the importance and perceived outcomes of specific behaviors effect choice, persistence, and performance11), adherence to oral appliance therapy is hypothesized to be more likely if patients perceive therapy to be effective, have social support from others (e.g., encouragement and assistance from friends, family, healthcare providers for adhering), and are confident that they can adhere.12 Although an increasing number of older patients are being diagnosed with obstructive sleep apnea and prescribed oral appliance therapy, studies examining older patients’ perceptions, self-efficacy, and social support for oral appliance therapy are lacking. These types of studies may be useful for informing development of behavioral interventions that increase acceptance and adherence to oral appliance therapy. We examined the perceptions of effectiveness, self-efficacy, and social support among older adults prescribed oral appliance therapy.
Patients and methods
Study Design, Sample, and Data Collection
Between April and June 2014, we mailed a survey to adults in the Los Angeles area who were 65 years or older who had been prescribed oral appliance therapy for obstructive sleep apnea over the prior 36 months from one Veterans Affairs medical center and who had a valid postal address (N=122). This Veterans Affairs medical center has a large sleep center that offers comprehensive therapy for obstructive sleep apnea, including positive airway pressure, oral appliances, and surgical interventions. Although the majority of patients with obstructive sleep apnea are initially treated with positive airway pressure therapy, some may begin oral appliance therapy as their initial therapy after discussion with a sleep physician about the risks and benefits of treatment options. For this study, eligible patients were identified through a review of durable medical equipment (Veterans Affairs Prosthetics) and dental clinic records to identify patients who were prescribed an oral appliance for sleep apnea. Postal address, date of birth, and gender were abstracted from the Veterans Affairs electronic health record. A $2 bill was included with the survey instrument mailed to these patients to encourage participation in the survey. The full study methods were approved by local institutional review boards (#2013-091198 and #13-001132).
Measures
Demographics
Age was calculated based upon date of birth obtained from the patient’s electronic health record, which also provided the patients’ gender. We collected information about race, ethnicity, and years of formal education on the survey. A question about length of use of the oral appliance (less than one year versus one year or longer) was included in the survey.
Health status
To characterize the overall health of the sample, we collected information on self-rated health,13 which is predictive of utilization and mortality,14, 15 as well as the presence of depressive symptoms and falls.16 (see Table 1)
Table 1.
Sample characteristics
| Continuous Variable | Mean (SD) |
|---|---|
| Age | 71.4 (6.3) |
| Categorical Variables | Frequency (%) |
| Education | |
| < 4 years college education | 19 (54) |
| > 4 years college education | 16 (46) |
| Gender | |
| Male | 32 (97) |
| Female | 1 (3) |
| Race/Ethnicity | |
| Asian | 1 (4) |
| Black | 3 (11) |
| Other | 1 (4) |
| Multiple | 2 (7) |
| White, Non-Hispanic | 20 (74) |
| Length of use of dental sleep appliance | |
| < 1 year | 17 (55) |
| > 1 year | 14 (45) |
| Self-Rated Health | |
| Excellent | 2 (6) |
| Very good | 4 (13) |
| Good | 13 (41) |
| Fair | 12 (38) |
| Poor | 1 (3) |
| Felt down, depressed, or hopeless in last 3 months | |
| Yes | 15 (44) |
| No | 19 (56) |
| Tripped or fallen in last 3 months | |
| Yes | 13 (64) |
| No | 23 (36) |
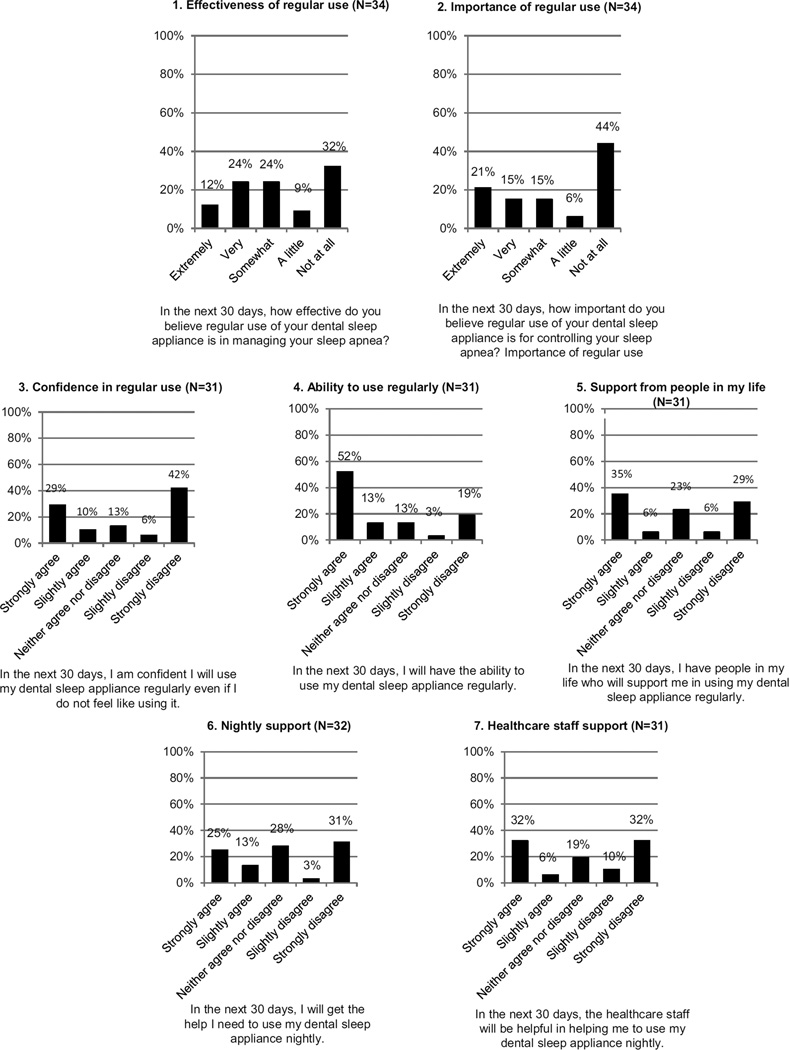
Measures of Oral Appliance Therapy Perceived Effectiveness, Self-Efficacy, and Support (see Figure 1)
Figure 1.
Descriptive results for the oral appliance survey items are shown in figure 1.
We adapted a subset of measures of perceived effectiveness (graphs 1 and 2 in Figure 1), self-efficacy (graphs 3 and 4 in Figure 1), and support (graphs 5, 6, and 7 in Figure 1) from a published questionnaire that was developed for individuals prescribed positive airway pressure therapy.17 Adaptations included replacing the term, “CPAP,” in each item stem used in the published questionnaire with the term, “dental sleep appliance.” We also made several formatting changes to make the questions and responses clearer for older veterans. For example, we provided five labeled response options for items 1 and 2 (i.e., extremely, very, somewhat, a little, and not at all) in place of the response options in the published questionnaire, which only labeled the extremes of the response scale (not at all important [or effective]=1 and extremely important [or effective]=5). Similarly, for items 3–7, we provided five labeled response options (strongly agree, slightly agree, neither agree nor disagree, slightly disagree, strongly disagree) in place of the response options provided in the published questionnaires, which labeled only the two extreme categories (disagree completely=1 and agree completely=5). In the instructions, we substituted the words, “30 days,” for the term, “month,” from the published questionnaire. We opted to included only a subset of items from the published questionnaire due to concern about participant burden. We also provided participants the opportunity to make open-ended comments.
Data Analysis
We examined frequency distributions for the survey items and types of sleep apnea therapy prescribed. Open-ended comments were reviewed and summarized. To assess for internal consistency reliability, we estimated Cronbach’s alpha for the 7-item scale assessing perceived effectiveness, self-efficacy, and nightly support.
We used Student’s t-test to examine differences in patient characteristics between survey responders and non-responders.
Results
A total of 39 individuals responded (response rate 30%) to the postal survey. The mean age was 71.4 (SD 6.3) years. Slightly more than half (54%) of responders reported having less than 4 years of college education. The majority of the sample was male (97%), and most responders were non-Hispanic white (74%). Fifty-five percent indicated use of their oral appliance therapy for less than one year.
More than half (65%) of participants agreed they would be able to use their oral appliance therapy regularly. In the domain of perceived effectiveness, 36% believed in the effectiveness of oral appliance therapy in managing or controlling their obstructive sleep apnea. In the domain of self-efficacy, 39% agreed with statements involving confidence in regular use of their oral appliance therapy. In the domain of social support, 38% agreed that they believed they would receive both nightly support and healthcare staff support, and 41% agreed that they believed they would receive necessary support from people in their life for using oral appliance therapy. (see Figure 1)
The internal consistency reliability for the 7-item scale (items listed in Figure 1) was 0.85, indicative of adequate reliability.18
Three participants provided comments. One participant commented that the process of getting fitted for an oral appliance was protracted because dental work was needed prior to fitting the oral appliance. This same participant noted a change in bite associated with the oral appliance and malfunctioning of the oral appliance due to a broken hinge. Another participant who had been prescribed a tongue retaining device commented that repeat testing showed that the device was ineffective. A third participant simply stated that he was unable to use the device.
There was no significant difference in age between survey non-responders and responders (p=.437). The non-responder and responder groups included one female per group.
Discussion
Although oral appliance therapy is increasingly prescribed for obstructive sleep apnea, two-thirds of older adults prescribed an oral appliance for obstructive sleep apnea did not perceive oral appliance therapy as effective, were not confident about oral appliance use, and/or did not believe they would receive needed support. This was despite our finding that more than half (65%) of patients believed they would use their oral appliance regularly.
Perceived effectiveness, self-efficacy, and social support for oral appliance therapy were low in this sample, with results indicating that older patients in our sample have low expectations for positive outcomes, have poor self-efficacy for overcoming barriers to use, and feel unsupported. These results are concerning since factors such as self-efficacy and social support are determinants of adherence to other types of sleep apnea therapies, such as positive airway pressure therapy.19, 20 Our results suggest that although oral appliance therapy may be an attractive alternative to positive airway pressure therapy because it is transportable and easy to use, many older patients prescribed oral appliance therapy may have unfavourable expectations and perspectives towards oral appliance therapy, which could negatively impact adherence. Whether younger, female, and non-veteran patients would have similar beliefs and expectations is unclear. Our sample, which was comprised of older, male veterans, had overall worse health, with nearly twice the percentage of survey participants reporting fair or poor health compared to only 17% of National Health and Nutrition Examination Survey respondents reporting fair or poor health.21 For example, other populations may not have the same low expectations for positive outcomes and may have more perceived support from their healthcare providers and family.
Our results indicate that perceptions of low effectiveness, poor self-efficacy, and lack of social support regarding oral appliance therapy are issues that should be addressed in the clinical setting, particularly when treating older, male veterans. Social Cognitive Theory suggests that behavioral and cognitive therapies provided in the clinical management of patients can lead to an appreciable improvement in adherence to prescribed therapies.17, 22 A systematic review of interventions to improve positive airway pressure adherence found improvement in outcomes when adherence was addressed through multiple approaches, including educational and psychosocial interventions.20 One study among positive airway pressure users found that a cognitive behavioral therapy intervention increased self-efficacy and social support as well as adherence to positive airway pressure therapy.23 Our findings suggest that sleep apnea patients prescribed oral appliance therapy could also benefit from cognitive behavioral therapy to improve adherence. Education about sleep apnea and the role of oral appliance therapy could improve outcome expectations and help patients identify ways to overcome barriers.12 Considering behavior change theory and identifying what stage of change a patient may be in when therapy is recommended could also help clinicians tailor more specific strategies, which may ultimately translate to higher levels of adherence.12
Our study has several limitations. First, the sample size was small, and the response rate was suboptimal. One of the possible reasons for the low response rate is that we mailed the survey instrument to patients instead of offering other modes such as online or telephone, and we only contacted each patient once. Multiple contacts with the patients may have improved the response rate. The individuals sampled were predominantly male, and all are veterans. We did not have information on many factors that potentially may influence beliefs about oral appliance therapy such as whether they had previously received educational information about oral appliance therapy.15 We did not have objective measurement of sleep apnea severity, AHI on oral appliance therapy, or adherence to oral appliance therapy in this sample. Although sensors that remotely and objectively monitor adherence to oral appliance therapy have recently been approved for use in the United States, this technology was not available at our facility during the survey period. Documentation of subjective number of hours of oral appliance use per night was very sparse, which prevented us from examining relationships between oral appliance therapy adherence and perceived effectiveness, self-efficacy, and social support. Finally, we had limited feedback from participants on ways we could improve the questionnaire for a future study.
Conclusions
Our study found unfavorable perceptions of the effectiveness of oral appliance therapy for sleep apnea, low levels of self-efficacy for oral appliance therapy, and poor social support for oral appliance therapy among older, predominantly male veterans. Future research involving larger samples that include both men and women of all ages and incorporate methods (e.g., sending the survey multiple times and using online and telephone modes of administering the survey) to increase response rates is needed to better understand patients’ perceptions of oral appliance therapy so that interventions can be developed to improve perceptions and increase social support for oral appliance therapy.
Acknowledgments
We thank Karl Kawakami, DDS, Michelle Zeidler, MD, MS, and Silverio Santiago, MD for enabling us to conduct the postal survey at the sleep center, Cindy Truong for abstracting and entering data, and Simone Vukelich for her assistance preparing the survey mailings.
Disclosures: This work was supported by the National Institute on Aging of the National Institutes of Health under Award Number [K23AG045937] and The Beeson Career Development in Aging Research Award Program (supported by NIA, AFAR, The John A. Hartford Foundation, and The Atlantic Philanthropies). Ron D. Hays received support from the University of California, Los Angeles (UCLA) and Charles Drew University (CDU), Resource Centers for Minority Aging Research Center for Health Improvement of Minority Elderly (RCMAR/CHIME) under NIH/NIA Grant P30-AG021684, and the UCLA/DREW Project EXPORT, NIMHD, [2P20MD000182]. Emily S. Patterson received support from the Institute Designed for Environments Aligned for Patient Safety (IDEA4PS) at The Ohio State University which is sponsored by the Agency for Healthcare Research & Quality [P30HS024379]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Department of Veterans Affairs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Institution where work was performed: All work was performed at VA Greater Los Angeles Healthcare System and David Geffen School of Medicine at UCLA
Conflicts of Interest: None
References
- 1.Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:136–143. doi: 10.1513/pats.200709-155MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Young T, Shahar E, Nieto FJ, et al. Predictors of sleep-disordered breathing in community-dwelling adults: the Sleep Heart Health Study. Arch Intern Med. 2002;162:893–900. doi: 10.1001/archinte.162.8.893. [DOI] [PubMed] [Google Scholar]
- 3.Ramar K, Dort LC, Katz SG, et al. Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015. J Clin Sleep Med. 2015;11:773–827. doi: 10.5664/jcsm.4858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lazard DS, Blumen M, Levy P, et al. The tongue-retaining device: efficacy and side effects in obstructive sleep apnea syndrome. J Clin Sleep Med. 2009;5:431–438. [PMC free article] [PubMed] [Google Scholar]
- 5.Okuno K, Sato K, Arisaka T, et al. The effect of oral appliances that advanced the mandible forward and limited mouth opening in patients with obstructive sleep apnea: a systematic review and meta-analysis of randomised controlled trials. J Oral Rehabil. 2014;41:542–554. doi: 10.1111/joor.12162. [DOI] [PubMed] [Google Scholar]
- 6.Sharples LD, Clutterbuck-James AL, Glover MJ, et al. Meta-analysis of randomised controlled trials of oral mandibular advancement devices and continuous positive airway pressure for obstructive sleep apnoea-hypopnoea. Sleep Med Rev. 2016;27:108–124. doi: 10.1016/j.smrv.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iftikhar IH, Hays ER, Iverson MA, Magalang UJ, Maas AK. Effect of oral appliances on blood pressure in obstructive sleep apnea: a systematic review and meta-analysis. J Clin Sleep Med. 2013;9:165–174. doi: 10.5664/jcsm.2420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Almeida FR, Mulgrew A, Ayas N, et al. Mandibular advancement splint as short-term alternative treatment in patients with obstructive sleep apnea already effectively treated with continuous positive airway pressure. J Clin Sleep Med. 2013;9:319–324. doi: 10.5664/jcsm.2576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bachour P, Bachour A, Kauppi P, Maasilta P, Makitie A, Palotie T. Oral appliance in sleep apnea treatment: respiratory and clinical effects and long-term adherence. Sleep Breath. 2016;20:805–812. doi: 10.1007/s11325-015-1301-0. [DOI] [PubMed] [Google Scholar]
- 10.Sutherland K, Vanderveken OM, Tsuda H, et al. Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med. 2014;10:215–227. doi: 10.5664/jcsm.3460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wigfield A, Eccles JS. Expectancy-Value Theory of Achievement Motivation. Contemp Educ Psychol. 2000;25:68–81. doi: 10.1006/ceps.1999.1015. [DOI] [PubMed] [Google Scholar]
- 12.National Cancer Institute. Thoery at a Glance - A Guide for Health Promotion Practice. 2nd. U.S. Dept of Health and Human Services, Public Health Service; 2005. [Google Scholar]
- 13.Ware J, Jr, Kosinski M, Gandek B. SF-36 Health Survey: Manual & Interpretation Guide. Lincoln, RI: QualityMetric Incorporated; 2000. [Google Scholar]
- 14.DeSalvo KB, Fan VS, McDonell MB, Fihn SD. Predicting mortality and healthcare utilization with a single question. Health Serv Res. 2005;40:1234–1246. doi: 10.1111/j.1475-6773.2005.00404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hays RD, Spritzer KL, Thompson WW, Cella D. U.S. General Population Estimate for "Excellent" to "Poor" Self-Rated Health Item. J Gen Intern Med. 2015;30:1511–1516. doi: 10.1007/s11606-015-3290-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kerse N, Boyd M, McLean C, Koziol-McLain J, Robb G. The BRIGHT tool. Age Ageing. 2008;37:553–588. doi: 10.1093/ageing/afn145. [DOI] [PubMed] [Google Scholar]
- 17.Stepnowsky CJ, Jr, Marler MR, Ancoli-Israel S. Determinants of nasal CPAP compliance. Sleep Med. 2002;3:239–247. doi: 10.1016/s1389-9457(01)00162-9. [DOI] [PubMed] [Google Scholar]
- 18.Nunnally JC. Psychometric theory. 2nd. New York: McGraw-Hill; 1978. [Google Scholar]
- 19.Dzierzewski JM, Wallace DM, Wohlgemuth WK. Adherence to Continuous Positive Airway Pressure in Existing Users: Self-Efficacy Enhances the Association between Continuous Positive Airway Pressure and Adherence. J Clin Sleep Med. 2016;12:169–176. doi: 10.5664/jcsm.5478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15:343–356. doi: 10.1016/j.smrv.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zajacova A, Dowd JB. Reliability of self-rated health in US adults. Am J Epidemiol. 2011;174:977–983. doi: 10.1093/aje/kwr204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stepnowsky CJ, Marler MR, Palau J, Annette BJ. Social-cognitive correlates of CPAP adherence in experienced users. Sleep Med. 2006;7:350–356. doi: 10.1016/j.sleep.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Richards D, Bartlett DJ, Wong K, Malouff J, Grunstein RR. Increased adherence to CPAP with a group cognitive behavioral treatment intervention: a randomized trial. Sleep. 2007;30:635–640. doi: 10.1093/sleep/30.5.635. [DOI] [PubMed] [Google Scholar]