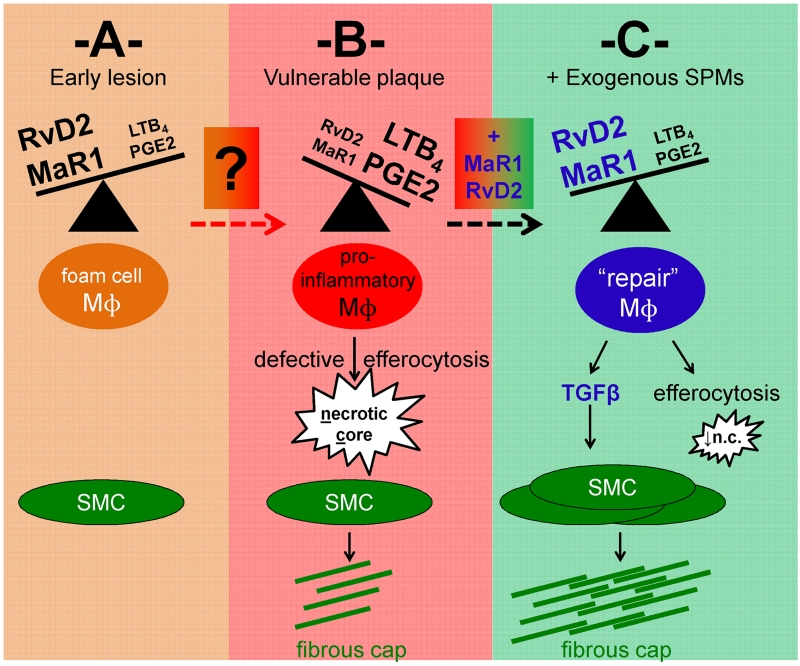
Figure 1. Resolving lipid mediators during atherosclerotic plaque progression.
Working model of the cellular consequences of altered ratios of pro-inflammatory vs. pro-resolving lipid mediators in early (A) versus advanced (B) atherosclerotic plaques. The factors that promote lipid mediator imbalance during the transition from (A) to (B) remain to be fully elucidated. In (B) reduced levels of lipid mediators resolvin D2 (RvD2) and maresin 1 (MaR1), and increased leukotriene LTB4 and prostaglandin PGE2, are associated with features of vulnerable plaques, including inflammatory macrophages, enlarged necrotic cores, and thin fibrous caps. (C) Predicted mechanistic basis of RvD2 and MaR1 therapy in advanced atherosclerosis, leading to macrophage reprogramming, reduced necrotic cores, and macrophage-TGFβ-mediated activation of SMCs. As noted in the commentary, a concurrent study to Viola et al., which showed similar results in mice and also humans [12], together with the results of previous studies showing the benefit of pro-resolving mediator therapy in atherosclerosis, are consistent with the overall principles depicted in this scheme. Mɸ = macrophage. SMC = smooth muscle cell.