Abstract
Background
To evaluate the efficacy of arthrodiastasis for Legg-Calve-Perthes disease.
Methods
Arthrodiastasis was conducted using external fixator devices (Orthofix) in 7 patients at least 8 years of age with a diagnosis of Legg-Calve-Perthes disease. The average follow-up was 80 months (range, 32 to 149 months), and their average age was 9.1 years (range, 8 to 12 years). The results of treatment were evaluated by measuring the degree of hip pain and the range of motion of the hip at 6 months after the operation and comparing the values with preoperative measurements. Radiological recovery was evaluated by the epiphyseal index and compared with the preoperative values. At the final follow-up, clinical and radiological results were evaluated using the Iowa hip score and the Stulberg classification.
Results
On the clinical evaluation performed at 6 months after arthrodiastasis, the degree of pain decreased by 1.8 points on average, and the average flexion, internal rotation, and abduction increased by 35°, 16°, and 11°, respectively. Based on radiological findings, the epiphyseal index showed a remarkable increase of 6.6 on average (from 19 preoperatively to 26 postoperatively). At the final follow-up, the average Iowa hip score improved from 65 points preoperatively to 84 points. There were 1 Stulberg class I hip, 2 Stulberg class II hips, 3 Stulberg class III hips, 1 Stulberg class IV hip, and no Stulberg class V hip.
Conclusions
We conclude that arthrodiastasis using an external fixator can be a relatively promising surgical procedure for the treatment of late-onset Legg-Calve-Perthes disease.
Keywords: Legg-Calve-Perthes disease, Arthrodiastasis, Epiphyseal index, Iowa hip score, Stulberg classification
Various treatment modalities have been introduced for the treatment of Legg-Calve-Perthes disease that is diagnosed based on clinical symptoms and abnormal radiological findings. However, definitive criteria for the treatment of the disease have not been established because accurate causes, pathogenesis, and pathology of the disease have not been completely elucidated. The prognosis and course of the disease are diverse and unpredictable, and it is likely to lead to degenerative arthritis in early adulthood.1) In particular, the prognosis is worse in patients older than 8 years of age, primarily because the remaining time for bone growth and reformation is relatively short and femoral head depression progresses further due to physical reasons such as reduced elasticity of the acetabulum.2,3)
Arthrodiastasis using an external fixator is a relatively novel treatment method for Legg-Calve-Perthes disease. It is considered to be useful because it maintains the mobility of the hip joint and a secures space for the femoral head in the joint while minimizing physical pressure and preserving synovial fluid circulation. The orthopedic department of Dong-A University Hospital analyzed the results of joint distraction conducted using external fixator in 7 patients with Legg-Calve-Perthes disease to evaluate the usefulness of arthrodiastasis.
METHODS
Arthrodiastasis was conducted using an external fixator in 7 patients at least 8 years of age who had been diagnosed with Legg-Calve-Perthes disease between November 1997 and May 2007. The patients had no history of previous treatment and were followed for at least 2 years (Table 1). The average follow-up was 80 months (range, 32 to 149 months), and their average age was 9.1 years (range, 8 to 12 years). The male to female ratio was 6:1. The exclusion criteria were bilateral presentation of the disease, combined lateral ossification, presence of sickle cell anemia or multiple epiphyseal dysplasia, and immunosuppression.
Table 1. Details of the Patients Treated by Arthrodiastasis.
| Case | Sex | Age at the on set of symptom (yr) | Classification | Duration of application (wk) | Length of follow-up (mo) | Adverse event | ||
|---|---|---|---|---|---|---|---|---|
| Waldenstrom | Catterall | Herring | ||||||
| 1 | Female | 10 | Fragmentation | IV | C | 12 | 33 | Loss to follow-up |
| 2 | Male | 8 | Avascular | III | B | 7 | 84 | Pin site infection |
| 3 | Male | 9 | Avascular | III | B | 6 | 149 | Pin site infection |
| 4 | Male | 12 | Fragmentation | IV | C | 30 | 61 | Distal femur fracture, left |
| 5 | Male | 9 | Fragmentation | IV | C | 7 | 87 | - |
| 6 | Female | 8 | Avascular | III | B | 16 | 114 | - |
| 7 | Male | 8 | Fragmentation | IV | C | 12 | 32 | Pin site infection |
Operative Technique
With the patient placed under general anesthesia, the arthrodiastasis procedure was performed using a shortened external fixation device (Orthofix, Bussolengo, Italy) under radiographic control. First, the pivot of the hip joint, which is the hinge area of the external fixation devices, was made by fixing a percutaneous guide-wire 5 mm distal to the center of the femoral head in 10° abduction of the hip joint under C-arm fluoroscopic guidance. Using a compression-distraction unit, the external fixator devices were mounted on the ilium and the femur, respectively, by fixing pins along the horizontal and axial planes to immediately expand the hip joint space from 0.5 cm to 1 cm until the distraction resulted in radiographic restoration of Shenton's line. The postoperative range of motion of the hip was maintained between 20° and 70° of flexion, partial weight bearing was allowed, and hip joint flexion and extension were recommended. The distractor was hand-tightened at intervals of 2 weeks and the pin sites were monitored for signs of infection. After the joint distraction procedure, the external fixation devices were maintained for 13 weeks (range, 6 to 30 weeks) on average.
For preoperative assessment, anteroposterior and frog-leg lateral radiographs of the pelvis were obtained. Radiographic severity of the disease was classified using the Waldenstrom classification, Catterall classification, and Herring lateral pillar classification.4,5) The epiphyseal index5) was used to assess the abnormal shape of the femoral epiphysis.
Treatment results were evaluated by measuring the degree of hip pain (0–3 points) and the range of motion of the hip at 6 months postoperatively and comparing with the preoperative values. Extent of recovery was evaluated up by comparing the preoperative and postoperative epiphyseal index. At the final follow-up by the time of skeletal maturity, clinical and radiological results were evaluated using the Iowa hip score and Stulberg classification.1)
RESULTS
In 3 patients, infection around the pins was observed, but all were recovered by wound dressing. One patient suffered a fracture in the distal femur on the operated side, which was treated with splinting. One patient could not be followed from the 33rd month after the operation (Table 1).
On the clinical evaluation performed at 6 months after arthrodiastasis, the degree of pain decreased from 2.6 points preoperatively to 0.8 points postoperatively on average. The range of flexion increased by 35° on average from 89° preoperatively to 124° postoperatively. The range of internal rotation increased by 16° on average from 15° preoperatively to 31° postoperatively and that of abduction increased by 11° on average from 24° preoperatively to 35° postoperatively.
Based on radiographic findings, three hips were Herring type B and 4 hips were Herring type C before the operation (Table 1). The epiphyseal index showed a remarkable increase of 6.57 (± 2.94) on average from 19 preoperatively to 26 postoperatively. At the final follow-up, the average Iowa hip score improved from 65 points preoperatively to 84 points postoperatively. There were 1 Stulberg class I hip, 2 Stulberg class II hips, 3 Stulberg class III hips, and 1 Stulberg class IV hip; there was no Stulberg class V hip.
Coxa plana and coxa magna were observed in 3 hips where additional shelf acetabuloplasty was performed to increase the covering of the femoral head. Overgrowth of the greater trochanter and shortening of the femoral neck were noted in 3 hips; a greater trochanter epiphysiodesis was performed in 1 hip and distal transposition of the greater trochanter was performed in the remaining 2 hips (Table 2). Patients in fragmentation stages and with wider ranges of invasion according to the Catterall and Herring classifications exhibited relatively worse results when assessed by the Stulberg classification. However, all the patients who were aged more than 8 years and presented with late-onset Legg-Calve-Perthes disease obtained sufficiently good treatment results classified as Catterall group III or IV or Herring grade B or C although the disease had been considered relatively difficult to treat in these patients.
Table 2. Radiologic Results of the Arthrodiastasis Group.
| Case | Epiphyseal index (initial) | Epiphyseal index (final) | Stulberg classification (final) | Additional procedure |
|---|---|---|---|---|
| 1 | 12 | 16 | III | - |
| 2 | 24 | 27 | II | Greater trochanter epiphysiodesis |
| 3 | 22 | 32 | II | Greater trochanter distal transposition |
| Shelf acetabuloplasty | ||||
| 4 | 20 | 28 | III | Cast for femur fracture |
| 5 | 20 | 24 | III | Shelf acetabuloplasty |
| 6 | 25 | 32 | I | - |
| 7 | 13 | 23 | IV | Greater trochanter distal transposition |
| Shelf acetabuloplasty |
Case 1
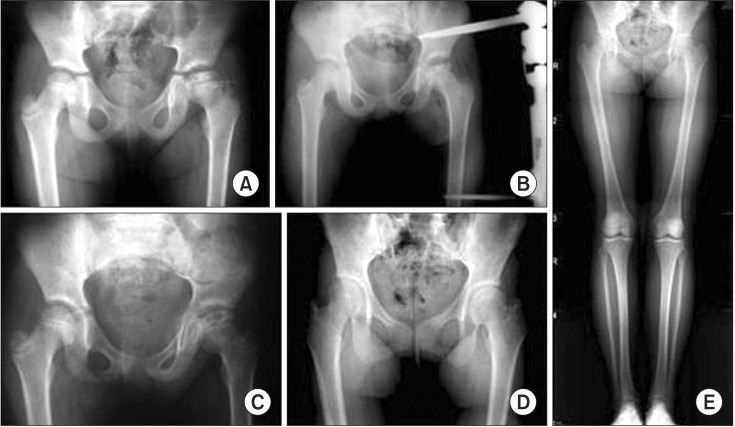
An 8-year-old female patient with Legg-Calve-Perthes disease of the left hip underwent arthrodiastasis using an external fixation device (case 6 in Tables 1 and 2). The external fixation device was maintained for 16 weeks. Her pain was relieved from 2 points preoperatively to 0 point at 6 months postoperatively. The range of motion increased by 30° for flexion, 10° for internal rotation, and 5° for abduction compared with the preoperative measurements. On the radiological evaluation, the epiphyseal index increased from 25 preoperatively to 32 postoperatively. The Iowa hip score improved from 70 points preoperatively to 88 points postoperatively. Thus, the hip was classified as Stulberg class I, showing a satisfactory treatment result without any additional operation (Fig. 1).
Fig. 1. (A) An 8-year-old girl shows left Legg-Calve-Perthes disease of Herring grade B on the radiograph. (B) Arthrodiastasis is performed. (C) Follow-up radiograph at 36 months after arthrodiastasis showing satisfactory femoral head regeneration. (D) Follow-up radiograph at 72 months after arthrodiastasis showing the reformed femoral head with congruency to the acetabulum. (E) Radiograph at the last follow-up (9 years) showing satisfactory results.
Case 2
A 9-year-old male patient with Legg-Calve-Perthes disease of the left hip had an external fixator for 6 weeks (case 3 in Tables 1 and 2). Hip pain was relieved from 2 points preoperatively to 1 point at 6 months postoperatively. The range of motion increased by 30° for flexion, 5° for internal rotation, and 5° for adduction compared with the preoperative measurements. At 25 months postoperatively, overgrowth of the greater trochanter and shortening of the femoral neck were observed in the hip; thus, a greater trochanter epiphysiodesis was performed. At 94 months postoperatively, a shelf acetabuloplasty was performed to increase the covering of the femoral head. On the radiological evaluation, the epiphyseal index increased from 22 to 32 at the final follow-up. The Iowa hip score improved from 65 points preoperatively to 80 points at the final follow-up. Thus, the hip was rated as Stulberg class II, showing a satisfactory treatment result (Fig. 2).
Fig. 2. (A) A 9-year-old boy shows right Legg-Calve-Perthes disease of Herring grade B on the radiograph. (B) Arthrodiastasis is performed. (C) Radiograph showing shortening of the femoral neck and relative overgrowth of the greater trochanter at 25 months after arthrodiastasis. (D) Greater trochanter distal transposition is done. (E) Shelf acetabuloplasty is performed for the coverage of femoral head at 94 months after arthrodiastasis. (F) Radiograph at the last follow-up (12 years) showing the reformed femoral head and the increased coverage of the femoral head with satisfactory clinical results.
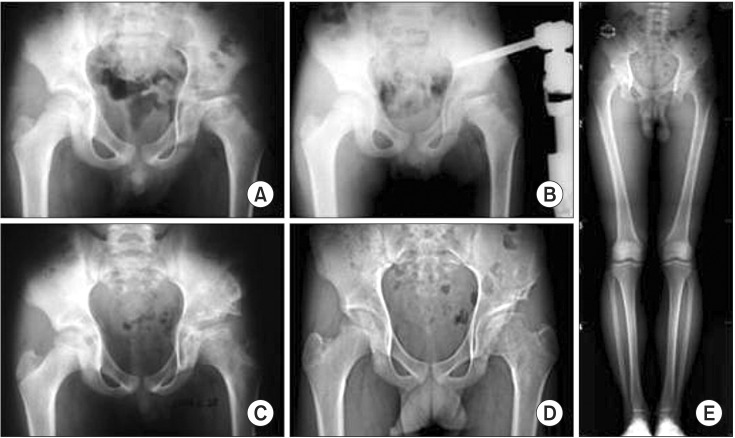
Case 3
A 9-year-old male patient with Legg-Calve-Perthes disease of the left hip wore an external fixator or 7 weeks (case 5 in Tables 1 and 2). Hip pain was relieved from 3 points preoperatively to 1 point at 6 months postoperatively. The range of motion increased by 40° for flexion, 20° for internal rotation, and 10° for adduction compared with the preoperative measurements. At 28 months postoperatively, a shelf acetabuloplasty was performed to increase the covering of the femoral head. On radiological evaluation, the epiphyseal index increased from 20 preoperatively to 24 at the final follow-up. The Iowa hip score improved from 63 points preoperatively to 72 points postoperatively. Thus, the hip was graded as Stulberg class III, showing a relatively satisfactory treatment result (Fig. 3).
Fig. 3. (A) A 9-year-old boy shows left Legg-Calve-Perthes disease of Herring grade C on the radiograph. (B) Arthrodiastasis is performed. (C) Shelf osteotomy is done for the coverage of the femoral head at 28 months after arthrodiastasis. (D) Radiograph at 72 months after arthrodiastasis showing the increased coverage of the ovoid femoral head. (E) Radiograph at the last follow-up (7 years) showing relatively satisfactory results.
DISCUSSION
Arthrodiastasis is a relatively new treatment method for Legg-Calve-Perthes disease, first reported in Verona in 1979 and has been used for osteoarthritis, chondrolysis, and avascular necrosis.6) This method maintains the mobility of the hip and secures a space for the femoral head in the joint while minimizing physical pressure and preserving synovial fluid circulation. Therefore, it is considered useful for Legg-Calve-Perthes disease and relatively good short-term follow-up results have been reported in several studies.7)
Kocaoglu et al.8) performed joint distraction using an Ilizarov external fixator on 11 patients with an average age of 7.5 years. Of the 11 hips, 7 were classified as Herring type C, and 8 hips were rated as Stulberg classification III or IV at the final follow-up. The method attracted much attention because it accelerated recovery of the hip in Legg-Calve-Perthes disease. In spite of this, the method has not been generally accepted because of the relatively high incidence of complications following the treatment such as infections around the pins. A group in Brazil prospectively studied 36 patients with Legg-Calve-Perthes disease9): 18 patients were treated by proximal femoral varus osteotomy and the other patients were treated by arthrodiastasis using external fixation devices. Indications were the same in both groups: pain in the hip joint in the stage of necrosis or fragmentation and Catterall group III or IV with at least 2 head-at-risk signs. Although regeneration of the femoral head occurred much earlier in the arthrodiastasis group, the results were satisfactory in both groups. Kucukkaya et al.10) performed arthrodiastasis on 11 patients and all the patients were classified into Catterall group III or IV or Herring grade B or C. The authors reported that recovery was much faster with arthrodiastasis, but recommended the treatment should be performed before destruction of the femoral head due to the limited possibility of regaining the height of the epiphysis through reformation of the regenerated bone in patients more than 8 years of age at the time of onset of the disease.
In this study, arthrodiastasis using external fixation devices were performed on 7 patients in whom the onset of symptoms occurred after 8 years of age. All patients were evaluated for pain and range of motion at 6 months after the operation. Radiological changes were compared and analyzed at the final follow-up. Satisfactory results were obtained with respect to pain and range of motion based on the clinical evaluation. The epiphyseal index at the final follow-up increased by 6.57 on average, indicating remarkable recovery. Patients in fragmentation stages and greater extent of invasion based on the Catterall and Herring classifications obtained relatively worse results according to the Stulberg classification. However, sufficiently good treatment results were achieved even in patients classified as Catterall group III or IV or Herring grade B or C despite the fact that the disease is difficult to treat disease when develops after 8 years of age. One of the most impressive findings of this study is that arthrodiastasis applied in the early stage of the disease before any significant collapse of the femoral head (Catterall group IV or Herring grade C) would prevent further fragmentation and accelerate the recovery process with ease. Therefore, benefits that can be expected from the joint distraction procedure include recovery of the height of the destroyed epiphysis, prevention of additional destruction of the femoral head, containment of the femoral head in the acetabulum, and fast recovery and reformation of the femoral head.
Daly et al.11) reviewed the results of shelf acetabuloplasty in 26 patients with early Legg-Calve-Perthes disease in the stage of reossification. Their age at the onset of symptoms was over 8 years. Most of the patients were classified as Catterall group III or IV. In the study, the authors concluded that the procedure could provide better long-term outcomes than femoral or pelvic osteotomy. In the current study, 3 patients showed findings of coxa plana or coxa magna after arthrodiastasis and thus shelf acetabuloplasty was performed to increase the covering of the femoral head. These patients showed satisfactory results at the final follow-up; thus, shelf acetabuloplasty can be considered a useful treatment method for sequelae after the recovery stage of Legg-Calve-Perthes disease.
This study was limited by its retrospective design and lack of a control group. Other limitation include that the number of patients was small and variables were inconsistent except for age. Conducting research on Legg-Calve-Perthes disease is challenging due to diverse characteristics of the disease and confusingly various classification systems and prognosis predictors. In addition, it is not easy to determine the optimal treatment modality since reported clinical results are based on a small number of subjects rarely involving a control group and subjects in previous studies have inconsistent characteristics with regard to age and progression of the disease. Thus, treatment results of Legg-Calve-Perthes disease are unsatisfactory in general. Many studies are being conducted in an effort to explore effective treatment modalities. The purpose of this study was to elucidate whether arthrodiastasis would provide better long-term results in older children with Legg-Calve-Perthes disease. Although we did not have much experience with the procedure, a long-term follow-up was not carried out, and statistical analyses could not be performed due to the small study population and inconsistent follow-up period, the results of this study suggest a considerable potential of arthrodiastasis as a treatment of Legg-Calve-Perthes disease. Furthermore, considering that the procedure allows for early joint mobilization and helps the recovery of the spherical shape of the depressed femoral head, encouraging results may be obtained even in patients with advanced Legg-Calve-Perthes disease.
In conclusions, arthrodiastasis using external fixation devices can be considered an effective treatment method in patients presenting with depression and deformation of the femoral head resulting from late-onset Legg-Calve-Perthes disease. It would be desirable to confirm our results in further research involving a greater number of cases and longer follow-up.
ACKNOWLEDGEMENTS
The authors thank Dong-A University and Dong-A University Hospital for the research funds for this clinical study. The article was presented at the 15th triennial congress of the Asia Pacific Orthopaedic Association in Seoul, Korea in 2007.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calve-Perthes disease. J Bone Joint Surg Am. 1981;63(7):1095–1108. [PubMed] [Google Scholar]
- 2.Bellyei A, Mike G. Acetabular development in Legg-Calve-Perthes disease. Orthopedics. 1988;11(3):407–411. doi: 10.3928/0147-7447-19880301-05. [DOI] [PubMed] [Google Scholar]
- 3.Mazda K, Pennecot GF, Zeller R, Taussig G. Perthes' disease after the age of twelve years: role of the remaining growth. J Bone Joint Surg Br. 1999;81(4):696–698. doi: 10.1302/0301-620x.81b4.9626. [DOI] [PubMed] [Google Scholar]
- 4.Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part I: classification of radiographs with use of the modified lateral pillar and Stulberg classifications. J Bone Joint Surg Am. 2004;86(10):2103–2120. [PubMed] [Google Scholar]
- 5.Heyman CH, Herndon CH. Legg-Perthes disease: a method for the measurement of the roentgenographic result. J Bone Joint Surg Am. 1950;32(4):767–778. [PubMed] [Google Scholar]
- 6.Aldegheri R, Trivella G, Saleh M. Articulated distraction of the hip. In: De Bastiani G, Apley AG, Goldberg A, editors. Orthofix external fixation in trauma and orthopaedics. London: Springer Verlag; 2000. pp. 605–612. [Google Scholar]
- 7.Aldegheri R, Trivella G, Saleh M. Articulated distraction of the hip: conservative surgery for arthritis in young patients. Clin Orthop Relat Res. 1994;(301):94–101. [PubMed] [Google Scholar]
- 8.Kocaoglu M, Kilicoglu OI, Goksan SB, Cakmak M. Ilizarov fixator for treatment of Legg-Calve-Perthes disease. J Pediatr Orthop B. 1999;8(4):276–281. [PubMed] [Google Scholar]
- 9.Guamiero R, Luzo CA, Montenegro NB, Godoy RM. Legg-Calve-Perthes disease: a comparative study between two types of treatment: femoral varus osteotomy and arthrochondrodiastasis with external fixation; 25th European Paediatric Ophthalmological Society (EPOS); 2000; Milan, Italy. [Google Scholar]
- 10.Kucukkaya M, Kabukcuoglu Y, Ozturk I, Kuzgun U. Avascular necrosis of the femoral head in childhood: the results of treatment with articulated distraction method. J Pediatr Orthop. 2000;20(6):722–728. doi: 10.1097/00004694-200011000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Daly K, Bruce C, Catterall A. Lateral shelf acetabuloplasty in Perthes' disease: a review of the end of growth. J Bone Joint Surg Br. 1999;81(3):380–384. doi: 10.1302/0301-620x.81b3.9405. [DOI] [PubMed] [Google Scholar]