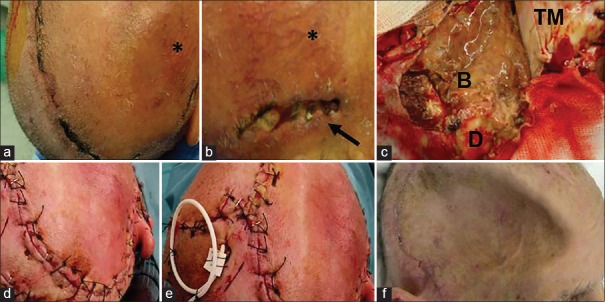
Figure 2.
(a and b) 54-year-old male previously treated by the right hemispheric decompressive craniectomy for severe head trauma. Twenty-one days after surgery the flap appeared swollen, showing a reticular pattern of small vessels surrounding the area of dehiscence (black asterisk). A 3 cm long, 1 cm large dehiscence was observed along the temporal line (black arrow). (c) At flap re-opening, after lifting the temporalis muscle (TM), a purulent collection involving the brain was immediately evident (B), with partial resorption of the overlying dural membrane (D). (d) Flap re-suturing was then easily obtained. (e) Intraoperative positioning of a contralateral external ventricular shunt was needed to reduce flap tension allowing uncomplicated re-suturing. (f) One month after revision a sinking flap syndrome developed. Nonetheless, full healing of the skin flap was evident