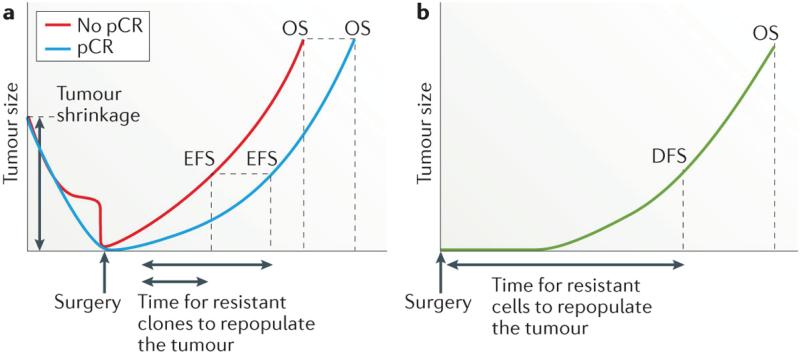
Figure 3. The influence of therapeutic response on survival.
a | In the neoadjuvant setting, achievement of a pathological complete response (pCR) is hypothesized to result in prolonged both event-free survival (EFS) and overall survival (OS), compared with an incomplete response, because fewer drug-resistant clones are present and, therefore, even fewer are likely to be left behind after completion of surgery and systemic treatments; thus repopulation of the tumour and/or the development of clinically detectable metastases is delayed or might never happen, and OS is prolonged in the population of patients with a pCR. The early benefit on EFS associated with achieving a pCR to neoadjuvant therapy, compared with an incomplete response, might be diminished in the long-term, however, as resistant clones repopulate the tumour and eventually lead to clinical disease recurrence and, in some cases, death; that is, attaining a pCR might improve OS, but the proportion of patients who are cured might not be significantly different. b | In the adjuvant setting, the time taken for any residual resistant cells to repopulate the tumour is reflected in the duration of disease-free survival (DFS) and OS. In all scenarios, the probability of pre-existing resistance, and thus the chance of residual cells being left after all treatment is completed, increases with tumour size at diagnosis and might be at least partially related to the breast cancer subtype. It should be noted, for example, that triple-negative breast cancers tend to be larger and to have more-rapid growth than other breast cancer subtypes;116 therefore, the risk of relapse might be higher, and the time to relapse shorter, for this subtype compared with others. Ultimately, the benefit of complete tumour shrinkage in patients with a pCR, in comparison with the outcomes of patients who receive only adjuvant therapy, might be minimal — assuming that almost all tumour cells are removed when R0 resection is achieved and that, in the adjuvant setting, the small number of residual cells are less likely to be treatment resistant.