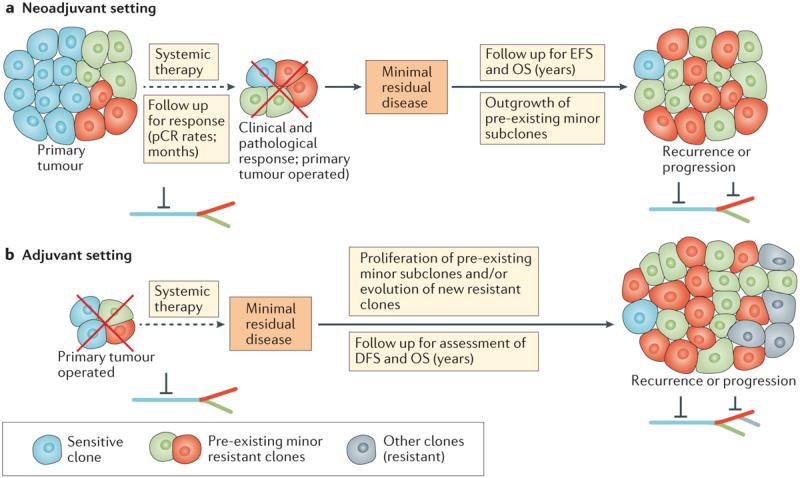
Figure 4. Tumour heterogeneity and drug resistance in the neoadjuvant and adjuvant breast cancer settings.
a | The efficacy of neoadjuvant treatment targeting ‘trunk’ (clonal) mutations or aberrations that are expressed by most or all of the tumour cells might nevertheless be limited by the overgrowth of spatially distinct distributed subclones with intrinsic resistance mechanisms (green and red cells), leading to primary drug resistance. This outgrowth of resistant subclones might underlie incomplete responses, or eventual relapse in those with a complete response. b | In the course of adjuvant therapy, the treatment duration and follow-up time are longer, creating a niche for the development of secondary (acquired) resistance to therapy, and/or outgrowth of pre-existing minor resistant subclones that were left behind after surgery and could persist despite systemic therapy. Contemporary data suggest, however, that the latter process is likely to predominate — most resist clones that underlie recurrence are detectable prior to treatment and, therefore, eventual acquired resistance is probably a consequence of low-level intrinsic resistance. The trunk–branch model for tumour heterogeneity is shown: the trunk of the tree bears ubiquitous genomic alterations; acquired subclonal mutations that are present only in a subset of the tumour cells compose the branches. Red inhibitory symbols represent pharmacological blockade. DFS, disease-free survival; EFS, event-free survival; OS, overall survival; pCR, pathological complete response