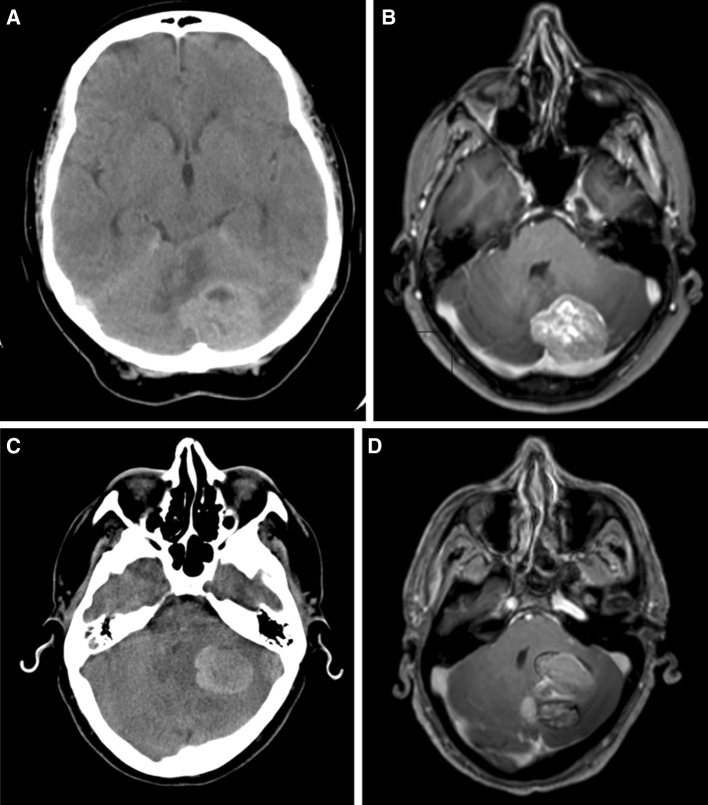
Fig. 1.
Illustrative cases. Case 1 images (a) and (b) 54 year old female. PMH Breast cancer (Her2 positive) Treated with mastectomy 1 year ago plus adjuvant chemotherapy (trastuzumab). Presented with 2 weeks of headaches and unsteadiness. CT brain revealed (a) large solid left cerebellar tumour, confirmed on MRI (b). KPS 90 pre-operatively. CT staging pre-op showed local lymph node involvement but no other metastatic disease. Underwent craniotomy and gross total resection with adjuvant WBRT and further systemic chemotherapy. Re-presented with similar symptoms 21 months later and MRI showed recurrent tumour at the same site. CT staging showed no evidence of extracranial disease. Further craniotomy and gross total resection performed. No further adjuvant therapy given. Gradual deterioration 10 months after second surgery and died 36 months after initial diagnosis. Case 2 images (c) and (d) 67 year old male. PMH Testicular cancer - orchidectomy 12 years ago. Presented with increasing confusion, headache, unsteadiness and falls. Acute deterioration the previous day. KPS 50 on arrival. CT head revealed 36 × 25 mm left cerebellar haemorrhagic tumour with triventricular hydrocephalus (c). Transferred to regional neurosurgical unit and external ventricular drain (EVD) inserted. MRI confirmed solitary bulky left cerebellar (d). Gross total resection performed later that admission, histology revealed metastatic carcinoma. Post- operatively the patient developed bulbar dysfunction and swallowing difficulty. Staging CT performed post-operatively revealed metastatic lung cancer with mediastinal and liver metastases. EVD reinserted due to post-operative hydrocephalus. 5 days of palliative WBRT administered as an inpatient. Continued deterioration and the patient died in hospital 5 weeks after surgery