Neglected or chronic ruptures of the patellar tendon are defined as ruptures presenting after 6 weeks. Late presentation is often due to neglect or missed diagnosis.1,12 With chronic ruptures, the patient presents with weakness, instability, and pain. Management of patients with chronic ruptures is difficult due to adhesions, proximal patellar migration, contracture, and quadriceps muscle atrophy.29 Before reconstruction of the patellar tendon (using autografts, allografts, or synthetic materials), the position of the patella must be normalized. Several methods had been reported to relocate the proximally migrated patella distally to its anatomic location, including preoperative traction, intraoperative traction, quadricepsplasty, and external fixation.8,15,17,20,27,30,31,33 The aim of this case report was to present the use of ring and wire external fixation applying the lengthening principles of Ilizarov13 to mobilize the proximally migrated patella distally as a successful treatment of chronic neglected patellar tendon rupture followed by second-stage patellar tendon reconstruction using an allograft. We report our experience in 2 cases, with an improved modification of the external fixator construct used for distal patellar transport in case 2. This report of 2 cases was approved by the Hospital for Special Surgery Institution Review Board.
Case 1
A 44-year-old man presented to the office of the senior authors (S.H.C., S.R.R.) with bilateral posttraumatic chronic patellar tendon ruptures and proximal migration of the patellae. The patient was involved in a severe jet-ski accident in which he sustained this bilateral injury and ruptured his spleen and was on a ventilator due to a brain injury for almost 1 year. Because of the severity of his other injuries, the patellar tendon ruptures were not initially diagnosed. After being weaned from the ventilator, it was noted that he had bilateral extensor lag, with both patellae migrated proximally into the midthigh region. He was in a rehabilitation facility since he came off the ventilator. The patient presented in a wheelchair with a chief complaint of inability to walk accompanied by bilateral anterior knee pain. The patient presented to the sports medicine service 3 years after the injury.
The patient, who was not able to stand, had full painless range of motion (ROM) of both hips. The knee ROM on both sides was from 15° to 110° of flexion, and there were severe extensor lags of both knees of 25°. Both patellae were migrated proximally at the junction of the proximal two-thirds and distal one-third of the thigh. Bilateral thigh atrophy with significant scarring of the quadriceps mechanism was noted. The patient could not extend either knee actively against gravity. Sensory examination was normal bilaterally, and the vascular examination was also normal.
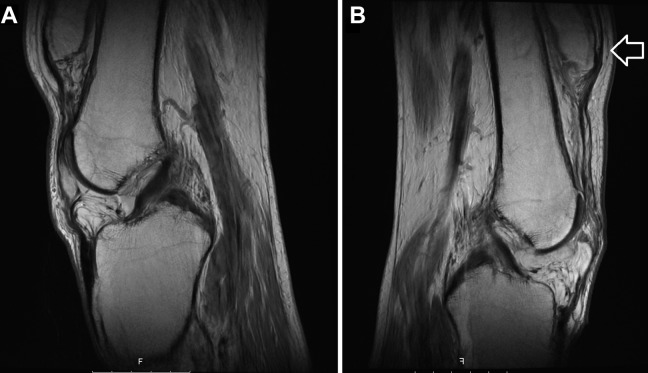
Radiographs of both knees revealed a 9-cm proximal migration of the left patella and 6-cm migration of the right patella, measured from the distal pole of the patella to the Blumensaat line. The Insall-Salvati ratio was 2.2 and 2 on the left and right sides, respectively. Magnetic resonance imaging (MRI) of both knees revealed bilateral severe patellar tendon insufficiency (Figure 1). Moderate quadriceps fatty atrophy (Goutallier grade 2) was noted on MRI bilaterally.
Figure 1.
Preoperative sagittal magnetic resonance image of the (A) right and (B) left knees showing proximal displacement of the patella (arrow).
The patient underwent staged operative correction. Stage 1 involved gradual bilateral distal transport and mobilization of the proximally migrated patellae using the Ilizarov/external fixation principles. The frames were removed bilaterally after 12 weeks once the patellae were in a satisfactory position. This was followed 1 day later by second-stage surgery with bilateral patellar tendon allograft reconstruction using patellar tendon allograft.
Technique
A 2-ring circular external fixator frame was used (Figure 2). The proximal ring was a 180-mm two-thirds ring fixed to the femur using two 6-mm half pins. The distal ring was a 155-mm half ring fixed to the patella using 2 tension wires placed within the patella from lateral to medial with an angle spread of about 20°. Three distraction rods were then placed between the femoral and patellar rings, with hinges adjacent to the patella half ring. Postoperatively, the patient was allowed weightbearing as tolerated and knee ROM exercises. The adjustments were started on the first postoperative day, with a target of 1.5-mm distraction per day divided into 3 adjustments. The patient was followed up every 2 weeks with radiographs of both knees to follow the progression of distal transfer of the patella. The target was to pull the right patella distally 6 cm and the left 9 cm. We used the Insall-Salvati ratio14 for assessment of patellar height to follow the progression of distal patellar transport, and the goal was to achieve a ratio of 1.
Figure 2.

Intraoperative view showing bilateral Ilizarov frame application. Note the distal ring holding the patella will be pushed distally (arrow), transporting the patella to the outlined circle.
Complications
Minor obstacles during the distraction period included canting of the ring causing superficial abrasion from contact between the proximal ring and the skin; this was managed by repositioning the ring. The patient was admitted to the hospital for a resistant pin tract infection and cellulitis during the distraction phase, and the infection completely resolved with intravenous vancomycin for 2 weeks followed by oral trimethoprim/sulfamethoxazole (TMP/SMX) for 4 weeks.
The distraction proceeded well with the right as well as the left patellae, with the need to speed the rate of distraction on the left side at some point to 3 mm per day where the patella was more proximally migrated and to make up for having to stop the distraction for almost 2 weeks until resolution of the pin tract infection. The correction was achieved after 2 months on the right side and after 3 months on the left side. Once the patellae were in a satisfactory position bilaterally (Figure 3), the decision was made to remove the frames after 3 months and proceed with open bilateral patellar tendon reconstruction (Figure 4). This was done using patellar tendon allograft, and fixation of the tibial tubercle allograft bone plug into a trough in the proximal tibia was accomplished using 4.5-mm cortical screws bilaterally. Proximally, the allograft tendon was secured to the quadriceps tendon using 5.0 Ethibond sutures (Ethicon). Postoperatively, ROM was initiated on the first postoperative day starting at 0° to 40°, progressing to 60° at 2 weeks, and increased gradually to 90° by 4 weeks. The patient was allowed partial weightbearing with crutches and a hinged knee brace set at 0° to 50° for 6 weeks, then continued using the brace for walking for another 4 weeks until regaining quadriceps strength. The patient was followed monthly, and bony healing of the tibial tubercle allograft to the proximal tibia was achieved by 16 weeks. The patient underwent physical therapy postoperatively, was able to gradually achieve full extension and 100° flexion bilaterally, and was able to stand and walk again. Over the course of 2 years, the patient developed progressive scarring of the quadriceps tendon on the left side and had an extensor lag of 25°. He was operated upon successfully with open quadricepsplasty and was able to again achieve full extension. The final ROM was full extension to 100° flexion bilaterally. The quadriceps strength was 5 out of 5 bilaterally, and no functional outcome scores were obtained pre- or postoperatively. The patient died of medical problems unrelated to his orthopaedic condition. We were not able to obtain a letter of consent.
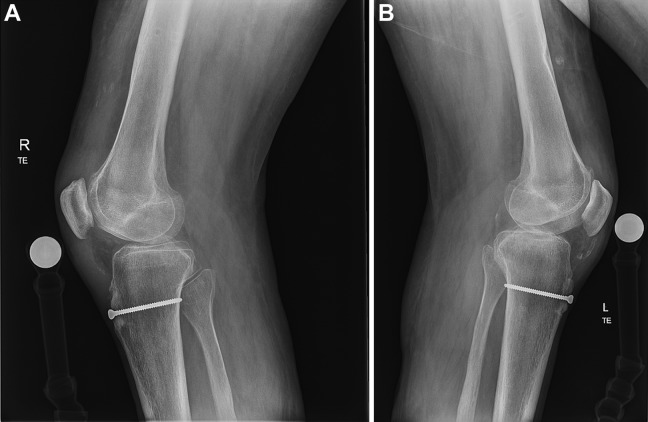
Figure 3.
Postoperative plain lateral radiographs at the end of distraction showing improved patellar height of the (A) right and (B) left knees.
Figure 4.
Postoperative radiograph after allograft patellar tendon reconstruction of the (A) right and (B) left knees.
Case 2
A 44-year-old man presented to the office of the senior authors (R.F.W., S.R.R.) with posttraumatic left knee chronic patellar tendon rupture and proximal migration of the patella. The patient sustained this injury in a basketball game. In the acute setting, the injury was missed and the patient was misdiagnosed as lateral collateral ligament injury and treated with physical therapy for weakness and extension lag. The patient presented to our office 6 years after the injury with chronic left knee pain, instability, weakness, and extensor lag.
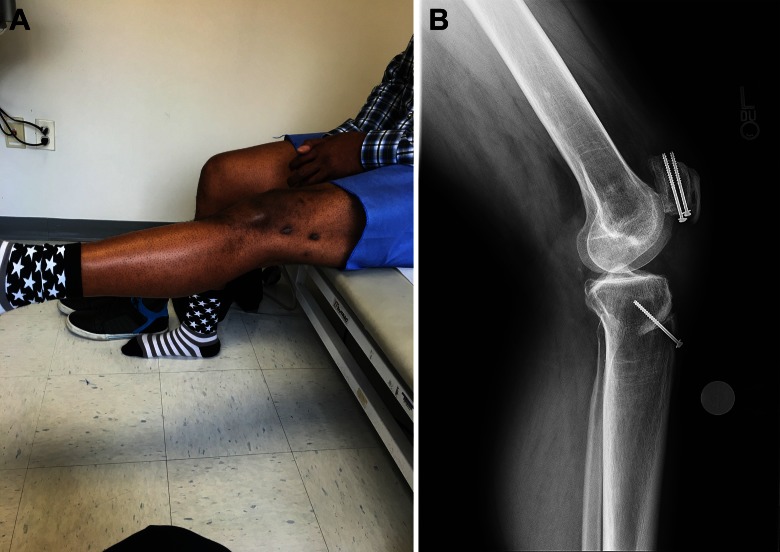
The patient had an abnormal gait pattern consistent with left-sided quadriceps weakness. He had full painless ROM of both hips and ankles. The right knee ROM was from full extension to 130° of flexion. Evaluation of the left knee revealed an extension lag of 30° (Figure 5) to 130° of flexion as ROM, with no evidence of anteroposterior or varus/valgus instability. The patella was palpated in the thigh with fixed proximal migration, and the patellar tendon could not be palpated. Atrophy of the left thigh musculature with significant scarring of the quadriceps mechanism was noted. Motor examination revealed quadriceps weakness on the left side of 4 out of 5, as opposed to 5 out of 5 quadriceps strength on the right side. Sensory and vascular examination were normal bilaterally.
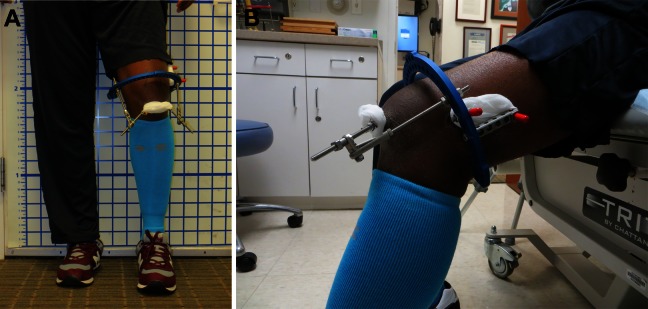
Figure 5.

Preoperative clinical photograph showing extension lag of the left knee.
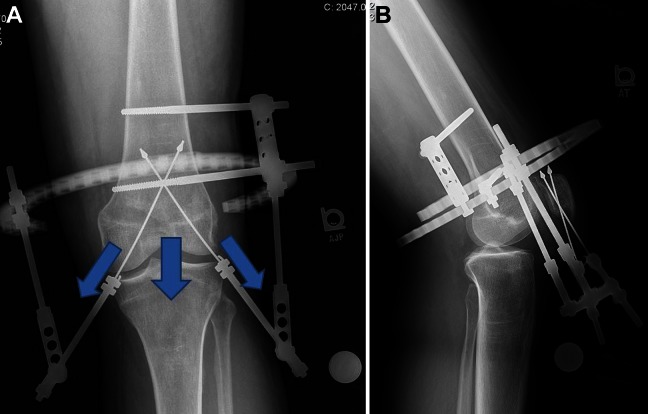
Plain radiographs of the left knee revealed a 5-cm proximal migration of the patella from the Blumensaat line; the Insall-Salvati ratio was 1.9 (Figure 6). The problem list included chronic left knee patellar tendon insufficiency with severe patella alta and contracture of the left quadriceps. The patient underwent staged operative correction. Stage 1 involved gradual distal transport and mobilization of the proximally migrated patellae using the Ilizarov/external fixation principles (Figure 7). The frame was removed after 7 weeks once the patella was in a satisfactory position. This was followed 9 days later by stage 2, which involved patellar tendon reconstruction using patellar tendon allograft.
Figure 6.
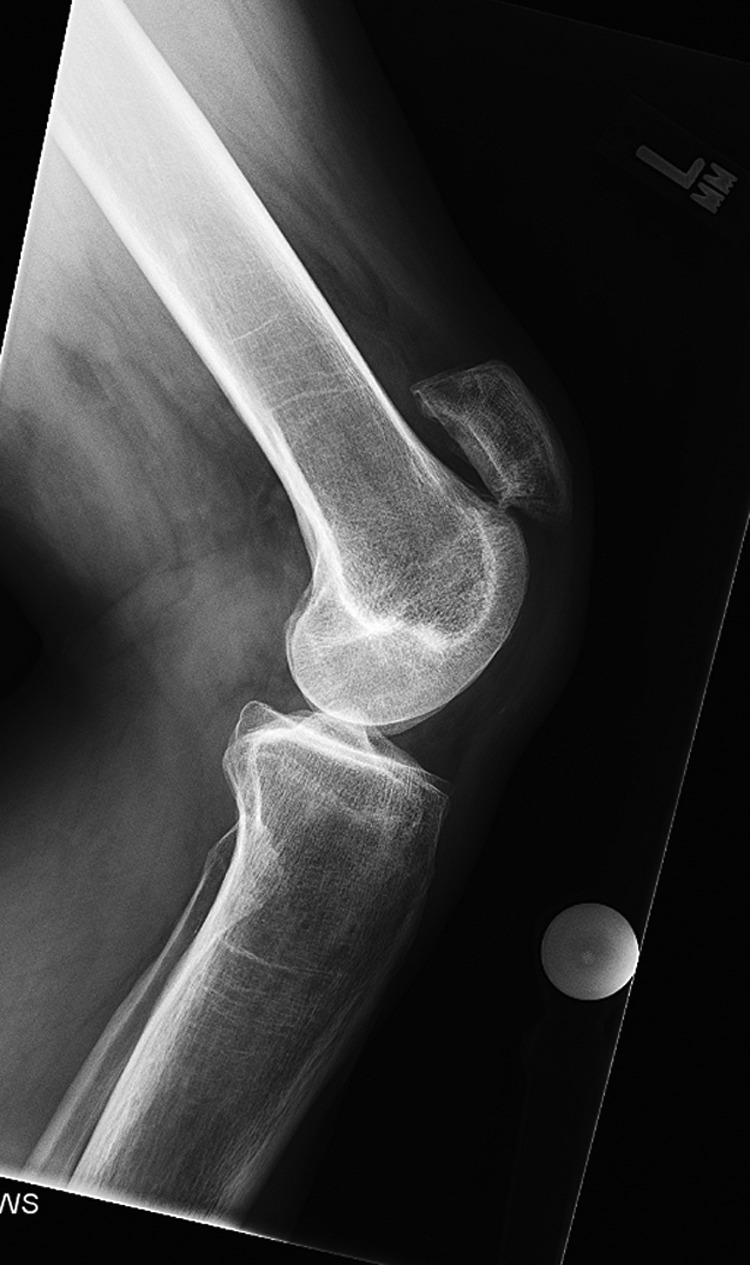
Preoperative plain lateral radiograph of the left knee showing proximal patellar migration.
Figure 7.
Postoperative clinical photographs showing the frame in the (A) standing frontal and (B) bent knee sagittal positions.
Modified Technique
A 180-mm ring was applied to the distal femur orthogonal to the femoral axis and secured with two 6-mm half pins. Next, 2 oblique olive wires were placed through the patella in a proximal to distal direction. The 2 wires were 30° off a vertical line and created a vector that was a vertical line in a proximal to distal direction. The wires were cut off the ends of the olives, and the olives were seated at the proximal medial and proximal lateral poles of the patella. The wires were attached to slotted Ilizarov rods, and a mechanism to axially pull the olive wires was created off the femoral ring. The direction was oblique to avoid the future knee incision, and the resultant vector was straight distal. Knee ROM was checked and was from full extension to 90° of flexion. Finally, the position of the frame and the wires was checked under fluoroscopy. The adjustments were started on the first postoperative day with a target of 1-mm distraction per day divided into 4 adjustments. The patient was followed up with every 2 weeks with plain radiographs of the left knee to follow the progression of distal transport of the patella (Figure 8). The target was to pull the patella distally 5 cm. We used the Insall-Salvati ratio14 for assessment of patellar height to follow the progression of distal patellar transport, and the goal was to achieve a ratio of 1.
Figure 8.
Postoperative (A) frontal and (B) lateral plain radiographs at the end of distraction showing improved patellar height of the left knee. Note the oblique distal pull on the 2 olive wires creating a resultant vector in the distal direction (arrows).
Complications
The postoperative course was complicated by deep venous thrombosis 10 days after the frame application and was treated by rivaroxaban for 3 months.
The distraction proceeded well, and correction was achieved after 6 weeks. Once the patella was in a satisfactory position, confirmed by an Insall-Salvati ratio of 1 (measured on lateral knee radiographs), the decision was made to remove the frames after 7 weeks (Figure 9) and proceed with open patellar tendon reconstruction, which was performed 9 days after the frame removal using fresh-frozen patellar tendon allograft. Proximal fixation of the patellar bone block was achieved using two 4.0-mm cannulated screws, while distal fixation of the tibial tubercle bone plug (25 mm long × 10 mm wide) into a trough in the proximal tibia was accomplished using one 4.0-mm cannulated screw. Postoperatively, ROM was initiated on the first postoperative day starting at 0° to 40°, progressing to 60° at 2 weeks, and increased gradually to 90° by 4 weeks. The patient was allowed partial weightbearing with crutches and a hinged knee brace set at 0° to 50° for 6 weeks, then continued using the brace for walking for another 4 weeks until regaining quadriceps strength. He underwent physical therapy and was able to gradually achieve full extension and recover 100° of flexion; progressive strengthening and resistance exercises were initiated at 12 weeks. The patient was followed monthly with plain radiographs, and bone healing of the tibial tubercle allograft to the proximal tibia was achieved by 16 weeks, while patellar bone block healing was achieved by 20 weeks. At follow-up, 1.5 years from the patellar tendon reconstruction, he had no pain, instability, or weakness. The patient can fully extend his left knee against gravity, with ROM from full extension to 100° of flexion with no extensor lag and can walk without limp (Figure 10). The quadriceps strength was 5 out of 5, but no functional outcome scores were obtained pre- or postoperatively.
Figure 9.
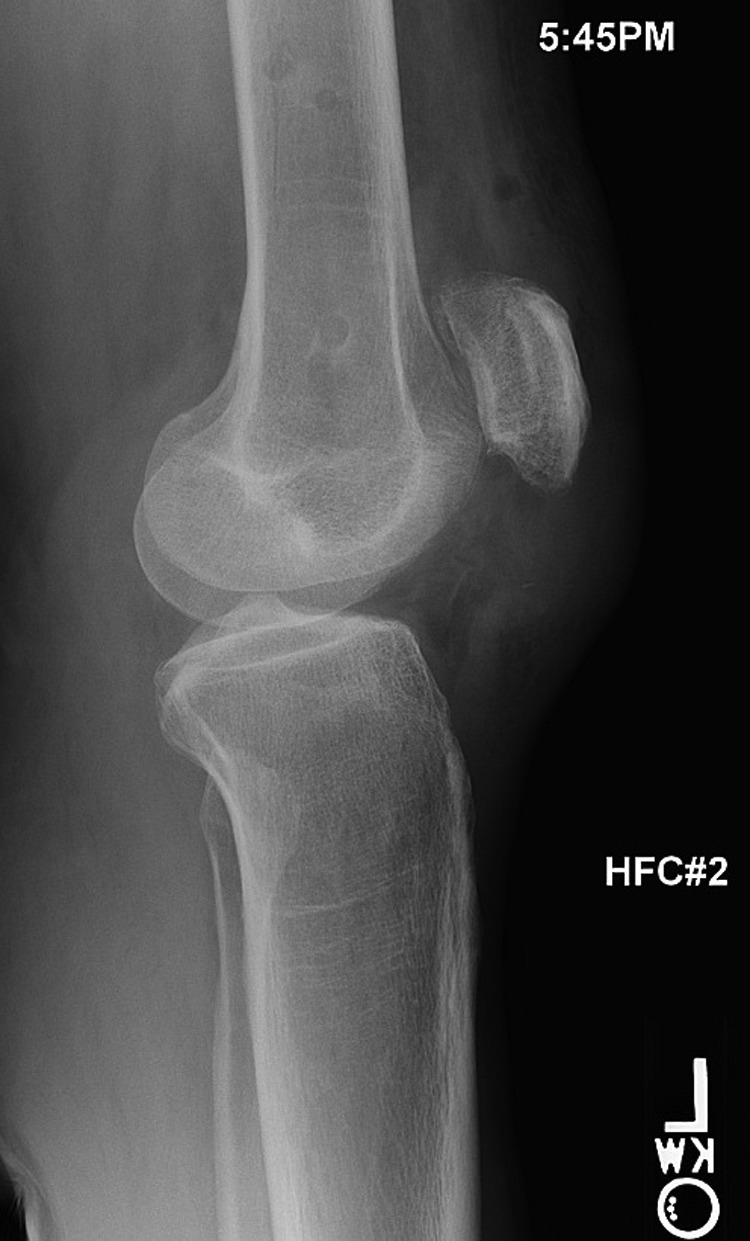
Postoperative plain lateral radiograph after frame removal.
Figure 10.
Postoperative 1-year follow-up (A) clinical photograph showing full knee extension against gravity and (B) plain lateral radiograph showing maintained patellar height with complete bone healing.
Discussion
Isolated patellar tendon rupture is an uncommon injury, usually occurring in patients younger than 40 years.22,29 The rupture may be secondary to trauma or spontaneous in patients with pathological tendon secondary to a predisposing underlying disease, including metabolic,9 rheumatoid,28 or hormonal disorders.6 Additionally, patellar tendon disruption may occur in patients after total knee arthroplasty,3 after bone–patellar tendon–bone (BPTB) autograft harvest for anterior cruciate ligament reconstruction,24 and in patients receiving local steroid injections.7 Most often, these patients are seen after acute injury for immediate management where direct surgical repair can be done with favorable results.18,31
Neglected rupture of the patellar tendon is rare, and the exact incidence is unknown.15,30,31 Patellar tendon rupture can be missed in certain situations such as obesity, polytrauma, and in patients with significant hemarthrosis, which may make palpation of the tendon defect difficult, all leading to neglected patellar tendon rupture.22,30,31 Additional diagnostic tools include radiographs that can show patella alta and MRI that can provide additional information such as the exact location of the rupture and the condition of the tendon.32 Surgical management of neglected patellar tendon rupture is more difficult than that for acute ruptures, and the results are less favorable and less predictable. The management becomes more challenging the longer it is left untreated. The technical difficulties are attributed to extensor mechanism adhesions, contracture, fixed proximal patellar migration, and quadriceps muscle atrophy.1,3,28
The goal of treatment is functional and structural restoration of the extensor mechanism to achieve active knee extension.16 There is no gold standard treatment for neglected patellar tendon ruptures. With delay in repair more than 6 weeks, the quadriceps retraction and proximal patellar migration make simple reapproximation of the tendon ends very difficult. Primary repair augmented with autogenous hamstring tendon (semitendinosus gracilis) or fascia lata graft has been used.21 Another salvage procedure is reconstruction of the extensor mechanism with an allograft, and Achilles tendon and BPTB allografts are the most commonly used, with the bone plug secured into the tendon insertion at the tibial tubercle.2 Nazarian and Booth25 reported on 36 patients treated with a fresh-frozen whole extensor mechanism allograft including quadriceps tendon, patella, patellar tendon, and tibial tubercle. The mean ROM in the entire group was 1.4° to 98° of flexion, and the mean extensor lag was 13° in 15 of 36 patients. Neyret et al26 described the use of a contralateral extensor mechanism autograft to reconstruct chronic patellar tendon ruptures. The contralateral autograft consisted of a tibial bone block, the middle third of the patellar tendon, a patellar bone block, and the central portion of the quadriceps tendon. In their case report of 2 cases, the final ROM was 0° to 90° and 0° to 120°, with no extensor lag. Synthetic materials have also been used with satisfactory results.11 Fukuta et al11 reported on the successful use of Leeds-Keio (L-K) prosthetic ligament in 2 patients with patellar tendon rupture after total knee arthroplasty, and the final ROM was –15° to 110° with no extensor lag in one patient and 0° to 105° with 5° extension lag in the other patient.
In cases with severe quadriceps tendon contracture and fixed proximal patellar migration, numerous techniques have been reported to adequately mobilize the patella and relocate it distally to its anatomic position and to reconstruct the patellar tendon; however, there is no widely accepted method. Preoperative skeletal traction has been reported but was complicated by prolonged hospitalization and knee stiffness with variable success in extensor mechanism lengthening.8,17,27,31 Siwek and Rao31 advocated 10 days of traction followed by fascia lata augmentation with external fixation using pins and wires. Mandelbaum et al20 recommended a Z lengthening of the quadriceps tendon and Z shortening of the patellar tendon with augmentation using the hamstring (semitendinosus and gracilis) tendons. Levin19 used a Dacron graft to replace the tendon followed by cast immobilization for 6 weeks.
Casey and Tietjens4 reported on 4 cases where they successfully used direct repair augmented by cerclage. Ecker et al,8 McNally and Marcelli,23 and Falconiero and Pallis10 used a single wire in a simple loop fashion to augment their repairs. Chen et al5 modified the technique by Ecker et al,8 using an autogenous hamstring graft and a circular wire through the patellar and tibial tunnels instead of a Steinman pin for patellar traction. Milankov et al24 used an autogenous contralateral BPTB graft reinforced by a double-wire loop.
The use of external fixation has been reported for patients with severe quadriceps contractures and fixed elevated patella.17,27,31,33 Isiklar et al15 reported on 2 patients with chronic patellar tendon ruptures due to failed primary repairs in which the authors used ring and wire external fixation, applying the distraction principles of Ilizarov preoperatively to mobilize the patella distally and postoperatively to protect the reconstruction while maintaining ROM and full weightbearing.
Applying the law of tension stress, Ilizarov13 showed that gradual steady traction on living tissues creates increased metabolic activity characterized by stimulated cellular proliferative and biosynthetic functions. During distraction, skin, connective tissue, blood vessels, nerves, muscles, and bones undergo increased regeneration. This was demonstrated in a canine model, where under gradual distraction at a rate of 0.125 mm every 6 hours, connective tissues and muscles showed evidence of increased metabolic activity in the form of ultrastructural changes with increased number of fibroblasts.
When using Ilizarov principles and an Ilizarov external fixator to treat these neglected ruptures, full weightbearing and ROM of the knee can be maintained. Other advantages include minimized hospitalization time and controlled lengthening speed and duration.
To our knowledge, this is the second case report study that demonstrates successful use of external fixation to mobilize and distally relocate the patella by lengthening of the extensor mechanism as a first stage prior to second-stage reconstruction of the patellar tendon. In the first case report by Isiklar et al,15 these authors also used external fixation for protection after the patellar tendon reconstruction, but we did not find this to be needed. In their case report, Isiklar et al15 reported on successful use of external fixation to treat 2 patients with chronic patellar tendon ruptures with failed primary repair, presenting 3.5 years and 8 months after the initial injury, the final ROM achieved was 0° to 130° in 1 patient and 0° to 110° in the second patient, with no extensor lag, normal Insall-Salvati ratio, and 5 out of 5 quadriceps strength in both patients. Those results were most similar to the results we achieved. Furthermore, we have modified the technique in the second case presented in this case report study. The advantage of the external fixation technique used in the second case was that the wires did not cut through the skin as the patella was transported distally. The wires were pulled axially through a small wire site at the skin minimizing skin trauma. Despite the high rate of complications encountered, specifically the pin tract infection in the first patient and deep vein thrombosis in the second patient, those complications were managed conservatively and appropriately without the need to reoperate and without any effect on the final outcome of the procedure.
Conclusion
The use of pins and wires for external fixation (applying the lengthening principles of Ilizarov) provides a practical salvage solution for the treatment of neglected patellar tendon ruptures. Although, this technique facilitates reconstruction of chronic patellar tendon rupture, it should be reserved for patients with severe soft tissue contractures, adhesions, and fixed proximal patellar migration. The surgeon must have experience applying the Ilizarov external fixation.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Bek D, Demiralp B, Kömürcü M, Sehirlioǧlu A. Neglected patellar tendon rupture: a case of reconstruction without quadriceps lengthening. J Orthop Traumatol. 2008;9:39–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Burks RT, Edelson RH. Allograft reconstruction of the patellar ligament: a case report. J Bone Joint Surg Am. 1994;76:1077–1079. [DOI] [PubMed] [Google Scholar]
- 3. Cadambi A, Engh GA. Use of a semitendinosus tendon autogenous graft for rupture of the patellar ligament after total knee arthroplasty. A report of seven cases. J Bone Joint Surg Am. 1992;74:974–979. [PubMed] [Google Scholar]
- 4. Casey MT, Jr, Tietjens BR. Neglected ruptures of the patellar tendon. A case series of four patients. Am J Sports Med. 2001;29:457–460. [DOI] [PubMed] [Google Scholar]
- 5. Chen B, Li R, Zhang S. Reconstruction and restoration of neglected patellar tendon using semitendinosus and gracilis tendons with preserved distal insertions: two case reports. Knee. 2012;19:508–512. [DOI] [PubMed] [Google Scholar]
- 6. Chen CH, Niu CC, Yang WE, Chen WJ, Shih CH. Spontaneous bilateral patellar tendon rupture in primary hyperparathyroidism. Orthopedics. 1999;22:1177–1179. [DOI] [PubMed] [Google Scholar]
- 7. Clark SC, Jones MW, Choudhury RR, Smith E. Bilateral patellar tendon rupture secondary to repeated local steroid injections. J Accid Emerg Med. 1995;12:300–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ecker ML, Lotke PA, Glazer RM. Late reconstruction of the patellar tendon. J Bone Joint Surg Am. 1979;61:884–886. [PubMed] [Google Scholar]
- 9. ElGuindy A, Lustig S, Servien E, et al. Treatment of chronic disruption of the patellar tendon in osteogenesis imperfecta with allograft reconstruction. Knee. 2010;18:121–124. [DOI] [PubMed] [Google Scholar]
- 10. Falconiero RP, Pallis MP. Chronic rupture of a patellar tendon: a technique for reconstruction with Achilles allograft [case report]. Arthroscopy. 1996;12:623–626. [DOI] [PubMed] [Google Scholar]
- 11. Fukuta S, Kuge A, Nakamura M. Use of the Leeds-Keio prosthetic ligament for repair of patellar tendon rupture after total knee arthroplasty. Knee. 2003;10:127–130. [DOI] [PubMed] [Google Scholar]
- 12. Gries PE, Lahav A, Holmstrom MC. Surgical treatment options for patella tendon rupture, part II: chronic. Orthopedics. 2005;28:765–769. [DOI] [PubMed] [Google Scholar]
- 13. Ilizarov GA. The tension stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989;238:249–281. [PubMed] [Google Scholar]
- 14. Insall J, Salvati EA. Patella position in the normal knee joint. Radiology. 1979;101:101–104. [DOI] [PubMed] [Google Scholar]
- 15. Isiklar ZU, Varner KE, Lindsey RW, et al. Late reconstruction of patellar ligament ruptures using Ilizarov external fixation. Clin Orthop Relat Res. 1996;322:174–178. [PubMed] [Google Scholar]
- 16. Jarvela T, Halonen P, Jarvela K, Moilanen T. Reconstruction of ruptured patellar tendon after total knee arthroplasty: a case report and a description of an alternative fixation method. Knee. 2005;12:139–143. [DOI] [PubMed] [Google Scholar]
- 17. Kelikian H, Riashi E, Gleason J. Restoration of quadriceps function in neglected tear of the patellar tendon. Surg Gynecol Obstet. 1957;104:200–204. [PubMed] [Google Scholar]
- 18. Kuechle DK, Stuart MJ. Isolated rupture of the patellar tendon in athletes. Am J Sports Med. 1994;22:692–695. [DOI] [PubMed] [Google Scholar]
- 19. Levin PD. Reconstruction of the patellar tendon using a Dacron graft: a case report. Clin Orthop Relat Res. 1976;118:70–72. [PubMed] [Google Scholar]
- 20. Mandelbaum BR, Bartolozzi A, Carney B. A systematic approach to reconstruction of neglected tears of the patellar tendon. Clin Orthop Relat Res. 1988;235:268–271. [PubMed] [Google Scholar]
- 21. Matava MJ. Patellar tendon ruptures. J Am Acad Orthop Surg. 1996;4:287–296. [DOI] [PubMed] [Google Scholar]
- 22. McGrory JE. Disruption of the extensor mechanism of the knee. J Emerg Med. 2003;24:163–168. [DOI] [PubMed] [Google Scholar]
- 23. McNally PD, Marcelli EA. Achilles allograft reconstruction of a chronic patellar tendon rupture [case report]. Arthroscopy. 1998;14:340–344. [DOI] [PubMed] [Google Scholar]
- 24. Milankov Ziva M, Semnic R, Miljkovic N, Harhaji V. Reconstruction of patellar tendon rupture after anterior cruciate ligament reconstruction: a case report. Knee. 2008;15:419–422. [DOI] [PubMed] [Google Scholar]
- 25. Nazarian DG, Booth RE., Jr Extensor mechanism allografts in total knee arthroplasty. Clin Orthop Relat Res. 1999;367:123–129. [PubMed] [Google Scholar]
- 26. Neyret P, Donell ST, Carret JP, et al. Patellar ligament rupture treated by contralateral patellar ligament autograft and its application in patients with tibial allografts. Knee. 1994;1:158–160. [Google Scholar]
- 27. Nsouli AZ, Nsouli TA, Haidar R. Late reconstruction of the patellar tendon: case report with a new method of repair. J Orthop Trauma. 1991;31:1319–1321. [PubMed] [Google Scholar]
- 28. Prasad S, Lee A, Clarnette R, Faull R. Spontaneous bilateral patellar tendon rupture in a woman with previous Achilles tendon rupture and systemic lupus erythematosus. Rheumatology (Oxford). 2003;42:905–906. [DOI] [PubMed] [Google Scholar]
- 29. Scott WN, Insall JN. Injuries of the knee In: Rockwood CA, Jr, Green DP, Bucholz RW, eds. Fractures in Adults. 3rd ed Philadelphia, PA: JB Lippincott; 1991:1799–1914. [Google Scholar]
- 30. Shephard GJ, Christodoulou L, Hegap AI. Neglected rupture of the patellar tendon. Arch Orthop Trauma Surg. 1999;119:241–242. [DOI] [PubMed] [Google Scholar]
- 31. Siwek CW, Rao JP. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am. 1981;63:932–937. [PubMed] [Google Scholar]
- 32. Sutherland F, Dawson JS, Moran CG. MRI detection of partial rupture of the patellar tendon in association with multiple ligament injuries of the knee its surgical importance. Injury Extra. 2005;36:6–8. [Google Scholar]
- 33. Takebe K, Hirohata K. Old rupture of the patellar tendon. Clin Orthop Relat Res. 1985;196:253–255. [PubMed] [Google Scholar]