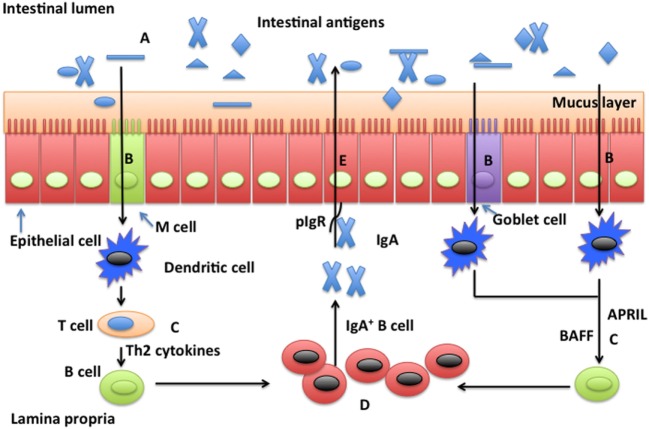
Figure 1.
Possible mechanisms whereby glutamine promotes secretion of intestinal secretory immunoglobulin A. Intestinal secretory immunoglobulin A (SIgA) production requires stimulation via a T cell-dependent or a T cell-independent pathway. In the T cell-dependent pathway (left), M cells sample and deliver antigens from the intestinal lumen to dendritic cells (DCs) in the underlying subepitheilal dome region. DCs activate T cells in the interfollicular region and stimulate production of Th2 cytokines necessary for the differentiation of immature B cells into IgA-secreting plasma cells. In the T cell-independent pathway (right), release of the B cell-activating factor of the tumor necrosis factor family (BAFF) and a proliferation-inducing ligand (APRIL) from DCs promote T cell-independent mucosal IgA responses. Other factors, such as vasoactive intestinal peptide (VIP), IgA-inducing protein (IGIP), and nitric oxide (NO) also play important roles (not shown) in T-cell-independent pathways. SIgA is transported across the epithelium after binding to the polymeric immunoglobulin receptor (pIgR). In the intestinal lumen, SIgA binds intestinal antigens from microbes and diet. Glutamine may affect intestinal production of SIgA through intestinal microbiota (A), antigen sampling and presentation (B), induction pathways for SIgA production by plasma cells via either a T cell-dependent and T cell-independent pathway (C), activation and homing of IgA+ plasma cells (D), and transport of SIgA (E).