Abstract
Background
In‐hospital cardiac arrest (IHCA) is a major public health problem with significant mortality. A better understanding of where IHCA occurs in hospitals (intensive care unit [ICU] versus monitored ward [telemetry] versus unmonitored ward) could inform strategies for reducing preventable deaths.
Methods and Results
This is a retrospective study of adult IHCA events in the Get with the Guidelines—Resuscitation database from January 2003 to September 2010. Unadjusted analyses were used to characterize patient, arrest, and hospital‐level characteristics by hospital location of arrest (ICU versus inpatient ward). IHCA event rates and outcomes were plotted over time by arrest location. Among 85 201 IHCA events at 445 hospitals, 59% (50 514) occurred in the ICU compared to 41% (34 687) on the inpatient wards. Compared to ward patients, ICU patients were younger (64±16 years versus 69±14; P<0.001) and more likely to have a presenting rhythm of ventricular tachycardia/ventricular fibrillation (21% versus 17%; P<0.001). In the ICU, mean event rate/1000 bed‐days was 0.337 (±0.215) compared with 0.109 (±0.079) for telemetry wards and 0.134 (±0.098) for unmonitored wards. Of patients with an arrest in the ICU, the adjusted mean survival to discharge was 0.140 (0.037) compared with the unmonitored wards 0.106 (0.037) and telemetry wards 0.193 (0.074). More IHCA events occurred in the ICU compared to the inpatient wards and there was a slight increase in events/1000 patient bed‐days in both locations.
Conclusions
Survival rates vary based on location of IHCA. Optimizing patient assignment to unmonitored wards versus telemetry wards may contribute to improved survival after IHCA.
Keywords: critical care, in‐hospital cardiac arrest, outcome, resuscitation
Subject Categories: Cardiopulmonary Resuscitation and Emergency Cardiac Care, Cardiopulmonary Arrest
Introduction
In‐hospital cardiac arrest (IHCA) affects more than 200 000 inpatients in the United States annually.1 The current literature reports significant variability across hospitals in IHCA survival rates ranging from as low as zero survival to 36.2% survival in an adjusted analysis of US hospitals in the Get With the Guidelines—Resuscitation (GWTG‐R) Registry.2 Survival and neurologic outcomes following IHCA have improved substantially over the last decade, yet the reasons for the improvements are unclear.3 Some studies have suggested that patient outcomes are improved if the IHCA is witnessed, or if patients are in monitored settings.4, 5 A consensus statement published by the American Heart Association in March 2013 highlighted variability in IHCA management plans across US hospitals, improved survival in patients with witnessed IHCA, and guidance on which patients would benefit from increased monitoring.6 Prior work has shown, however, that hospitals differ in where IHCA occurs, and the degree to which hospitals are able to align with the recommendations outlined in the above guideline is not well understood.5, 7
Understanding the current state of where IHCA locations differ in hospitals across the United States is an important step to identifying how to best direct location‐specific efforts at reducing IHCA incidence and improving IHCA‐associated morbidity and mortality. This study seeks to fill the knowledge gap regarding the location where patients suffer IHCA across US hospitals, the potential effect of location on survival, and the trends in location over time.
In this study, we sought to describe (1) patient and hospital characteristics of IHCA by hospital location, (2) the event rate and proportion of survival of IHCA occurring in the ICU versus inpatient wards (monitored and unmonitored beds), and (3) temporal trends in IHCA in the ICU versus inpatient ward over time.
Methods
Design
We conducted a retrospective study using data from GWTG‐R, formerly known as the National Registry of Cardiopulmonary Resuscitation. While this registry has been enrolling patients since January 2000, data on event location became well defined after 2003. In this database, a “cardiac arrest” event is defined as a resuscitation that requires chest compressions and/or defibrillation.8 Event location was reported for each event using the Resuscitation Patient Management Tool provided by GWTG‐R. The design of the registry has been described in detail elsewhere.8 Institutions that do not staff an ICU were excluded from this analysis. This study was approved by the University of Pennsylvania Institutional Review Board. The requirement for informed consent was waived.
Study Population
We identified all IHCA events reported to the registry from January 1, 2003 to September 14, 2010. All patients over 18 years old were eligible for inclusion. Hospitals with fewer than 5 events per year, events outside of the hospital and in locations besides an inpatient ward or ICU were excluded (eg, procedure locations, delivery suite, ambulatory units, and the emergency department). Patients were categorized as being ward patients if they were reported to be in a general inpatient area, on telemetry, or in a step‐down unit. Patients were categorized as being in the ICU if they were located in an adult ICU or cardiac ICU. Hospitals with missing data regarding inpatient bed‐days were also excluded.
By arrest location (ICU versus ward), we described patient, arrest, and hospital‐level characteristics. Patient characteristics include age, sex, race/ethnicity, and pre‐arrest comorbidities; arrest characteristics included initial arrest rhythm, and immediate cause of arrest; and hospital characteristics included hospital size (small, medium, large) and affiliation (academic, urban, private). Hospital characteristics were abstracted from the American Hospital Association Annual Survey.
Event Rate and Proportion of Survivors by Location (ICU Versus Inpatient Ward)
To calculate each hospital's event rate by location, we calculated the mean number of IHCA events divided by 1000 hospital bed‐days. Hospital bed‐days were selected as the incidence “denominator” measurement of the population at risk, analogous to person‐time,9, 10 as the true denominator of total admissions by location is not routinely reported by hospital and so it was not available. Hospital bed‐days were estimated from data reported to the annual American Hospital Association survey and linked by GWTG‐R statisticians with the closest year of data in GWTG‐R. Using event data from GWTG‐R (numerator) and hospital bed days (denominator), we were able then to calculate the rate of IHCA by hospital location (ICU versus inpatient ward).
Of IHCA events occurring in the ICU and inpatient ward, we also calculated the proportion of survivors to discharge by arrest location. This analysis was completed to describe the event rates for patients who arrested outside of the ICU but in monitored ward settings (ie, telemetry) versus unmonitored ward settings.
In order to describe an adjusted survival rate, we created a generalized estimating equation regression model to determine how the covariates affected the survival outcome. Covariates that were associated with outcome were accounted for in the adjusted results. The covariates included age, race, medical comorbidities, residence, cause of arrest, initial rhythm, timing of arrest (day/night/weekend) and finally, witnessed arrest.
Temporal Trends in IHCA in the ICU Versus Inpatient Wards
IHCA rates were plotted by year and by location to evaluate changes over the study period. The proportion of patients who survived IHCA to hospital discharge were plotted by location over the 7‐year study time period to evaluate for a trend.
Statistical Analysis
Descriptive statistics were used to describe arrest locations (ICU versus inpatient ward) relative to patient, arrest, and hospital‐level characteristics. Student t tests were performed for continuous variables and χ2 tests were used for categorical variables. P‐values <0.05 were considered significant.
We compared the mean IHCA event rate/1000 bed‐days by hospital location (ICU versus inpatient monitored ward versus inpatient unmonitored ward) for all hospitals in the cohort. The proportion of survivors to events by location is also reported for the entire cohort and over the study time frame. Tests for significance were completed using ANOVA, and pairwise comparisons were made between the 3 varying patient settings.
Statistical analyses were performed using SAS version 9.3 (SAS Institute Inc, Cary, NC). The Institutional Review Board at the University of Pennsylvania approved this study.
Results
There were 85 201 IHCA events at 455 hospitals included in the study cohort (Figure 1).
Figure 1.
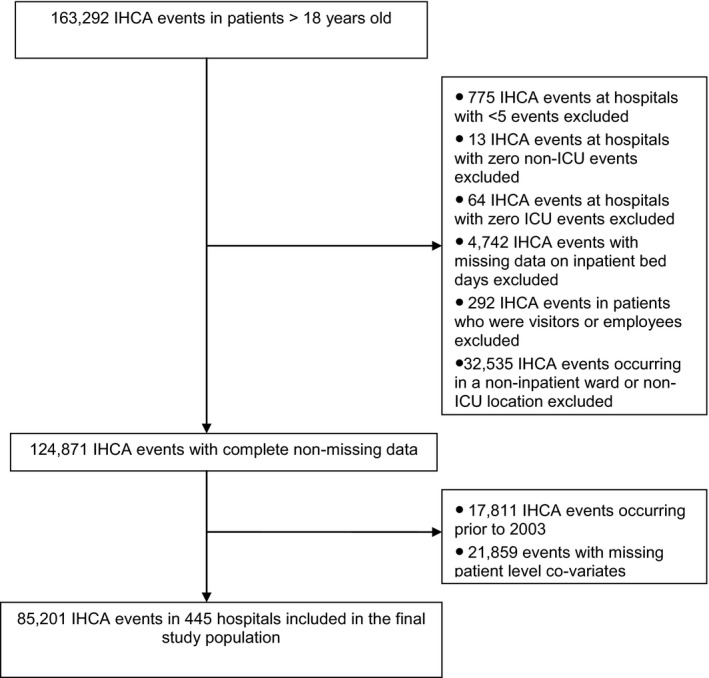
Utstein consort diagram. This figure illustrates study inclusion and exclusion criteria. ICU indicates intensive care unit; IHCA, in‐hospital cardiac arrest.
Patient Demographics
Of IHCA, 59% (50 514) of events occurred in the ICU compared to 41% (34 687) on inpatient wards (P<0.0001). Patients who arrested in the ICU were younger than ward patients (64±16 versus 69±14 years; P<0.0001), and were more likely to have preexisting hypoperfusion, pulmonary disease, renal and hepatic insufficiency, metabolic abnormalities, and sepsis (Table 1).
Table 1.
Patient and Arrest Level Characteristics of IHCA Events by Hospital Locations
| ICU, % (n) | Inpatient Ward, % (n) | P‐Value | |
|---|---|---|---|
| All patients | 59 (50 514) | 41 (34 687) | |
| Patient demographics | |||
| Age, mean y (SD) | 64 (16) | 69 (14) | <0.0001 |
| Male | 59 (29 583) | 58 (19 980) | <0.0001 |
| Race | |||
| White | 68 (34 569) | 70 (24 238) | <0.0001 |
| Black | 20 (10 320) | 21 (7301) | |
| Other | 11 (5625) | 9 (3148) | |
| Existing conditions | |||
| Neurologic | 26 (13 253) | 24 (8488) | <0.0001 |
| Cardiac | 75 (38 032) | 76 (26 303) | <0.0001 |
| Pulmonary | 68 (34 449) | 33 (11 562) | <0.0001 |
| Renal insufficiency | 39 (19 536) | 33 (11 548) | <0.0001 |
| Hepatic insufficiency | 10 (5150) | 6 (2229) | <0.0001 |
| Diabetes mellitus | 30 (15 228) | 34 (11 920) | <0.0001 |
| Metabolic abnormalities | 22 (11 045) | 13 (4532) | <0.0001 |
| Hypotension | 39 (19 528) | 15 (5141) | <0.0001 |
| Septicemia | 22 (11 292) | 13 (4408) | <0.0001 |
| Malignancy | 12 (6155) | 15 (5290) | <0.0001 |
| Major trauma | 5 (2543) | 2 (634) | <0.0001 |
| Arrest characteristics | |||
| Initial rhythm | |||
| Asystole | 33 (16 493) | 43 (15 025) | <0.0001 |
| PEA | 47 (23 611) | 40 (13 707) | |
| VT/VF | 21 (10 410) | 17 (5955) | |
| Cause of arrest | |||
| Cardiac | 69 (34 920) | 59 (20 379) | <0.0001 |
| Respiratory | 39 (19 929) | 46 (15 924) | <0.0001 |
| Neurologic | 1 (551) | 1 (346) | 0.0288 |
| Metabolic | 57 (28 567) | 31 (10 670) | <0.0001 |
ICU indicates intensive care unit; IHCA, in‐hospital cardiac arrest; PEA, pulseless electrical activity; VT/VF, ventricular tachycardia/ventricular fibrillation.
Arrest Characteristics
Arrests characterized by pulseless electrical activity and asystole were predominant in both populations, with 80% of the ICU population suffering a nonshockable initial rhythm and 83% of ward patients arresting due to asystole/pulseless electrical activity. Patients who arrested in the ICU had a slightly higher rate of ventricular tachycardia or ventricular fibrillation versus patients on the inpatient wards (21% versus 17%, P<0.0001). In the ICU, the cause of IHCA was more commonly cardiac (69% versus 59%, P<0.0001) or metabolic (57% versus 31%, P<0.0001) (Table 1) when compared with the inpatient ward.
Hospital Characteristics
There was a significantly higher proportion of IHCA in the ICU compared to the inpatient wards in all hospital types (Table 2).
Table 2.
Hospital Characteristics
| ICU, % (n=50 514) | Inpatient Ward, % (n=34 687) | P‐Value | |
|---|---|---|---|
| Hospital characteristics | |||
| Academic (223), n=55 895 | 60 (33 724) | 40 (22 171) | <0.001 |
| Nonacademic (211), n=29 306 | 57 (16 790) | 43 (12 516) | |
| Urban (386), n=78 896 | 60 (46 973) | 40 (31 923) | <0.001 |
| Rural (48), n=6305 | 56 (3541) | 44 (2764) | |
| Private (65), n=9865 | 63 (6257) | 37 (3608) | <0.001 |
| Public (369), n=75 336 | 59 (44 257) | 41 (31 079) | |
| Size (beds) | |||
| Small (6–99), n=16 533 | 59 (9742) | 41 (6791) | 0.03 |
| Medium (100–400), n=36 506 | 59 (21 602) | 41 (14 904) | |
| Large (>400), n=30 140 | 60 (18 092) | 40 (12 048) | |
ICU indicates intensive care unit.
IHCA Event Rate by Location
The mean event rate of IHCA in the ICU was 0.337 (±0.215) events per 1000 patient‐bed days compared with inpatient ward patients dichotomized into either a monitored ward bed (telemetry) versus an unmonitored ward bed, which was 0.109 (±0.079) events per 1000 patient‐bed days and 0.134 (±0.098), respectively. Using ANOVA, these event rates were statistically different (P<0.001). Via pairwise comparison, we found significant differences in event rate in the ICU versus monitored ward (P<0.0001), ICU versus unmonitored ward (P<0.0001), and monitored versus unmonitored ward (P<0.01) (Table 3).
Table 3.
Event Rate (Number of Events Per Year Per 1000 Inpatient Bed‐Days) and Survival Rates (Percent of Survivals Among Arrest Events Per Year Per Location)
| Total | ICU | Monitored Ward | Unmonitored Ward | P‐Valuea | |
|---|---|---|---|---|---|
| No. of hospitals | 445 | 445 | 445 | 445 | |
| Unadjusted event rate, mean (SD) | 0.580 (0.325) | 0.337 (0.215) | 0.109 (0.079) | 0.134 (0.098) | <0.0001 |
| Unadjusted survival rate, mean (SD) | 0.173 (0.079) | 0.162 (0.096) | 0.231 (0.171) | 0.141 (0.122) | <0.0001 |
| Adjusted survival rate, mean (SD) | 0.144 (0.032) | 0.140 (0.037) | 0.193 (0.074) | 0.106 (0.037) | <0.0001 |
ICU indicates intensive care unit.
P‐value obtained via ANOVA.
IHCA Survival: ICU Versus Inpatient Wards
On adjusted analysis, survival was best for patients in a monitored ward setting (19.3%) followed by ICU setting (14%) and finally an unmonitored ward setting (10.6%) (Table 3). These results represent survival in the wards and ICU and specifically exclude patients who arrest in other locations, including the emergency department and treatment areas within the hospital (Figure 1).
Temporal Trends in IHCA in the ICU Versus Inpatient Wards
The mean event rate of IHCA/1000 patient bed‐days was also higher in the ICU across all years of the study (2003–2010) (Figure 2). The proportion of patients who survived IHCA improved over the 7‐year period and with greater improvement in survival rates observed in the inpatient ward than in the ICU setting (P<0.001) (Figure 3).
Figure 2.
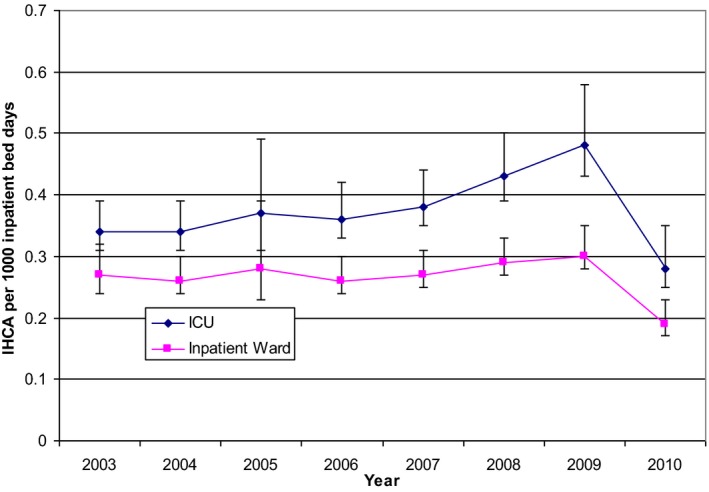
Rate of in‐hospital cardiac arrest/1000 patient bed‐days by location. This figure illustrates the rate of IHCA/1000 patient bed‐days by location per year over the study period. (Data were collected from January 1, 2003 to September 14, 2010, and therefore 2010 is incomplete). IHCA indicates in‐hospital cardiac arrest.
Figure 3.
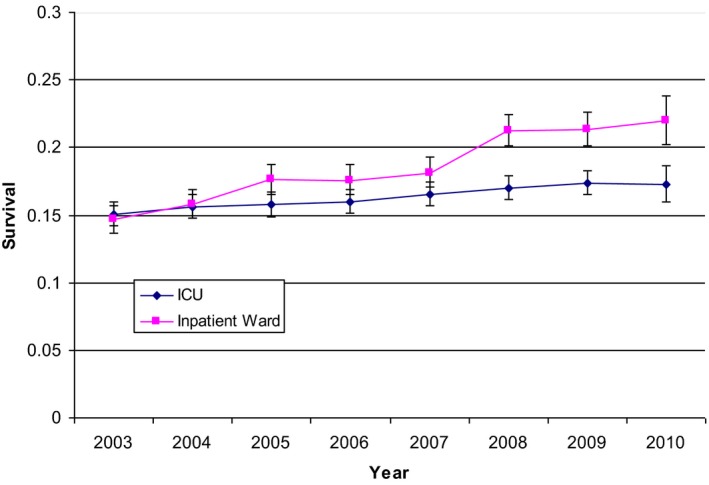
Survival by location over time. This figure illustrates the proportion of patients who survived to discharge after IHCA by location and year over the study period. ICU indicates intensive care unit; IHCA, in‐hospital cardiac arrest.
Discussion
This study has 3 main findings: (1) Patient and hospital characteristics of IHCA vary when comparing events in the ICU versus inpatient wards. (2) IHCA is more common in the ICU than in inpatient wards. (3) Survival from IHCA on the inpatient monitored ward is higher than in the ICU, and survival from IHCA in an unmonitored ward setting has the worst survival.
In our study, most IHCA occurred in the ICU (59%), slightly higher than reports from smaller studies.5 Prior work has suggested that location of IHCA is an important factor in patient outcomes, with significantly better outcomes for those that occur in monitored settings.11, 12, 13 The drivers of improved outcomes in monitored settings such as the ICU are likely multifactorial including immediate availability of advanced life support, monitored and witnessed status of cardiac arrests, and greater nurse‐to‐patient ratios.14 Additionally, there may be an element of selection bias in the ICU, where patients who are often unlikely to benefit from resuscitation have establishment of “do not resuscitate” policies. Given an expected mortality rate of 20% to 40% in the ICU and the introduction of rapid response systems to transfer high‐risk patients to an ICU, a high rate of IHCA in the ICU seems consistent.15 However, prior work has demonstrated that 78% to 90% of ICU deaths occur after decisions to withhold or withdraw life support.15 Therefore, it raises the question of whether the expected rate of IHCA in the ICU should be this high.
In addition to the ICU, our study investigated the event rate and survival of a second monitored setting, the inpatient ward telemetry bed. We found that these patients had a better chance for survival versus the ICU patient who is most often more critically ill and the unmonitored ward patient whose resuscitation may be delayed by a lack of timely detection. This finding supports a prior theory that early detection and rapid intervention impart improved outcomes, and not surprisingly, ward patients with less critical illness than ICU patients have a better chance for survival.
Our study findings also showed that over time there has been an increase in IHCA events occurring in an ICU setting, suggesting that hospitals may be attempting to concentrate patients at risk for IHCA in highly monitored settings. We specifically observed a slight increase in rates of IHCA in the ICU in 2008–2010. This could reflect the introduction of rapid response teams. In 2008, the Joint Commission mandated that all US hospitals implement a system to improve recognition and response to changes in a patient's condition.16 A systematic review of studies evaluating the effectiveness of rapid response systems found that their implementation was associated with significant reductions in non‐ICU IHCA.17 However, this same study showed there was no overall mortality benefit. One possibility is that patients who experience a rapid response on an inpatient ward may be transferred to an ICU setting while at high risk for IHCA. However, IHCA may still happen quickly following transfer from an inpatient ward, leaving little time for critical care interventions.
Our study shows that over the study time frame (2003–2010), survival improved with more improvement noted for IHCA on inpatient wards. The greater improvement in survival demonstrated when a patient is on the inpatient ward may reflect the relationship between severity of illness and survival after IHCA. Temporal improvement in survival regardless of IHCA location can be attributed to multiple potential factors including an increased emphasis on quality of resuscitation (high‐quality chest compressions with limited interruption, early defibrillation) and the utilization of postarrest care bundles (eg, early cardiac catheterization, targeted temperature management, and hemodynamic optimization).18 We propose that greater advances in IHCA survival might be realized with careful attention to the assignment of patient location for individuals at risk for catastrophic events such as cardiac arrest.
Identifying the patient most at risk for decompensating is a complex task and given limitations in resource allocation, it is not feasible to place all patients in critical care beds. However, our findings indicate that patients who suffer IHCA survive at higher rates in monitored settings (ICU and telemetry units). Preventing IHCA will always be the better alternative for improving overall patient health outcomes; however, placing at‐risk patients with a high likelihood for IHCA in monitored settings may contribute to furthering the already observed trends in improved survival after IHCA. Further study to identify these individuals at risk for IHCA will potentially contribute to improved outcomes or better yet, prevention of IHCA.
Limitations
Limitations of our study are consistent with those of large multicenter databases. Participation in GWTG‐R is voluntary and represents ≈15% of hospitals in the United States. It is therefore possible that nonparticipating institutions may be different from those hospitals choosing to participate. To date, however, GWTG‐R is the largest global registry of IHCA and findings from this data set have impacted national and international resuscitation policies and guidelines. Although this data set includes significant hospital‐level data, there were limitations. One limitation of this data set is that overall hospital occupancy is unknown, and therefore, we are unclear how this factor may affect patient location and therefore, patient location when they arrest.
We could not adjust for severity of illness or source of admission, which may significantly affect whether a patient carried a “do not resuscitate” order or individual wishes regarding specific goals of care. We also could not adjust for the presence or lack of a “rapid response system,” which may impact the location of IHCA but was not available for all years of the data. We also report event rates by hospital types, but there is likely confounding across hospital types (eg, academic and size) that may account for some of the variations in rates. We compared ICU to inpatient wards and recognize that there is variability across hospitals in how these areas are accessed, staffed (eg, patient‐to‐provider ratio, provider training, provider coverage days versus nights), and monitored (eg, telemetry, virtual tracking).19 Finally, we give event rates per 1000 hospital bed‐days, but are unable to account for all bed types. Our overall estimation is that ICU and ward beds account for the majority of hospital bed‐days; however, the number of observation beds was not accounted for in this analysis, as we did not have that level of specificity from each hospital reporting data. Additionally, we are not aware of any source that has bed days by location, so we were limited in our application of total hospital bed‐days by location, which may introduce bias in our estimates.
Conclusions
Over half of all IHCA occurs in the ICU, where patients are highly monitored and resources are intense. However, patients in the ICU are critically ill and therefore successful resuscitation after IHCA with meaningful survival is complicated by the underlying pathophysiology that required the initial ICU admission. IHCA also occurs at a high rate on inpatient wards and while some of these events are unpredictable, monitoring that potentially could lead to earlier recognition may impart better survival outcomes. Understanding who is at highest risk for IHCA and placing those individuals in the best setting for high‐level resuscitation is of utmost importance. Further work identifying the patient‐level predictors of cardiac arrest and factors that most contribute to improved outcomes will be important in helping providers and hospitals implement systems to prevent IHCA when possible and improve outcomes when inevitable.
Appendix
The American Heart Association's Get With the Guidelines®—Resuscitation (formerly the National Registry of Cardiopulmonary Resuscitation) Investigators: Robert A. Berg (study author), Graham Nichol, Vinay M. Nadkarni, Mary Ann Peberdy, Paul S. Chan, Tim Mader, Karl B. Kern, Sam Warren, Emilie Allen, Brian Eigel, Elizabeth A. Hunt, Joseph P. Ornato, Scott Braithwaite, Romergryko G. Geocadin, Mary E. Mancini, Jerry Potts, and Tanya Lane Truitt.
Disclosures
Dr Churpek has a patent pending (ARCD. P0535US.P2) for risk‐stratification algorithms for hospitalized patients and research support from the National Institutes of Health (NIH) (K08 HL121080). Dr Edelson has a patent pending (ARCD. P0535US.P2) for risk stratification algorithms for hospitalized patients, research support and honoraria from Philips Healthcare (Andover, MA) and an honorarium from Early Sense (Tel Aviv, Israel), and ownership interest in Quant HC (Chicago, IL), which is developing products for risk stratification of hospitalized patients. Dr Mikkelsen has research support from the NIH. Dr Merchant has grant/research support from the NIH (K23 10714038), pilot funding from Physio‐Control, Seattle, WA; Zoll Medical, Boston, MA; Cardiac Science, Bothell, WA; Philips Medical, Seattle, WA. Dr Perman has research support from the NIH (K12 HD057022). The remaining authors have no conflicts to disclose.
(J Am Heart Assoc. 2016;5:e003638 doi: 10.1161/JAHA.116.003638)
References
- 1. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DP, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB; on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–e322. [DOI] [PubMed] [Google Scholar]
- 2. Merchant RM, Berg RA, Yang L, Becker LB, Groenveld PW, Chan PS. Hospital variation in survival after in‐hospital cardiac arrest. J Am Heart Assoc. 2014;3:e000400 doi: 10.1161/JAHA.113.000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Girotra S, Chan PS. Trends in survival after in‐hospital cardiac arrest. N Engl J Med. 2013;368:680–681. [DOI] [PubMed] [Google Scholar]
- 4. Brady WJ, Gurka KK, Mehring B, Peberdy MA, O'Connor RE. In‐hospital cardiac arrest: impact of monitoring and witnessed event on patient survival and neurologic status at hospital discharge. Resuscitation. 2011;82:845–852. [DOI] [PubMed] [Google Scholar]
- 5. Kutsogiannis DJ, Bagshaw SM, Laing B, Brindley PG. Predictors of survival after cardiac or respiratory arrest in critical care units. CMAJ. 2011;183:1589–1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Morrison LJ, Neumar RW, Zimmerman JL, Link MS, Newby LK, McMullan PWJr, Hoek TV, Halverson CC, Doering L, Peberdy MA, Edelson DP; American Heart Association Emergency Cardiovascular Care Committee, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Cardiovascular and Stroke Nursing . Strategies for improving survival after in‐hospital cardiac arrest in the United States: 2013 consensus recommendations: a consensus statement from the American Heart Association. Circulation. 2013;127:1538–1563. [DOI] [PubMed] [Google Scholar]
- 7. Tian J, Kaufman DA, Zarich S, Chan PS, Ong P, Amoateng‐Adjepong Y, Manthous CA; American Heart Association National Registry for Cardiopulmonary Resuscitation Investigators . Outcomes of critically ill patients who received cardiopulmonary resuscitation. Am J Respir Crit Care Med. 2010;182:501–506. [DOI] [PubMed] [Google Scholar]
- 8. Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, Berg RA, Nichol G, Lane‐Trultt T. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. [DOI] [PubMed] [Google Scholar]
- 9. Szklo M, Nieto J. Epidemiology: Beyond the Basics. Burlington, MA: Jones and Bartlett Publishers; 2014. [Google Scholar]
- 10. Sandroni C, Nolan J, Cavallaro F, Antonelli M. In‐hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007;33:237–245. [DOI] [PubMed] [Google Scholar]
- 11. Sandroni C, Ferro G, Santangelo S, Tortora F, Mistura L, Cavallaro F, Caricato A, Antonelli M. In‐hospital cardiac arrest: survival depends mainly on the effectiveness of the emergency response. Resuscitation. 2004;62:291–297. [DOI] [PubMed] [Google Scholar]
- 12. Tunstall‐Pedoe H, Bailey L, Chamberlain DA, Marsden AK, Ward ME, Zideman DA. Survey of 3765 cardiopulmonary resuscitations in British hospitals (the BRESUS Study): methods and overall results. BMJ. 1992;304:1347–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dumot JA, Burval DJ, Sprung J, Walters JH, Mraovic B, Karafa MT, Mascha EJ, Bourke DL. Outcome of adult cardiopulmonary resuscitations at a tertiary referral center including results of “limited” resuscitations. Arch Intern Med. 2001;161:1751–1758. [DOI] [PubMed] [Google Scholar]
- 14. Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, Harris M. Nurse staffing and inpatient hospital mortality. N Engl J Med. 2011;364:1037–1045. [DOI] [PubMed] [Google Scholar]
- 15. Truog RD, Cist AF, Brackett SE, Burns JP, Curley MA, Danis M, DeVIta MA, Rosenbaum SH, Rothenberg DM, Sprung CL, Webb SA, Wlody GS, Hurford WE. Recommendations for end‐of‐life care in the intensive care unit: the Ethics Committee of the Society of Critical Care Medicine. Crit Care Med. 2001;29:2332–2348. [DOI] [PubMed] [Google Scholar]
- 16. The Joint Commission's Annual Report on Quality and Safety. 2008. Available at: http://www.jointcommissionreport.org. Accessed August 26, 2016.
- 17. Chan PS. Rapid response teams. Arch Intern Med. 2010;170:18. [DOI] [PubMed] [Google Scholar]
- 18. Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS; American Heart Association Get with the Guidelines‐Resuscitation Investigators . Trends in survival after in‐hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients. JAMA. 2002;288:2151. [DOI] [PubMed] [Google Scholar]


