Abstract
Background:
Although the effect of cardiac rehabilitation (CR) on cardiovascular disease (CVD) prognosis has been well-documented by several systematic reviews, none have focused on the effect of CR on metabolic syndrome (MetS) and its related components. Therefore, the present systematic review and meta-analysis was conducted to assess the effect of CR on MetS and its components.
Materials and Methods:
PubMed, SCOPUS, Cochrane library, and Google Scholar database were searched up to February 2014 with no date and language restrictions. The random effects model was used to assess the overall effect of CR on MetS prevalence and the change in metabolic or anthropometric measures.
Results:
Fifteen studies with 19,324 subjects were included in the present systematic review and meta-analysis. Our analysis showed that the CR could significantly reduce MetS prevalence [reduction rate: 0.25, 95% confidence interval (CI): 0.21, 0.3, P value <0.001; P value for heterogeneity <0.001, I-squared: 86.2%]. Additionally, results showed the protective role of CR on all MetS components including high density lipoprotein cholesterol [mean difference (MD): 2.13 mg/dL, 95% CI: 1.17, 3.1], triglyceride (MD: -27.45 mg/dL, 95% CI: −36.92, −17.98), systolic blood pressure (SBP) (MD: −6.20 mmHg, 95% CI: -8.41, −3.99), diastolic blood pressure (DBP) (MD: −2.53 mmHg, 95% CI: −3.64, −1.41), fasting blood sugar (FBS) (MD: −6.42 mg/dL, 95% CI: −6.85, −5.99), and waist circumference (WC) (MD: −2.25 cm, 95% CI: −3.15, −1.35).
Conclusion:
CR has resulted in improvement in MetS and its entire components, and could be considered as a useful tool for MetS patients, especially among those with CVD.
Keywords: Cardiac rehabilitation (CR), meta-analysis, metabolic factors, syndrome x
INTRODUCTION
Metabolic syndrome (MetS), also called syndrome X, is a cluster of metabolic factors including hypertension, dyslipidemia, abdominal obesity, and impaired plasma glucose, which are highly related to cardiovascular disease (CVD).[1] There are several definitions for MetS but their parameters are generally the same and have some slight differences. Three widely used definitions are those proposed by the World Health Organization (WHO),[2] the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III),[3] and the International Diabetes Federation (IDF).[4] According to Adult Treatment Panel III (ATP III) criteria, one-third of overweight and obese people in the United States have MetS.[5] Today, the increase in its prevalence as a result of the increased prevalence of obesity and sedentary lifestyle has been well-documented, especially in older adults.[6] Moreover, the prevalence of MetS in cardiac rehabilitation (CR) program is estimated to be 48-58%, which is more than twice the prevalence in the general population[5,7] and it is proposed that the MetS among coronary heart disease (CHD) patients is associated with higher rates of morbidity and mortality.[1,8,9]
The first-line management in individuals with the MetS is lifestyle modification.[10] One of the core components of lifestyle modification is physical activity, which is the most important part of CR program for patients with CVDs too.[10,11,12,13] CR is a complex interventional therapy, which is defined as “comprehensive long-term services involving medical evaluation, prescribed exercise, cardiac risk-factor modification, health education, counseling, and behavioral interventions” by the U.S. Department of Health and Human Services and the National Heart, Lung, and Blood Institute.[14,15] As it is well-documented that exercise training and diet at least partly reverse MetS,[10] it would be useful to determine the efficacy of CR on MetS patients too. Although various studies were conducted to test the effect of CR on MetS patients, there are still inconsistent results on the effect of CR on reverse MetS and also its components. For instance, although several studies have failed to find any significant effect of CR on high density lipoprotein cholesterol (HDL-C),[16,17,18] some others have even documented its significant effects on HDL-C.[19,20,21,22] The same pattern can be observed in other metabolic factors too.[16,17,18,19,20,21,22,23,24,25,26,27,28,29,30] Therefore, the present article aimed to summarize and if possible, perform a meta-analysis on published data about the effect of CR on MetS reduction rate and its components or related metabolic and anthropometric markers.
MATERIALS AND METHODS
Search strategy
PubMed, SCOPUS, Cochrane library, and Google Scholar were searched up to February 2014 without any language or date restrictions. The search strategy was developed to maximize sensitivity of article identification and we used both terms selected from medical subject headings (MeSH) and non-MeSH terms including MetS X, MetS, syndrome x, insulin resistance, metabolic diseases in combination with CR, cardiovascular rehabilitation, cardiopulmonary rehabilitation, cardiac exercise, cardiovascular exercise, cardiopulmonary exercise, rehabilitation, and cardiac rehabilitation. Additional eligible studies were sought by a hand search of reference lists from primary articles, which were found to be related to the topic.
Inclusion criteria
We included (a) interventional studies investigating the effect of CR (a supervised group-based program undertaken in a hospital or community setting such as a sports center.) (b) interventional studies conducted in adults (>18 years) with MetS (according to ATP III definitions or other guidelines); (c) interventional studies where at least one of the following outcome measures were assessed before and after CR: number of MetS patients, fasting blood sugar (FBS), total cholesterol (TC), triglyceride (TG), low density lipoprotein cholesterol (LDL-C), HDL-C, systolic blood pressure (SBP) and diastolic blood pressure (DBP), body mass index (BMI), and waist circumference (WC). Titles and if needed, abstracts of retrieved articles were separately screened by two authors for their eligibility (ZK and MS) and disagreements were resolved by discussion with a third author (ASA).
Data extraction
The information including the first author's name, year of publication, country of origin, MetS definition, prenumber and postnumber of MetS patients, and metabolic/anthropometric factors were extracted. Data were extracted by a single reviewer (ZK) and checked by a second reviewer (ASA). Moreover, we contacted the authors of the included articles for additional unpublished data or clarification of data[18,21,26] when necessary to ensure that all related articles were represented in the meta-analysis.
Statistical analysis
The change in mean (difference in means) cardiometabolic factors including FBS, TC, TG, LDL-C, HDL-C, SBP, DBP, BMI, and WC and their corresponding standard errors (SEs) were calculated based on the reported pre- and post-CR data and used as effect size. To calculate the mean changes and their corresponding standard deviations (SDs) for articles, which did not provide these data, we computed the correlation coefficient using articles that reported changes in the mean and SD of metabolic factors.[18,21] Furthermore, the MetS reduction rate was calculated from pre- and post-CR prevalence in each study of MetS as an effect size to be included in the meta-analysis. Summary mean estimates with their corresponding SDs were derived by the method explained by DerSimonian and Laird[31] using random effects model, taking between-studies variability into account. Statistical heterogeneity between studies was evaluated with Cochran's Q test and I-squared (I-squared more than 25% was considered as high heterogeneity).[32] Additionally, we performed a simple meta-regression analysis to investigate whether the heterogeneity found between studies was related to changes in WC. Subgroup analysis was also incorporated to check for the possible sources of between-studies heterogeneity.[32] Sensitivity analysis was also performed to explore the extent to which inferences might depend on a particular study or group of studies. Publication bias was assessed by visual inspection of funnel plots[33] and statistical assessment of asymmetry was done with Egger's regression asymmetry test and Begg's adjusted rank correlation test.[34] All statistical analyses were carried out by the use of Stata, version 11.2 (StataCorp, College Station, TX, USA). P values <0.05 were considered statistically significant.
RESULTS
Our preliminary online search retrieved 1,200 studies, about 1,175 were excluded after reading titles or abstracts because they did not met our inclusion criteria [Figure 1]. Finally, 15 articles were eligible to be included in the current systematic review (seven conducted in the US,[16,18,19,22,24,27,29] three in Canada,[23,25,30] two in Europe,[20,26] and three in Asia[17,21,28]). In total, these studies included 19,324 MetS patients and the number of participants ranged from 32 to 15,819. The ATP III criteria[3] were used in nine studies,[16,17,20,21,22,24,25,30] whereas harmonized criteria[35] were used in two studies;[18,23] the International Diabetes Federation (IDF) criteria[4] were used only in one study[26] and three studies did not report their definitions.[19,28,29] The duration of studies was from 4 weeks to 59 weeks. Table 1 provides detailed information about included studies.
Figure 1.
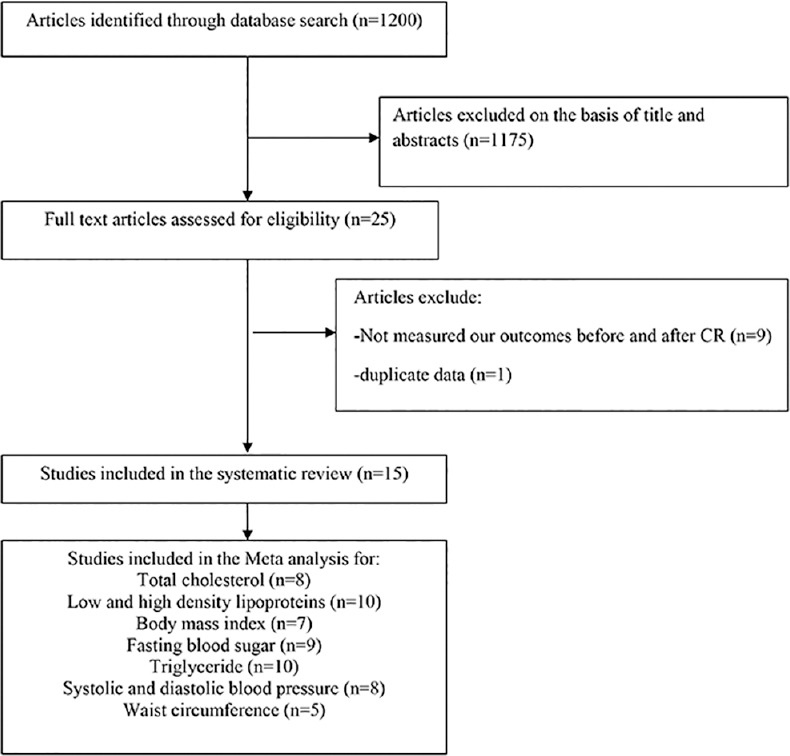
Summary of study selection process
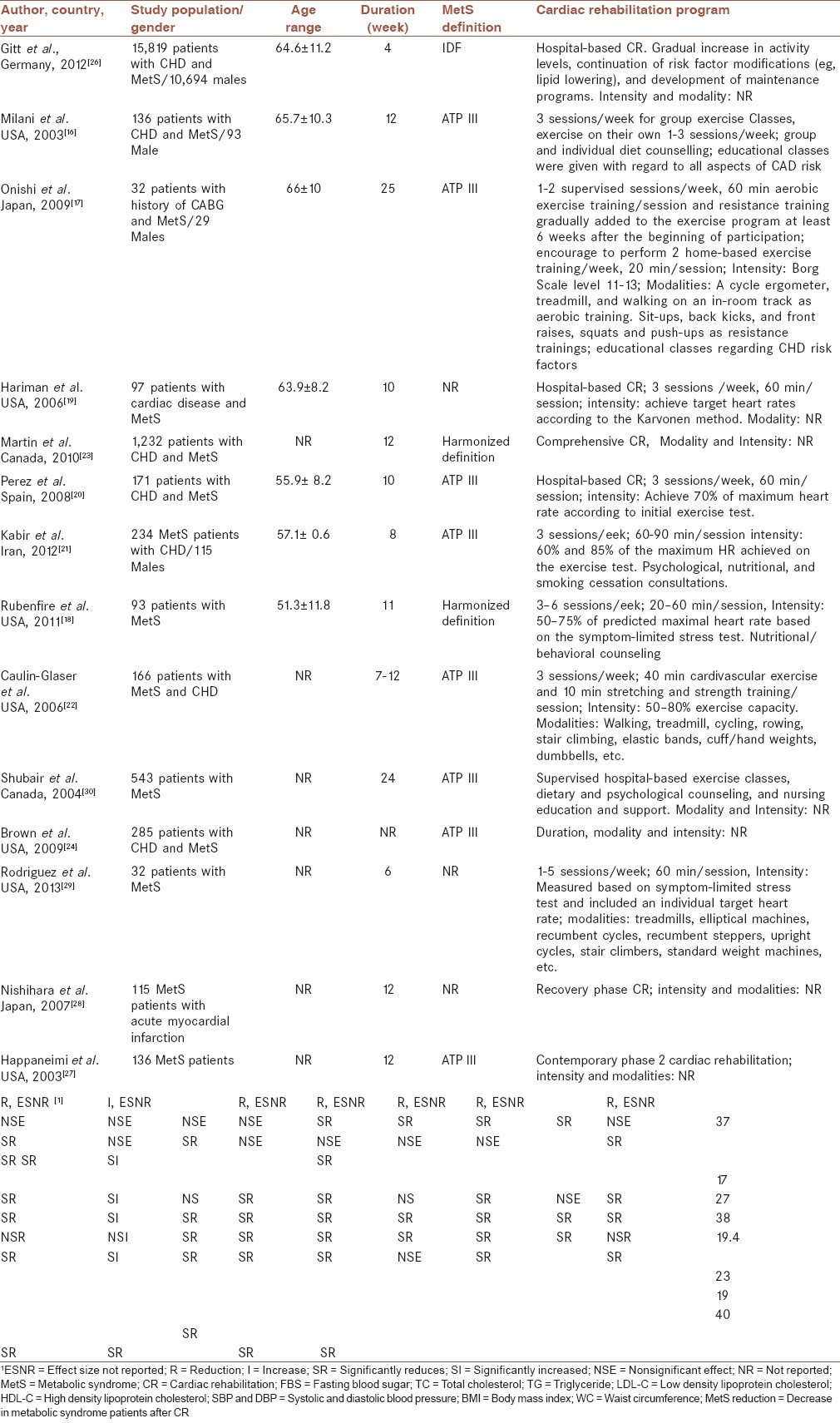
Table 1.
Characteristics of studies evaluated the effect of CR on metabolic syndrome and/or its components
Results from meta-analysis
Effect of cardiac rehabilitation on metabolic syndrome recovery
Eight studies[16,18,20,21,23,24,25,30] with 2,866 subjects evaluated the effect of the CR on the recovery from MetS by reporting the decrement in MetS prevalence. We found a significant effect of CR on decreasing MetS prevalence in the whole data set [prevalence reduction (95% CI): 0.25 (0.21, 0.3), P value <0.001; P value for heterogeneity <0.001, I-squared: 86.2%]; subgroup analysis based on duration of CR (duration <10 week as short term and duration >10 weeks as long term) showed that short-term CR administration results in a greater reduction in MetS prevalence than long-term CR [prevalence reduction rate (95% CI): 0.34 (0.26, 0.43), P value < 0.001and prevalence reduction rate (95% CI): 0.24 (0.18, 0.29), P < 0.001,respectively] [Figure 2]. The study by Brown et al.[24] did not provide the duration of CR; so we could not classify this study based on duration. There was no evidence of publication bias using Egger's and Begg's asymmetry tests (P for bias = 0.602 and 0.938, respectively). Sensitivity analysis could not show considerable change regarding the effect of CR on MetS prevalence after excluding any of included studies.
Figure 2.
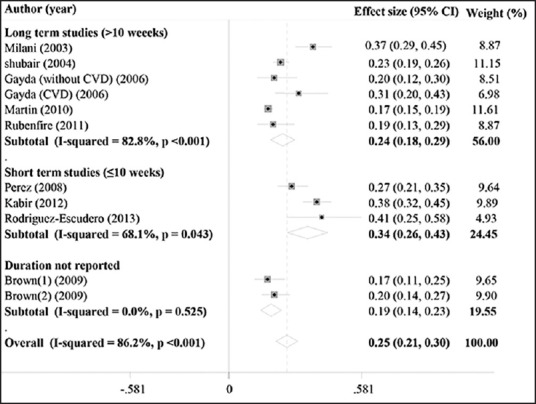
Forest plot of studies that evaluated the effect of CR on the prevalence reduction of MetS and subgroup analysis based on CR duration; long-term CR (>10 weeks), short-term CR (≤10 weeks); squares and diamonds represent effect size; horizontal lines show 95% confidence intervals (CIs)
Effect of cardiac rehabilitation on metabolic factors
The result of the overall effect and short-term effect versus long-term effect of CR on metabolic factors are summarized in Table 2.
Table 2.
Meta-analysis results for the effect of cardiac rehabilitation (CR) on metabolic factors
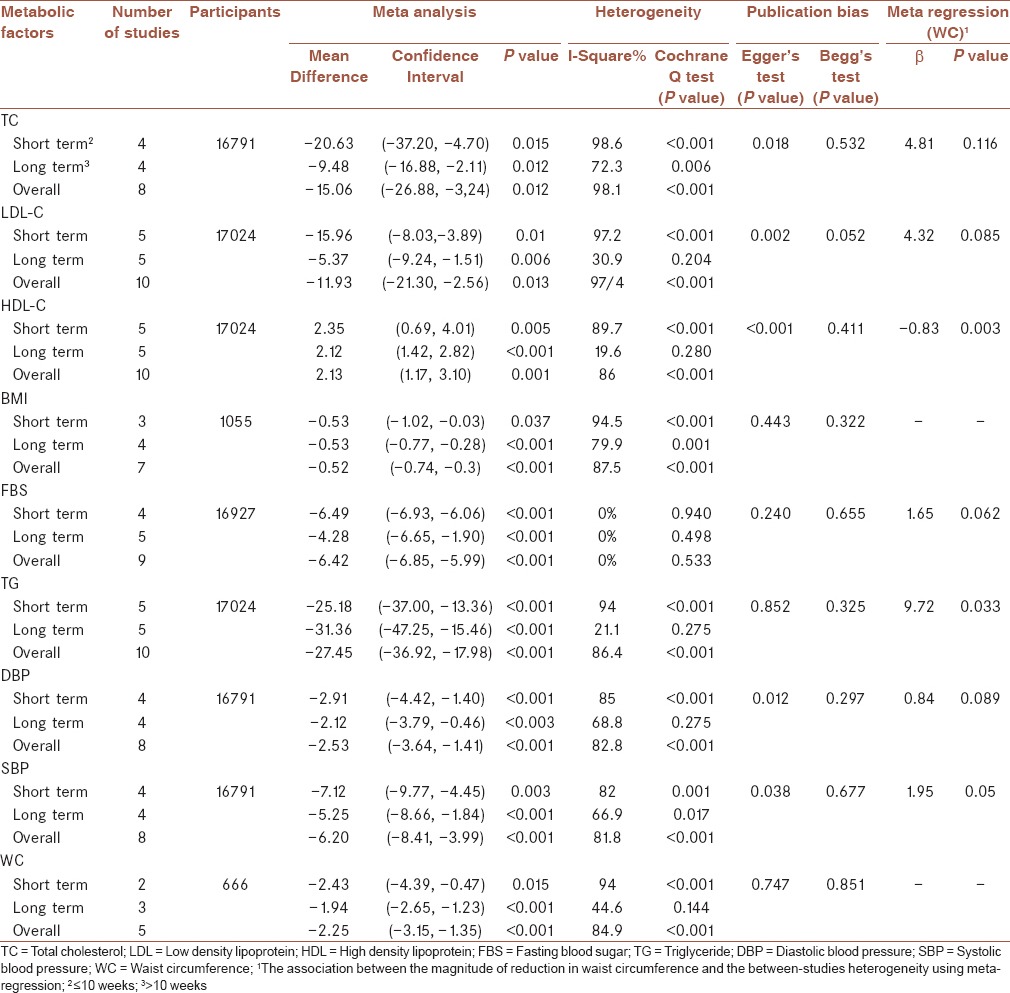
Lipid profile
Ten studies[16,17,18,19,20,21,22,25,26,27] with 17,024 subjects evaluated the effect of CR on LDL-C, HDL-C, and TG, and 8 studies[16,17,18,20,21,22,25,26] with 16,791 subjects evaluated the role of CR on TC. CR resulted in a significant reduction in TC, LDL-C, and TG and a significant increase in the mean HDL-C levels. Subgroup analysis based on the study period showed that administered short-term CR had resulted in a greater reduction in TC and LDL-C, and a greater increase in HDL-C compared to long-term CR [Table 2]. In contrast, long-term CR had resulted in greater reduction in serum TG than short-term CR.
Blood pressure
Eight studies[16,17,18,20,21,22,25,26] with 16,791 subjectsexamined the effect of CR on SBP and DBP in MetS patients. Our meta-analysis showed that CR resulted in a significant reduction in both the mean SBP and DBP levels. Subgroup analysis based on the study period showed that effect of short-term CR on SBP and DBP had resulted in a greater reduction than long-term CR [Table 2].
Fasting blood sugar
Nine studies[16,17,18,20,21,22,25,26,27] with 16,791 subjects evaluated the role of CR on FBS. Overall, a meta-analysis showed the beneficial effect of CR on FBS levels. When the subgroup analysis was performed based on the duration of CR, we observed that short-term CR was associated with a greater reduction in FBS as compared with long-term CR [Table 2].
Body mass index
Seven studies[16,18,20,21,22,25,28] with 1,055 participants were included in the meta-analysis. We found a significant effect of CR on decreasing BMI. Subgroup analysis based on CR duration showed that effect of CR on BMI was not different in short-term CR as compared with long-term CR [Table 2].
Waist circumference
Five studies[16,17,18,20,21] with 666 subjectsexamined the effect of CR on WC. Meta-analysis showed that CR resulted in a significant reduction in mean WC. When the subgroup analysis was performed based on duration of CR, we observed that short-term CR was associated with a greater reduction in WC as compared with long-term CR [Table 2].
Association between waist circumference and metabolic syndrome components
The result of the meta regression showed that the decrease in WC was significantly associated with decrease in LDL, SBP, DBP, FBS, and TG and a significant increase in HDL but a nonsignificant trend was found for the association of WC with TC [Table 2].
Publication bias and sensitivity analysis for studies, which explored the effect of cardiac rehabilitation on metabolic markers
We did not find any evidence of publication bias for studies assessing the effect of CR on TG, WC, and BMI [Table 2]. With regard to TC, HDL, LDL, SBP, and DBP, we reached a significant publication bias by Egger's test (P = 0.018, P < 0.001, P = 0.002, P = 0.038, and P = 0.012, respectively); however, this was not verified by Begg's test (P = 0.532, P = 0.411, P = 0.052, P = 0.677, and P = 0.297, respectively). Sensitivity analysis showed that the effect of CR on all metabolic factors (lipid profile, FBS, BP, BMI, and WC) did not substantially modify by removing the result of a certain study.
DISCUSSION
The present systematic review and meta-analysis could provide evidences about the favorable effect of CR with regard to not only MetS but also its entire individual components and related metabolic or anthropometric markers. Based on our results, adherence to CR can result in 25% decrease in the proportion of MetS patients. Moreover, short-term CR (≤10 weeks) might result in a greater reduction in MetS prevalence (about 34%), TC, LDL-C, FBS, DBP, SBP, WC, and greater increase in HDL-C as compared with long-term CR. On the other hand, effect of CR (>10 weeks) on TG was shown to be greater in long-term period than short-term CR. The role of different components of CR from exercise to diet and consultation among MetS patients are investigated separately in various studies but to the best of our knowledge, this is the first meta-analysis that has examined the effect of CR on patients with CVDs and MetS.
CR is one of the most known and well-studied interventions, which has been shown to be associated with decreased morbidity and mortality of CVD,[36] On the other hand, MetS among CVD patients is associated with higher risk of mortality and morbidity.[37] Exercise and diet are perceived not only as the key components of the treatment and prevention strategies in patients with MetS or CVD[10,38,39] but also as essential parts of CR.[11] According to a systematic review done by Pattyn et al., there is a beneficial effect of the dynamic endurance exercise on individual components of MetS, namely, WC, HDL-C, LDL-C, SBP, DBP, and BMI but exercise has no significant effect on TG and FBS.[38] Additionally, results from a meta-analysis on the Mediterranean diet among MetS patients showed a beneficial effect of diet on HDL-C, TG, WC, SBP, DBP, and glucose.[40] Moreover the result of a recent meta-analysis performed by Yamaoka and Tango revealed the favorable effect of lifestyle modification (diet and exercise/diet consultation) on all components of MetS except HDL.[10] Taken together, each of these studies indicate the beneficial effect of different components of CR on several metabolic factors but not on all factors, which is achievable by the implication of CR as indicated in our meta-analysis.
At present, the prevalence of MetS has dramatically increased parallel to obesity[6] and as it is well-known that abdominal obesity is one of the most important factors related to MetS and also the appearance of its individual components because of its major role in glucose and lipid metabolism.[41,42] The present meta-analysis also indicates that a decrease in WC is significantly associated with improvement in most components of MetS including LDL-C, HDL-C, TG, blood pressure (BP), and FBS. In line with our study, a decrease in WC is associated with increase in HDL-C and decrease in DBP in a meta-analysis done by Pattyn et al.[38] Therefore, our result may show that the effect of CR on WC may be the cause of its favorable effect on other MetS components.
Although the significant effect of CR on MetS and its related markers was shown in short- and long-term studies, we found that short-term CR resulted in greater effects on MetS and all its components except for TG compared with long-term CR. However, the included studies did not mention the prevalence of adherence to CR; the result may be related to a decrease in adherence to CR in long-term interventions[43] and as Dimatteo et al. mentioned in their meta-analysis, poor adherence to treatment may cause an impact on clinical outcome.[44]
Certain limitations of this study should be considered while interpreting our results. First, MetS has several definitions and due to the small number of study groups and inadequate data, a subgroup analysis based on definition was not possible. However, this may be acceptable because the parameters of its different definitions are generally the same. Second, none of our included studies had control MetS subjects for whom the CR was not implemented. Finally, some subgroup analysis such as sex-based differences due to inadequate data could not be performed.
CONCLUSION
In conclusion, CR can be considered as a treatment tool in MetS patients, especially for those with CVDs. Although short-term CR is associated with greater improvement in most MetS components and MetS prevalence as compared to long-term CR, effect of long-term CR remains significant for MetS reduction rate and all its related metabolic or anthropometric factors. Regarding thefavorable effect of CR on cardiometabolic components in MetS patients, further studies are required to investigate whether CR can affect the long-term prognosis of this group of patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
AUTHOR'S CONTRIBUTION
MS contributed in the conception and design of the work, drafting and revising the draft, conducting the study, approving the final version of the manuscript, and agreed with all aspects of the work.
AS-A contributed in the conception of the work, revising the draft, analyzing and interpreting of data, approving the final version of the manuscript, and agreed with all aspects of the work.
ZK contributed in the conception of the work, drafting and revising the draft, data acquisition, approving the final version of the manuscript, and agreed with all aspects of the work.
HS-K contributed in the conception of the work, data acquisition, approving the final version of the manuscript, and agreed with all aspects of the work.
RH contributed in the conception of the work, conducting the study, approving the final version of the manuscript, and agreed with all aspects of the work.
HR contributed in the conception and design of the work, conducting the study, drafting the draft, approving the final version of the manuscript, and agreed with all aspects of the work.
REFERENCES
- 1.Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–28. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- 2.Consultation W. Geneva, Switzerland: World Health Organization; 1999. Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications; pp. 1–59. [Google Scholar]
- 3.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of The National Cholesterol Education Program (NCEP) Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 4.Alberti G, Zimmet P, Shaw J, Grundy S. International Diabetes Federation 2006: The IDF consensus worldwide definition of the metabolic syndrome. [Last accessed on 2015 Aug 25]. Available from http://www.idf.org/webdata/docs/IDF_Meta_def_final.pdf .
- 5.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: Findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–9. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 6.Zimmet P, Alberti K, Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001;414:782–7. doi: 10.1038/414782a. [DOI] [PubMed] [Google Scholar]
- 7.Savage PD, Banzer JA, Balady GJ, Ades PA. Prevalence of metabolic syndrome in cardiac rehabilitation/secondary prevention programs. Am Heart J. 2005;149:627–31. doi: 10.1016/j.ahj.2004.07.037. [DOI] [PubMed] [Google Scholar]
- 8.Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–16. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 9.Cameron AJ, Shaw JE, Zimmet PZ. The metabolic syndrome: Prevalence in worldwide populations. Endocrinol Metab Clin North Am. 2004;33:351–75. doi: 10.1016/j.ecl.2004.03.005. table of contents. [DOI] [PubMed] [Google Scholar]
- 10.Yamaoka K, Tango T. Effects of lifestyle modification on metabolic syndrome: A systematic review and meta-analysis. BMC Med. 2012;10:138. doi: 10.1186/1741-7015-10-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Balady GJ, Williams MA, Ades PA, Bittner V, Comoss P, Foody JM, et al. American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; American Heart Association Council on Cardiovascular Nursing; American Heart Association Council on Epidemiology and Prevention; American Heart Association Council on Nutrition, Physical Activity, and Metabolism; American Association of Cardiovascular and Pulmonary Rehabilitation. Core Components of Cardiac Rehabilitation/Secondary Prevention Programs: 2007 Update: A Scientific Statement From the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2007;115:2675–82. doi: 10.1161/CIRCULATIONAHA.106.180945. [DOI] [PubMed] [Google Scholar]
- 12.Basati F, Sadeghi M, Kargarfard M, Yazdekhasti S, Golabchi A. Effects of a cardiac rehabilitation program on systolic function and left ventricular mass in patients after myocardial infarction and revascularization. J Res Med Sci. 2012;17:S28–32. [Google Scholar]
- 13.Golabchi A, Basati F, Kargarfard M, Sadeghi M. Can cardiac rehabilitation programs improve functional capacity and left ventricular diastolic function in patients with mechanical reperfusion after ST elevation myocardial infarction? A double-blind clinical trial. ARYA Atheroscler. 2012;8:125–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Wenger NK, Froelicher ES, Smith L, Ades PA, Berra K, Blumenthal JA, et al. Rockville, MD: US Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, and the National Heart, Lung, and Blood Institute AHCPR Publication; 1995. Cardiac Rehabilitation. Clinical Practice Guideline No. 17. [PubMed] [Google Scholar]
- 15.Mostafavi F, Ghofranipour F, Feizi A, Pirzadeh A. Improving physical activity and metabolic syndrome indicators in women: A transtheoretical model-based intervention. Int J Prev Med. 2015;6:28. doi: 10.4103/2008-7802.154382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Milani RV, Lavie CJ. Prevalence and profile of metabolic syndrome in patients following acute coronary events and effects of therapeutic lifestyle change with cardiac rehabilitation. Am J Cardiol. 2003;92:50–4. doi: 10.1016/s0002-9149(03)00464-8. [DOI] [PubMed] [Google Scholar]
- 17.Onishi T, Shimada K, Sunayama S, Ohmura H, Sumide T, Masaki Y, et al. Effects of cardiac rehabilitation in patients with metabolic syndrome after coronary artery bypass grafting. J Cardiol. 2009;53:381–7. doi: 10.1016/j.jjcc.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 18.Rubenfire M, Mollo L, Krishnan S, Finkel S, Weintraub M, Gracik T, et al. The metabolic fitness program: Lifestyle modification for the metabolic syndrome using the resources of cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2011;31:282–9. doi: 10.1097/HCR.0b013e318220a7eb. [DOI] [PubMed] [Google Scholar]
- 19.Hariman LM, Stachowiak A, Zajeski S, Hariman RJ. PR_026: Does Cardiac Rehabilitation Improve the Cardiac Profile of Patients With Metabolic Syndrome? Arch Phys Med Rehabil. 2006;87:e9. [Google Scholar]
- 20.Pérez IP, Zapata MA, Cervantes CE, Jarabo RM, Grande C, Plaza R, et al. Cardiac rehabilitation programs improve metabolic parameters in patients with the metabolic syndrome and coronary heart disease. J Clin Hypertens (Greenwich) 2010;12:374–9. doi: 10.1111/j.1751-7176.2009.00259.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kabir A, Sarrafzadegan N, Amini A, Aryan RS, Kerahroodi FH, Rabiei K, et al. Impact of cardiac rehabilitation on metabolic syndrome in Iranian patients with coronary heart disease: The role of obesity. Rehabil Nurs. 2012;37:66–73. doi: 10.1002/RNJ.00012. [DOI] [PubMed] [Google Scholar]
- 22.Caulin-Glaser T, Falko JM. Effects of cardiac rehabilitation on lipoprotein abnormalities in patients with Type 2 diabetes mellitus and metabolic syndrome. Future Lipidol. 2006;1:65–73. [Google Scholar]
- 23.Martin BJ, Arena R, Hauer T, Austford LD, Aggarwal S, Stone JA. The prognostic importance of metabolic syndrome in a large cardiac rehabilitation cohort. Circulation. 2011;124:A13818. [Google Scholar]
- 24.Brown TM, Sanderson BK, Bittner V. Drugs are not enough: The metabolic syndrome — A call for intensive therapeutic lifestyle change. J Cardiometab Syndr. 2009;4:20–5. doi: 10.1111/j.1559-4572.2008.00031.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gayda M, Brun C, Juneau M, Levesque S, Nigam A. Long-term cardiac rehabilitation and exercise training programs improve metabolic parameters in metabolic syndrome patients with and without coronary heart disease. Nutr Metab Cardiovasc Dis. 2008;18:142–51. doi: 10.1016/j.numecd.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 26.Gitt A, Jannowitz C, Karoff M, Karmann B, Horack M, Völler H. Treatment patterns and risk factor control in patients with and without metabolic syndrome in cardiac rehabilitation. Vasc Health Risk Manag. 2012;8:265–74. doi: 10.2147/VHRM.S28949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haapaniemi SS, Bonzheim KA, Franklin BA, Salmon RD, Gordon NF. Clinical effectiveness of a contemporary cardiac rehabilitation program in patients with the metabolic syndrome. Med Sci Sport Exer. 2003;35(Suppl 1):S233. [Google Scholar]
- 28.Nishihira M, Higo T, Noguchi T, Kawakami R, Aihara N, Ohara T, et al. PJ-117 is there any difference in the effects of cardiac rehabilitation between post-myocardial infarction patients with and without metabolic syndrome? (Exercise test/Cardiac rehabilitation-6, The 71st Annual Scientific Meeting of the Japanese Circulation Society. Circ J. 2007;71:500–1. [Google Scholar]
- 29.Rodriguez-Escudero JP, Somers VK, Heath AL, Thomas RJ, Squires RW, Sochor O, et al. Effect of a lifestyle therapy program using cardiac rehabilitation resources on metabolic syndrome components. J Cardiopulm Rehabil Prev. 2013;33:360–70. doi: 10.1097/HCR.0b013e3182a52762. [DOI] [PubMed] [Google Scholar]
- 30.Shubair MM, Kodis J, McKelvie RS, Arthur HM, Sharma AM. Metabolic profile and exercise capacity outcomes: Their relationship to overweight and obesity in a Canadian cardiac rehabilitation setting. J Cardiopulm Rehabil. 2004;24:405–13. doi: 10.1097/00008483-200411000-00008. [DOI] [PubMed] [Google Scholar]
- 31.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 32.Higgins J, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 33.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sterne JA, Egger M, Smith GD. Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ. 2001;323:101–5. doi: 10.1136/bmj.323.7304.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. International Diabetes Federation Task Force on Epidemiology and Prevention; Hational Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: A joint interim statement of the international diabetes federation task force on epidemiology and prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 36.Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, et al. Exercise-based rehabilitation for patients with coronary heart disease: Systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116:682–92. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 37.Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, et al. Metabolic Syndrome and risk of incident cardiovascular events and death: A systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007;49:403–14. doi: 10.1016/j.jacc.2006.09.032. [DOI] [PubMed] [Google Scholar]
- 38.Pattyn N, Cornelissen VA, Eshghi SR, Vanhees L. The effect of exercise on the cardiovascular risk factors constituting the metabolic syndrome: A meta-analysis of controlled trials. Sports Med. 2013;43:121–33. doi: 10.1007/s40279-012-0003-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rees K, Dyakova M, Ward K, Thorogood M, Brunner E. Dietary advice for reducing cardiovascular risk. Cochrane Database Syst Rev. 2013;3:CD002128. doi: 10.1002/14651858.CD002128.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kastorini CM, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB. The effect of Mediterranean diet on metabolic syndrome and its components: A meta-analysis of 50 studies and 534,906 individuals. J Am Coll Cardiol. 2011;57:1299–313. doi: 10.1016/j.jacc.2010.09.073. [DOI] [PubMed] [Google Scholar]
- 41.Hajer GR, van Haeften TW, Visseren FL. Adipose tissue dysfunction in obesity, diabetes, and vascular diseases. Eur Heart J. 2008;29:2959–71. doi: 10.1093/eurheartj/ehn387. [DOI] [PubMed] [Google Scholar]
- 42.Sadeghi M, Ghashghaei FE, Rabiei K, Golabchi A, Noori F, Baboli MT, et al. Does significant weight reduction in men with coronary artery disease manage risk factors after cardiac rehabilitation program? J Res Med Sci. 2013;18:956–60. [PMC free article] [PubMed] [Google Scholar]
- 43.Sluijs E, Knibbe J. Patient compliance with exercise: Different theoretical approaches to short-term and long-term compliance. Patient Educ Couns. 1991;17:191–204. [Google Scholar]
- 44.Dimatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: A meta-analysis. Med Care. 2002;40:794–811. doi: 10.1097/00005650-200209000-00009. [DOI] [PubMed] [Google Scholar]


