Abstract
Background
Low socioeconomic status (SES) is a known risk factor for heart failure, mortality among those with heart failure, and poor post heart transplant (HT) outcomes. This study sought to determine if SES is associated with decreased waitlist survival while on LVAD support and after HT.
Methods and Results
3,361 adult patients bridged to primary HT with an LVAD between May 2004 and April 2014 were identified in the UNOS database. SES was measured using the AHRQ SES index using data from the 2014 American Community Survey. In the study cohort, SES did not have an association with the combined endpoint of death or delisting on LVAD support (p=0.30). In a cause-specific unadjusted model, those in the top (HR 1.55, 95% CI 1.14–2.11, p=0.005) and second greatest SES quartile (HR 1.50, 95% CI 1.10–2.04, p=0.01) had an increased risk of death on device support compared to the lowest SES quartile. Adjusting for clinical risk factors mitigated the increased risk. There was no association between SES and complications. Post-HT survival, both crude and adjusted, was decreased for patients in the lowest quartile of SES index compared to all other SES quartiles.
Conclusions
Freedom from waitlist death or delisting was not impacted by SES. Patients with a higher SES had an increased unadjusted risk of waitlist mortality during LVAD support, which was mitigated by adjusting for increased comorbid conditions. Low SES was associated with worse post-HT outcomes. Further study is needed to confirm and understand a differential effect of SES on post-transplant outcomes that was not seen during LVAD support prior to HT.
Keywords: transplantation, heart failure, left ventricular assist device, socioeconomic position
Socioeconomic status (SES) has been identified as a risk factor for heart failure,1 hospital readmission,2, 3 and mortality.1, 2 Among patients who progress to Stage D heart failure, both heart transplantation and left ventricular assist devices (LVAD) provide improved quality of life and survival. Previous studies have identified race4, 5 and SES6 as a risk factor for decreased post-transplant survival in adults and children respectively. Similarly, low SES has been shown to be associated with increased risk of rejection and graft loss after transplantation.7, 8 One single-center study suggested that among patients bridged to transplantation (BTT) with an LVAD, low median household income was the only predictor of death or readmission.9 A 136 patient single-center study investigated at the impact of psychosocial determinants on LVAD patients found no impact on mortality, but found current drug use, depression, and paradoxically not currently smoking to increase the risk of readmission in destination therapy LVAD patients.10 This study sought to determine if SES and its determinants are associated with decreased survival while on LVAD support and after HT.
Methods
The United Network for Organ Sharing (UNOS) database was analyzed for patients bridged to transplantation with a continuous-flow LVAD (CF-LVAD) between May 2004 and April 2014. Follow-up data was collected through June 2014. Adult candidates (age ≥18 years) registered for a single organ primary heart transplant who received a Food and Drug Administration (FDA) approved CF-LVAD were included. Devices were limited to the Heartmate II (Thoratec/St. Jude, Pleasanton, CA) and Heartware HVAD (Heartware, Framingham, MA). Patients who required temporary left sided mechanical circulatory support, BiVAD, or total artificial heart were excluded from the analysis. The primary endpoint was freedom from death or delisting while on LVAD support. Secondary endpoints included death while on LVAD support, delisting while on LVAD support, complications (thromboembolism, device infection, device malfunction, or life-threatening ventricular arrhythmia) requiring UNOS listing status upgrade, and post-transplant survival. BTT was the ultimate strategy for all patients.
Socioeconomic status was measured using the Agency for Healthcare Research and Quality (AHRQ) SES index. The AHRQ SES index is a measure of neighborhood SES and was generated using the following Zip-code level Census variables: percentage of people in the labor force who are unemployed, percentage of people living below poverty level, median household income, median value of owner-occupied dwellings, percentage of people ≥25 years of age with less than a 12th-grade education, percentage of people ≥25 years of age completing ≥4 years of college, and percentage of households that average ≥1 people per room. (Supplemental Material)11. The SES index for this study was calculated using data from the 2014 American Community Survey and has been previously used.12–14 The study was submitted to the Institutional Review Board of Columbia University Medical Center and was determined to be exempt from review.
Statistical Analysis
Demographic and clinical variables were summarized with standard descriptive statistics and expressed as median (with interquartile range) for skewed continuous variables and count (with percentage) for categorical variables. Group comparisons were made with the Chi-squared and the Kruskal-Wallis test where appropriate. Kaplan-Meier survival analysis, univariate and multivariable Cox proportional-hazards regression were performed to determine survival statistics with Dunnett’s test applied for pairwise comparisons. Cause-specific hazard models were created and cumulative incidence functions were calculated with death and delisting alternating as a competing event. A two-tailed p-value of less than 0.05 was considered significant. Analyses were performed using SAS version 9.4 (SAS Institute, Inc, Cary, North Carolina).
Results
During the study period 3,361 patients met inclusion criteria. The Heartmate II was the predominant LVAD used among the study population (84%). After grouping patients into quartiles based on SES index score, demographic variables differed as anticipated: the top quartile was more educated, had a higher median income, had a greater proportion with private insurance, was more likely to be white or Asian, and was slightly older (Table 1). Clinical characteristics were similar across all quartiles except diabetes was less common and BMI was slightly less among those with a higher SES index score. A greater proportion of those in the highest SES quartile had the lowest functional status at listing. Lastly, patients in the top SES quartile were less likely to have an LVAD in place at the time of transplant listing and had a shorter time on LVAD support.
Table 1.
Baseline characteristics of study population
| Bottom Quartile N= 840 |
Second Quartile N= 841 |
Third Quartile N= 840 |
Top Quartile N= 840 |
p-value | |
|---|---|---|---|---|---|
| Male | 629 (75.5) | 642 (76.3) | 661 (78.7) | 648 (77.1) | 0.31 |
| Age | 53 (42–61) | 55 (45–62) | 56 (46.5–62) | 57 (47–63) | <0.0001 |
| LVAD Type | 0.43 | ||||
| Heartmate II | 706 (84.1) | 713 (84.8) | 713 (84.9) | 691 (82.3) | |
| Heartware HVAD | 134 (15.9) | 128 (15.2) | 127 (15.1) | 149 (17.7) | |
| Etiology of Cardiomyopathy | 0.03 | ||||
| Ischemic | 310 (36.9) | 369 (43.9) | 345 (41.1) | 332 (39.5) | |
| Non-ischemic | 530 (60.1) | 472 (56.1) | 495 (58.9) | 508 (60.5) | |
| Insurance Type | <0.0001 | ||||
| Private | 306 (36.4) | 388 (46.1) | 457 (54.4) | 512 (61.0) | |
| Medicaid | 152 (18.2) | 108 (12.8) | 97 (11.6) | 75 (8.9) | |
| Medicare | 338 (40.2) | 310 (36.9) | 245 (29.2) | 224 (26.7) | |
| Education Level | <0.0001 | ||||
| Eighth Grade or Less | 69 (8.2) | 39 (4.6) | 27 (3.2) | 27 (3.2) | |
| High School | 428 (51.0) | 397 (47.2) | 363 (43.2) | 243 (28.9) | |
| Post-Secondary | 343 (40.8) | 405 (48.2) | 450 (53.6) | 570 (67.9) | |
| Income | $35,477 (30,857–40,418) | $46,846 (42,087–51,427) | $57,881 (52,301–64,866) | $83,496 (71,393–97,955) | <0.0001 |
| Functional Status at Listing | 0.016 | ||||
| Disabled & Hospitalized | 221 (27.8) | 224 (27.9) | 226 (27.1) | 272 (33.9) | |
| Moderate Disability | 317 (39.9) | 292 (36.4) | 295 (37.1) | 266 (33.2) | |
| Cares for Self | 257 (32.3) | 287 (35.7) | 285 (35.8) | 264 (32.9) | |
| Race (%) | <0.0001 | ||||
| White | 376 (44.8) | 572 (68.0) | 620 (73.8) | 615 (73.2) | |
| African-American | 351 (41.8) | 196 (23.3) | 165 (19.6) | 136 (16.2) | |
| Hispanic | 92 (11.0) | 44 (5.2) | 34 (4.1) | 39 (4.6) | |
| Asian | 14 (1.7) | 15 (1.8) | 12 (1.4) | 41 (4.9) | |
| Diabetes (%) | 282 (33.6) | 290 (34.5) | 257 (30.6) | 232 (27.6) | 0.01 |
| Renal Function | 0.17 | ||||
| GFR>60 | 519 (61.8) | 484 (57.6) | 470 (50.6) | 460 (54.8) | |
| CKD Stage III | 261 (31.1) | 309 (36.7) | 317 (37.7) | 320 (38.1) | |
| CKD Stage IV | 31 (3.7) | 22 (2.6) | 23 (2.7) | 31 (3.7) | |
| CKD Stage V, Not on HD | 3 (0.4) | 1 (0.1) | 3 (0.4) | 1 (0.1) | |
| Dialysis | 26 (3.1) | 25 (3.0) | 27 (3.2) | 28 (3.3) | |
| BMI at Listing Hemodynamics | 28.3 (24.6–32.3) | 28.1 (24.9–32.0) | 28.1 (24.7–31.9) | 27.7 (24.4–31.0) | 0.005 |
| Mean PA Pressure (mmHg) | 31 (23–40) | 30 (23–38) | 30 (22–38) | 31 (24–39) | 0.07 |
| PCWP (mmHg) | 21 (13–28) | 20 (13–27) | 20 (13–27) | 22 (15–28) | 0.15 |
| Cardiac Index (L/min/m2) | 2.1 (1.8–2.5) | 2.1 (1.8–2.5) | 2.1 (1.8–2.6) | 2.0 (1.7–2.5) | 0.04 |
| PVR (Wood units) | 2.27 (1.49–3.37) | 2.29 (1.46–3.33) | 2.22 (1.40–3.16) | 2.29 (1.52–3.48) | 0.18 |
| LVAD at Listing (%) | 552 (65.7) | 540 (64.2) | 548 (65.2) | 506 (60.2) | 0.08 |
| Time from LVAD to Transplant (days) | 318 (170–580) | 283 (149–517) | 294 (152–516) | 265 (151–477) | 0.03 |
| Former Smoker (%) | 437 (52.2) | 457 (54.5) | 463 (55.1) | 421 (50.2) | 0.16 |
| ICD (%) | 667 (79.4) | 671 (79.8) | 668 (79.5) | 659 (78.5) | 0.97 |
| Prior Stroke (%) | 54 (6.4) | 61 (7.3) | 40 (4.8) | 44 (5.2) | 0.36 |
Values are summarized as number (%) or median (interquartile range). GFR=Glomerular filtration rate; CKD= Chronic kidney disease; HD=Hemodialysis; BMI=Body mass index; PA=Pulmonary artery; PCWP=Pulmonary capillary wedge pressure; PVR=Pulmonary vascular resistance; ICD=Implantable cardiac defibrillator
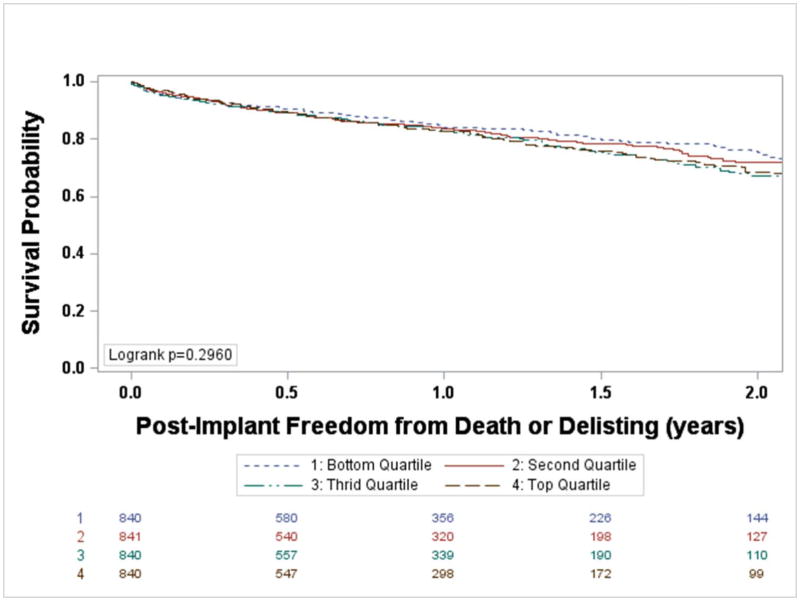
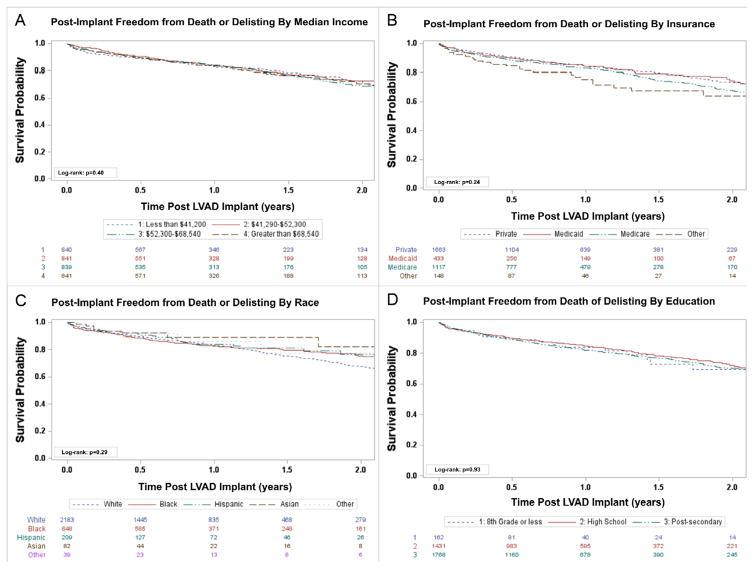
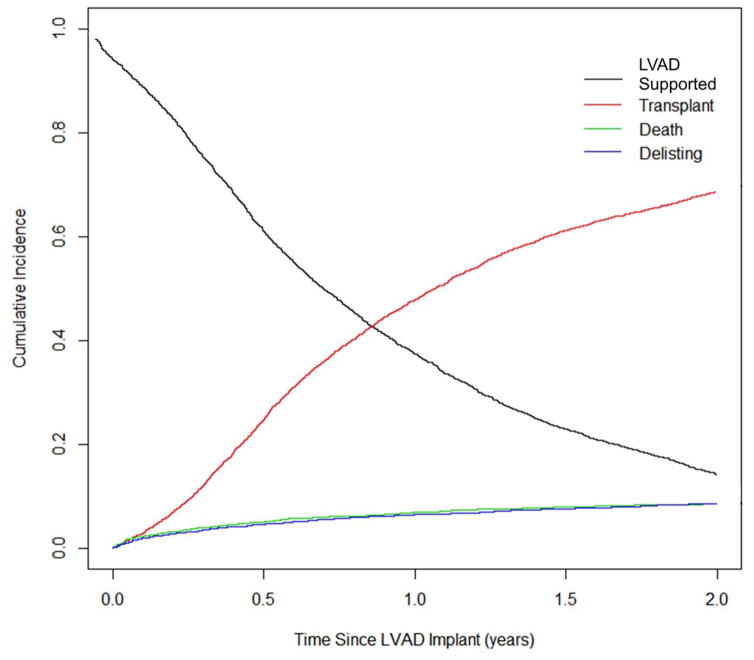
A total of 681 patients experienced death or delisting while on LVAD support. Between SES quartiles, there was no difference in event-free survival (Figure 1, p=0.30). Analysis of individual determinants of SES (education level, household income, type of insurance, and race) failed to demonstrate that any were significant predictors of the composite endpoint (Figure 2). Competing risks analysis was performed for all patients (Figure 3) and for each SES quartile, demonstrating differences in individual outcomes (Supplemental Figure 1). When accounting for delisting and transplantation as competing events, there was an increased risk of death for the top (HR 1.55, 95% CI 1.14–2.11, p=0.005) and third (HR 1.50, 95% CI 1.10–2.04, p=0.01) SES quartiles compared with the bottom quartile. A multivariable cause-specific hazard model was created for SES quartile, adjusting for clinical acuity at listing (functional status at listing and ventilator use at listing) and clinical comorbidities and factors that increase the difficulty of finding a suitable donor (age, gender, ABO blood group, BMI, pulmonary vascular resistance >3 Wood units, renal function, presence of an ICD, PRA>10%, complications requiring UNOS listing status upgrade, and waitlist time on LVAD support), which found that the increased risk of death during device support among patients of greater SES was no longer present (Top quartile 95% CI 0.95–2.04; p=0.09; Third Quartile 95% CI 0.84–1.79; p=0.28). The incidence of delisting was similar between SES quartiles.
Figure 1.
Freedom from death or delisting while on LVAD support stratified by SES index quartiles
Figure 2.
Freedom from Death or Delisting stratified by income (A), type of payment (B), race (C), and education (D)
Figure 3.
Competing Risk Plot of Waitlist Events for All Patients
A complication requiring UNOS listing status upgrade while on LVAD support occurred in 599 (18%) patients during the study period. There was no association between SES and frequency of complications requiring UNOS listing status upgrade (Range 17.1%–18.7%, p=0.86). Similarly, there was neither an increased risk of a composite measure of complications (thromboembolism, device infection, device malfunction, or life-threatening ventricular arrhythmia) across SES index quartiles, nor was there an increased risk of individual complications (Table 2).
Table 2.
Complications requiring UNOS listing status upgrade
| Second SES Quartile | Third SES Quartile | Top SES Quartile | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| HR | p-value | HR | p-value | HR | p-value | |
| Thromboembolism | 0.92 | 0.74 | 0.94 | 0.81 | 0.73 | 0.25 |
| Device Infection | 0.98 | 0.89 | 0.89 | 0.43 | 0.82 | 0.19 |
| Device Malfunction | 1.18 | 0.57 | 1.28 | 0.38 | 1.32 | 0.31 |
| Arrhythmia | 2.11 | 0.22 | 2.54 | 0.11 | 2.99 | 0.06 |
| Composite | 0.98 | 0.87 | 0.98 | 0.78 | 0.92 | 0.73 |
Reference Group: Bottom SES Quartile
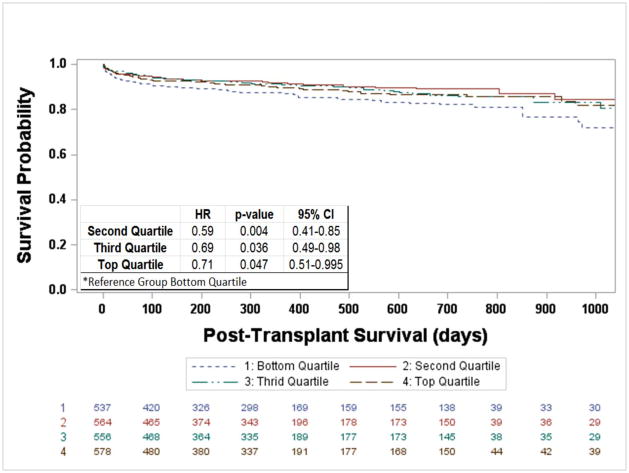
Heart transplantation occurred for 2,402 (71.5%) patients during the study period. The incidence of transplantation did not differ by SES, though the median time from LVAD implantation to transplantation was longer for the lowest SES quartile (Table 1). For the entire cohort one and two-year post-transplant survival was 89.9% and 86.2% respectively. When stratified by SES index quartiles, patients in the lowest quartile had a 29–41% increased risk of post-transplant graft loss (87.3% one-year and 82.2% two-year, p<0.03, Figure 4) compared with those in higher SES quartiles. However, no individual SES determinant (education level, income, race, or insurance type) was an independent predictor of post-transplant graft loss (Supplemental Figure 1). Adjusting for age15, renal dysfunction15, device infection16, 17, and duration of LVAD support18, 19 (previously reported pre-transplant causes of decreased BTT post-transplant survival) in addition to ischemic time, allograft rejection requiring hospitalization, and post-transplant hospitalizations for infection 15 the increased risk of post-transplant mortality among those of in the bottom SES quartile remained (Second Quartile: HR 0.57, 0.39–0.82, p=0.002; Third Quartile: HR 0.67, 0.47–0.94, p=0.02; Top Quartile: HR: 0.68, 0.48–0.95, p=0.02).
Figure 4.
Post-transplant freedom from graft loss stratified by SES index quartiles
Discussion
Socioeconomic disparities exist in healthcare in the United States. These disparities extend to Stage D heart failure with differences in multiple listing prior to heart transplantation14 and survival & rejection after transplantation7. This study examined the impact that SES and its determinants SES had on patients bridged to transplantation with a LVAD and resulted in three notable findings. First, all patients regardless of SES had similar freedom from death or delisting on LVAD support. Second, patients in the top two SES quartiles had an increased risk of death on the waitlist during LVAD support, which was explained by increased clinical acuity and differences in baseline clinical risk factors. Lastly, patients in the lowest SES index quartile had an early and sustained decreased post-transplant survival compared with each greater SES index quartile.
Implantation of a left ventricular assist device leads to improved quality of life, increased exercise tolerance20, and improved survival.21 In this study, SES did not impact freedom from death or delisting while on device support. However, higher SES status was associated with an unadjusted increased risk of death. A plausible explanation is that those of greater SES were clinically different and a higher risk population, which was the case in this study. Those in the top SES quartile had increased odds of being severely debilitated & hospitalized at the time of listing and on a ventilator at the time of listing. While clinical acuity at listing accounted for some of the increased risk of death for those with greater SES, a portion remained unexplained. This analysis attempted to account for alternative etiologies for the increased risk by controlling for clinical characteristics that increase the difficulty of finding a suitable donor (PRA>10%, BMI, gender, ABO blood type) and those that signify additional comorbidities (PVR suggesting pulmonary hypertension, ICD presence for chronicity of heart failure, renal dysfunction, age, waitlist time on LVAD support, and device complications). The increased risk of death on LVAD support was no longer significant for higher SES quartiles when adjusting for those clinical differences, suggesting that the listing characteristics may differ based on SES. Patients of lower SES more often had an upfront strategy with LVAD implantation at the time of listing (potentially bridge to decision) and were not as functionally debilitated when compared to those with the highest SES. Whether this was due to earlier engagement in care by those with higher SES or a bias based on SES remains unclear, but merits further exploration.
In this study SES index was associated with post-transplant outcomes. Patients in the lowest SES quartile had an early and sustained decrease in post-transplant survival, even after controlling for risk factors for post-transplant mortality. This finding is consistent with the impact of SES on pediatric heart transplant recipients6 and previous analyses of the UNOS database demonstrating an association between public insurance and worse outcomes following kidney22, liver23, and lung transplantation24. Insurance coverage of immunosuppressive drugs is one possible cause for the difference in post-transplant outcomes, as prescription coverage can vary between different types of insurance. In this study survival was equivalent for all SES during LVAD support when new medications (warfarin, aspirin, and/or dipyridamole) are not prohibitively expensive. However post-transplantation, when more expensive immunosuppressive drugs ($31,209 annually in 2011)25 are required, those with low SES had an increased risk of death. Post-transplant care requires frequent follow-up for monitoring of immunosuppressive drug levels and rejection surveillance, which is another potential explanation of this difference. In this study, however, there was no evidence of increased odds of hospitalization for rejection or hospitalization for infection following transplantation among those of lower SES.
Limitations of this study include the retrospective nature of the study. The UNOS dataset that was used is high-quality in that for all U.S. transplant centers data submission is mandatory by law, however it is limited to the data collected. As such, a number of covariates of interest including readmission, bleeding, and serum albumin were not available for analysis. Further, there were missing data. Although no variable had more than 1% missing aside from hemodynamic parameters where up to 15% was missing. Nevertheless this introduces the potential for bias into the analysis. Similarly, not all complications were able to be captured given the limitations of the UNOS database. The most serious complications that required UNOS status upgrade were captured however. The study population was also BTT, as the UNOS database does not include destination therapy patients. Lastly, the SES index was calculated using Zip-code level Census data as some specific SES determinants are not captured by the UNOS database. This has been used as a strategy in many prior analyses of the UNOS database; nonetheless Zip-code level data was used as a proxy for patient level data under the presumption that these factors are homogenous within a Zip-code and a patient’s Zip-code did not vary.
In conclusion, SES and its determinants did not impact survival to transplantation on LVAD support. Those of higher SES had an unadjusted increased risk of death during LVAD support, though this was due to clinical differences. Following transplantation, low SES was associated with worse post-transplant survival. Further study is needed to confirm and understand a differential effect of SES on post-transplant outcomes that was not seen during LVAD support prior to HT.
Supplementary Material
Clinical Perspective.
One major criticism of healthcare in the United States is the impact that socioeconomic status (SES) has on individual health outcomes. Previous studies have demonstrated that lower SES is a risk factor for heart failure, hospital readmission, and death. The impact of SES extends to Stage D heart failure as those with lower SES have decreased survival and an increased risk of rejection following transplantation. This study was an analysis of 3,361 adult patients in UNOS database to examine the impact of SES on patients supported with a continuous-flow left ventricular assist device (LVAD). The data demonstrated in an unadjusted analysis that there was increased waitlist mortality for the higher SES quartiles; however this increased risk was due to increased comorbid conditions. There was no difference between SES quartiles for complications requiring UNOS listing status upgrade. Post-transplantation survival was less for the lowest SES quartile, consistent with previous studies. This study demonstrated that SES and its determinants did not impact survival to transplantation on LVAD support and that SES should not be a barrier to use of an LVAD.
Acknowledgments
Sources of Funding
This study was supported by Lisa and Mark Schwartz and the Program to Reverse Heart Failure at New York Presbyterian Hospital/Columbia University. Dr. Clerkin is supported by National Institutes of Health Grant T32 HL007854-16.
Footnotes
Disclosures
Dr. Naka received consulting fees from Thoratec and Heartware. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
References
- 1.Hawkins NM, Jhund PS, McMurray JJV, Capewell S. Heart failure and socioeconomic status: accumulating evidence of inequality. European Journal of Heart Failure. 2012;14:138–146. doi: 10.1093/eurjhf/hfr168. [DOI] [PubMed] [Google Scholar]
- 2.Foraker RE, Rose KM, Suchindran CM, Chang PP, McNeill AM, Rosamond WD. Socioeconomic Status, Medicaid Coverage, Clinical Comorbidity, and Rehospitalization or Death After an Incident Heart Failure Hospitalization Atherosclerosis Risk in Communities Cohort (1987 to 2004) Circulation-Heart Failure. 2011;4:308–316. doi: 10.1161/CIRCHEARTFAILURE.110.959031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Philbin EF, Dec GW, Jenkins PL, DiSalvo TG. Socioeconomic status as an independent risk factor for hospital readmission for heart failure. American Journal of Cardiology. 2001;87:1367–1371. doi: 10.1016/s0002-9149(01)01554-5. [DOI] [PubMed] [Google Scholar]
- 4.Singh TP, Almond C, Givertz MM, Piercey G, Gauvreau K. Improved survival in heart transplant recipients in the United States: racial differences in era effect. Circulation Heart failure. 2011;4:153–60. doi: 10.1161/CIRCHEARTFAILURE.110.957829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu V, Bhattacharya J, Weill D, Hlatky MA. Persistent racial disparities in survival after heart transplantation. Circulation. 2011;123:1642–9. doi: 10.1161/CIRCULATIONAHA.110.976811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davies RR, Russo MJ, Reinhartz O, Maeda K, Rosenthal DN, Chin C, Bernstein D, Mallidi HR. Lower socioeconomic status is associated with worse outcomes after both listing and transplanting children with heart failure. Pediatric transplantation. 2013;17:573–81. doi: 10.1111/petr.12117. [DOI] [PubMed] [Google Scholar]
- 7.Singh TP, Givertz MM, Semigran M, DeNofrio D, Costantino F, Gauvreau K. Socioeconomic Position, Ethnicity, and Outcomes in Heart Transplant Recipients. The American Journal of Cardiology. 2010;105:1024–1029. doi: 10.1016/j.amjcard.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 8.Davies RR, Singh SK, Russo MJ, Robbins RC, Oyer PE, Mallidi HR. 61 The Association between Poor Socioeconomic Status and Poor Long-Term Outcomes Following Heart Transplantation. The Journal of Heart and Lung Transplantation. 2011;30:S28. [Google Scholar]
- 9.Smith SA, Hasan AK, Binkley PF, Foraker RE. The impact of insurance and socioeconomic status on outcomes for patients with left ventricular assist devices. The Journal of surgical research. 2014;191:302–8. doi: 10.1016/j.jss.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Snipelisky D, Stulak JM, Schettle SD, Sharma S, Kushwaha SS, Dunlay SM. Psychosocial characteristics and outcomes in patients with left ventricular assist device implanted as destination therapy. American heart journal. 2015;170:887–94. doi: 10.1016/j.ahj.2015.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agency for Healthcare Research and Quality. [Accessed Feb. 16, 2016];Creating and validating an index of socioeconomic status. Available at: http://archive.ahrq.gov/research/findings/final-reports/medicareindicators/medicareindicators3.html.
- 12.Lentine KL, Schnitzler MA, Xiao H, Saab G, Salvalaggio PR, Axelrod D, Davis CL, Abbott KC, Brennan DC. Racial Variation in Medical Outcomes among Living Kidney Donors. New England Journal of Medicine. 2010;363:724–732. doi: 10.1056/NEJMoa1000950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blum AB, Egorova NN, Sosunov EA, Gelijns AC, DuPree E, Moskowitz AJ, Federman AD, Ascheim DD, Keyhani S. Impact of socioeconomic status measures on hospital profiling in New York City. Circulation Cardiovascular quality and outcomes. 2014;7:391–7. doi: 10.1161/CIRCOUTCOMES.113.000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Givens RC, Dardas T, Clerkin KJ, Restaino S, Schulze PC, Mancini DM. Outcomes of Multiple Listing for Adult Heart Transplantation in the United States Analysis of OPTN Data From 2000 to 2013. JACC: Heart Failure. 2015;3:933–941. doi: 10.1016/j.jchf.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lund LH, Edwards LB, Kucheryavaya AY, Benden C, Christie JD, Dipchand AI, Dobbels F, Goldfarb SB, Levvey BJ, Meiser B, Yusen RD, Stehlik J. The Registry of the International Society for Heart and Lung Transplantation: Thirty-first Official Adult Heart Transplant Report—2014; Focus Theme: Retransplantation. The Journal of Heart and Lung Transplantation. 2014;33:996–1008. doi: 10.1016/j.healun.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 16.Healy AH, Baird BC, Drakos SG, Stehlik J, Selzman CH. Impact of Ventricular Assist Device Complications on Posttransplant Survival: An Analysis of the United Network of Organ Sharing Database. The Annals of Thoracic Surgery. 2013;95:870–875. doi: 10.1016/j.athoracsur.2012.10.080. [DOI] [PubMed] [Google Scholar]
- 17.John R, Pagani FD, Naka Y, Boyle A, Conte JV, Russell SD, Klodell CT, Milano CA, Rogers J, Farrar DJ, Frazier OH. Post–cardiac transplant survival after support with a continuous-flow left ventricular assist device: Impact of duration of left ventricular assist device support and other variables. The Journal of Thoracic and Cardiovascular Surgery. 2010;140:174–181. doi: 10.1016/j.jtcvs.2010.03.037. [DOI] [PubMed] [Google Scholar]
- 18.Takeda K, Takayama H, Kalesan B, Uriel N, Colombo PC, Jorde UP, Yuzefpolskaya M, Mancini DM, Naka Y. Outcome of cardiac transplantation in patients requiring prolonged continuous-flow left ventricular assist device support. The Journal of Heart and Lung Transplantation. 2015;34:89–99. doi: 10.1016/j.healun.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 19.Smedira NG, Hoercher KJ, Yoon DY, Rajeswaran J, Klingman L, Starling RC, Blackstone EH. Bridge to transplant experience: factors influencing survival to and after cardiac transplant. J Thorac Cardiovasc Surg. 2010;139:1295–305. 1305.e1–4. doi: 10.1016/j.jtcvs.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 20.Rogers JG, Aaronson KD, Boyle AJ, Russell SD, Milano CA, Pagani FD, Edwards BS, Park S, John R, Conte JV, Farrar DJ, Slaughter MS. Continuous Flow Left Ventricular Assist Device Improves Functional Capacity and Quality of Life of Advanced Heart Failure Patients. Journal of the American College of Cardiology. 2010;55:1826–1834. doi: 10.1016/j.jacc.2009.12.052. [DOI] [PubMed] [Google Scholar]
- 21.Mancini D, Colombo PC. Left Ventricular Assist Devices A Rapidly Evolving Alternative to Transplant. Journal of the American College of Cardiology. 2015;65:2542–2555. doi: 10.1016/j.jacc.2015.04.039. [DOI] [PubMed] [Google Scholar]
- 22.Goldfarb-Rumyantzev AS, Koford JK, Baird BC, Chelamcharla M, Habib AN, Wang B-J, Lin S-j, Shihab F, Isaacs RB. Role of Socioeconomic Status in Kidney Transplant Outcome. Clinical Journal of the American Society of Nephrology. 2006;1:313–322. doi: 10.2215/CJN.00630805. [DOI] [PubMed] [Google Scholar]
- 23.Yoo HY, Thuluvath PJ. Outcome of liver transplantation in adult recipients: Influence of neighborhood income, education, and insurance. Liver Transplantation. 2004;10:235–243. doi: 10.1002/lt.20069. [DOI] [PubMed] [Google Scholar]
- 24.Allen JG, Arnaoutakis GJ, Orens JB, McDyer J, Conte JV, Shah AS, Merlo CA. Insurance status is an independent predictor of long-term survival after lung transplantation in the United States. The Journal of Heart and Lung Transplantation. 2011;30:45–53. doi: 10.1016/j.healun.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 25.Evans RW. An Actuarial Perspective on the Annual Per Patient Maintenance Immunosuppressive Medication Costs for Transplant Recipients: 1993–2011. Am J Transplant. 2013;13:270–271. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.