Abstract
Knee pain in young, active patients with meniscus-deficient knees and articular cartilage damage can present a challenge to treatment. Meniscal allograft transplantation (MAT) has shown good clinical results as treatment for meniscus deficiency; however, worse outcomes have been observed in patients with significant chondral damage. The development of chondral restorative techniques such as osteochondral allograft transplantation (OCA) has expanded the population of patients who may benefit from MAT. We present a case of proximal tibial osteochondral and lateral meniscal allograft transplant. This review includes a sample of patient examinations and imaging, followed by a detailed technical description of the case. The technique article concludes with a discussion on the niche combined MAT-OCA procedures occupy in the patient treatment realm.
Knee pain in young, active patients with meniscus-deficient knees and articular cartilage damage can present a challenge to treatment. Meniscal allograft transplantation (MAT) has shown good clinical results as treatment for meniscus deficiency.1, 2, 3 However, studies have shown worse outcomes following MAT in patients with significant chondral damage.4 Historically, concomitant articular cartilage loss contraindicated MAT. Unfortunately, these pathologic changes are frequently associated, given the well-established chondroprotective effects of the meniscus.5 The development of chondral restorative techniques such as osteochondral allograft transplantation (OCA) has expanded the population of patients who may benefit from MAT.
Combined MAT and OCA has shown good clinical outcomes, comparable to either procedure done in isolation.1, 6, 7 The combined procedure is indicated in a painful, meniscus-deficient knee with full-thickness articular cartilage defects, most commonly caused by osteoarthritis, degenerative or traumatic chondral lesions (including osteochondritis dissecans), or tibial plateau fractures.6
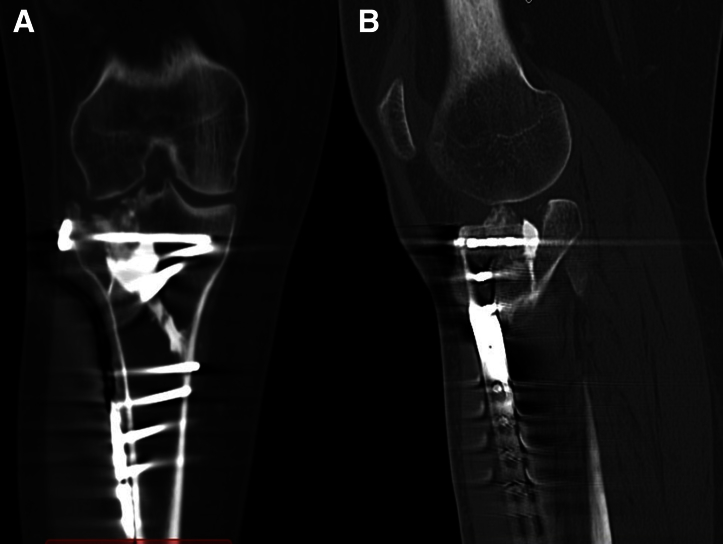
Figure 1 shows a radiographic image of a patient with previous tibial plateau fracture (after open reduction, internal fixation) as an example of a patient who may be indicated for a MAT and OCA procedure. Computed tomographic scans of the same knee (Fig 2) show lateral joint line depression and bone loss with irregularity of the tibial plateau.
Fig 1.

Radiograph showing 1 degree of mechanical axis deviation. This is an example of a patient who may be indicated for a MAT and OCA procedure. Previous fixation of right tibial plateau fracture without evidence of hardware failure can be seen. There is no significant leg length discrepancy. (MAT, meniscal allograft transplantation; OCA, osteochondral allograft transplantation.)
Fig 2.
CT scan of a potential patient. (A) Coronal CT showing a large depression in the lateral tibial plateau, with otherwise intact hardware. The medial joint space is intact. (B) Sagittal CT showing the defect is about 1 cm in the anteroposterior direction. The patient also has some osteophytes in that compartment. (CT, computed tomography.)
Surgical Technique
Setup
A diagnostic arthroscopy showed no healthy cartilage on the tibial plateau, with grade I to II lesions on the distal femur, without full-thickness defects. The patient was brought into the operating room where general anesthesia was administered following a femoral nerve block. The patient was positioned supine on the operating table. A thigh tourniquet was applied to the operative extremity.
Approach
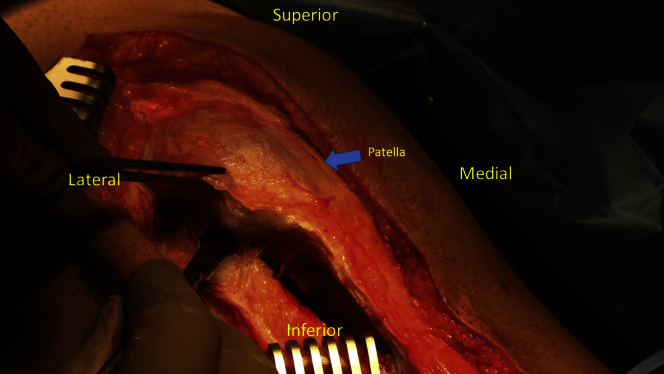
The patient's previous midline incision is used for the operative approach, as can be seen in Video 1. The incision is carried down to the extensor retinaculum. A full-thickness flap is developed laterally and extended posteriorly around the lateral border of the tibia. A lateral parapatellar arthrotomy is then made and used to expose the lateral tibial plateau and lateral femoral condyle, with the patella retracted medially (Fig 3). The fat pad is excised to improve exposure of the lateral tibial plateau. The femoral condyles are then inspected. Any remaining lateral meniscal tissue is removed from the proximal tibia with a scalpel. Z retractors and Hohmann retractors are then placed to adequately visualize the lateral compartment.
Fig 3.
Lateral arthrotomy. With the patient placed supine on the operating table, this image is looking anteriorly and obliquely at the right knee. The patient's previous midline incision is used for the operative approach as can be seen in Video 1. The incision is carried down to the extensor retinaculum. A full-thickness flap is developed laterally and extended posteriorly around the lateral border of the tibia. A lateral parapatellar arthrotomy is then made and used to expose the lateral tibial plateau and lateral femoral condyle, with the patella retracted medially.
Plateau Preparation
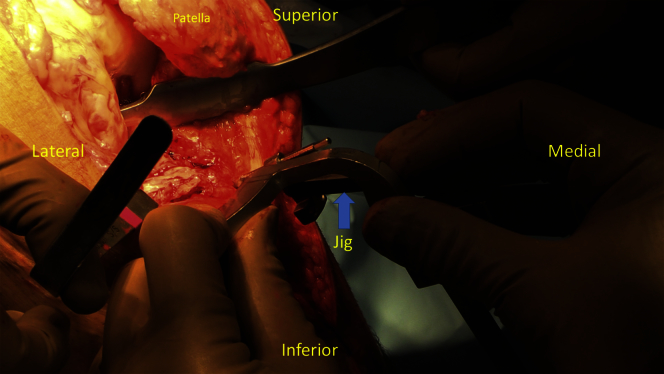
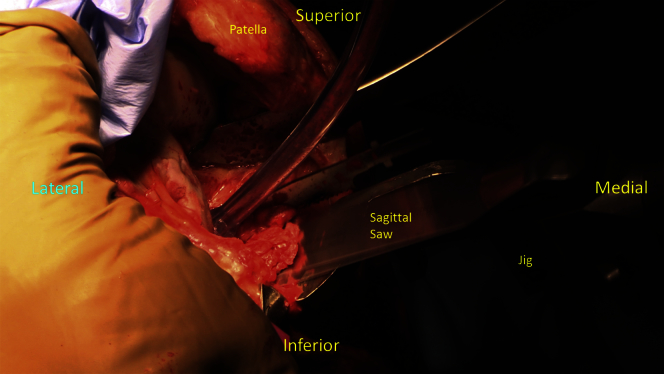
A unicondylar knee arthroplasty guide (Arthrex, Naples, FL) is then placed, first on the tibia and secured provisionally. Once properly aligned to the lateral tibial plateau ensuring appropriate slope and coronal angulation, the jig is pinned to the tibia. The line connecting the central aspects of the tibial spines is used as a sagittal cut reference. The extramedullary guide from the unicondylar knee arthroplasty system is used to optimize coronal alignment (Fig 4). The proximal tibial cut is then made with a reciprocating saw (Stryker, Kalamazoo, MI). Care is taken to avoid medial penetration of the cruciate ligaments with the anterior-to-posterior sagittal cut. The proximal tibial plateau fragment is removed to expose the well-defined void in the lateral tibial plateau. The edges of the cut are smoothed with a box rasp (Fig 5).
Fig 4.
With the patient placed supine on the operating table, this image is looking anteriorly and obliquely at the right knee. A unicondylar knee arthroplasty guide (Arthrex, Naples, FL) is properly aligned to the lateral tibial plateau ensuring appropriate slope and coronal angulation. The line connecting the central aspects of the tibial spines is used as a sagittal cut reference. The extramedullary guide from the unicondylar knee arthroplasty system is used to optimize coronal alignment.
Fig 5.
With the patient placed supine on the operating table, this image is looking anteriorly and obliquely at the right knee. Once the unicondylar knee arthroplasty guide is set up to ensure alignment, the proximal tibial cut is then made with a reciprocating saw (Stryker, Kalamazoo, MI). Care is taken to avoid medial penetration of the cruciate ligaments with the anterior-to-posterior sagittal cut. The proximal tibial plateau fragment is removed to expose the well-defined void in the lateral tibial plateau. The edges of the cut are smoothed with a box rasp.
Osteochondral Allograft Preparation
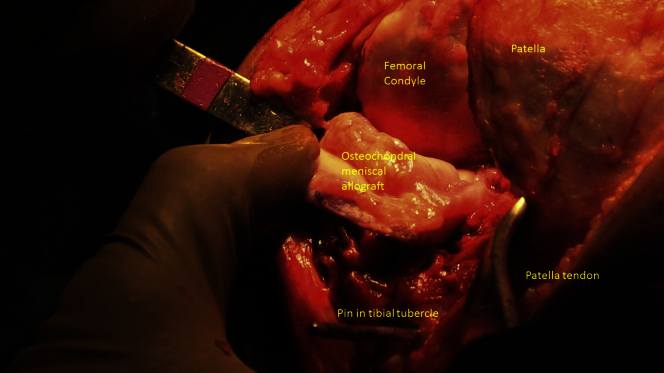
On the back table, an osteochondral proximal tibial allograft is prepared with the meniscus attached at the anterior and posterior roots (Fig 6). On the allograft, the length and width are marked after measuring them on the tibial cut. The height is obtained by measuring the height at the sagittal cut. With the height, width, and length measurements obtained, the allograft can be cut to approximate the recipient site on the tibia as closely as possible. The reciprocating saw is used to refine the tibial plateau cut to ensure optimal congruency of the graft with the recipient site.
Fig 6.
With the patient placed supine on the operating table, this image is looking anteriorly and obliquely at the right knee. An osteochondral proximal tibial allograft is prepared with the meniscus attached at the anterior and posterior roots (Fig 3). On the allograft, the length and width are marked after measuring them on the tibial cut. The height is obtained by measuring the height at the sagittal cut. With the height, width, and length measurements obtained, the allograft can be cut to approximate the recipient site on the tibia as closely as possible.
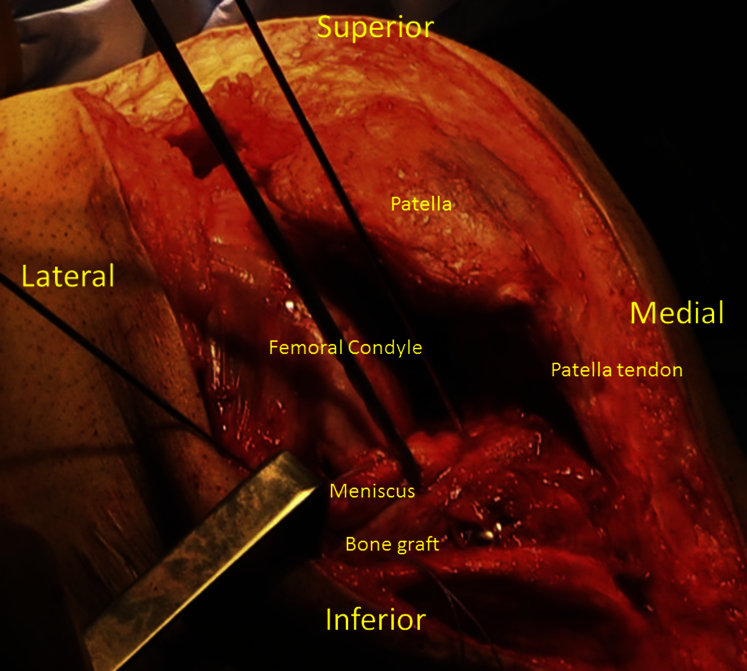
Introduction of Allograft
The allograft is then fit onto the osteotomy site and engaged within the tibia (Fig 7). Fluoroscopic assessment should then be used to ensure that the graft is flush in both the coronal and sagittal planes without overhang. The graft is provisionally fixed with 3 K-wires anteriorly, anterolaterally, and laterally. Confirmation of pin placement is confirmed with fluoroscopy. On satisfactory placement, the 3 K-wires are used to guide the placement of three 4.5-mm cannulated headless compression screws (Synthes, West Chester, PA) for final fixation (Fig 8). Stability of the plateau is assessed following placement of the screws.
Fig 7.
With the patient placed supine on the operating table, this image is looking anteriorly and obliquely at the right knee. After proper adjustments to ensure fit, the osteochondral meniscal allograft is seen here being placed into the previously made arthrotomy. Fluoroscopic assessment should then be used to ensure that the graft is flush in both the coronal and sagittal planes without overhang. The graft will be secured provisionally with 3 K-wires before final fixation.
Fig 8.
With the patient placed supine on the operating table, this image is looking anteriorly and obliquely at the right knee. After the graft is introduced onto the tibia site and satisfactory placement is confirmed fluoroscopically, the graft is provisionally fixed with 3 K-wires anteriorly, anterolaterally, and laterally. Pin placement is confirmed with fluoroscopy. On satisfactory placement, the 3 K-wires are used to guide the placement of three 4.5-mm cannulated headless compression screws (Synthes, West Chester, PA) for final fixation. Stability of the plateau is assessed following placement of the screws.
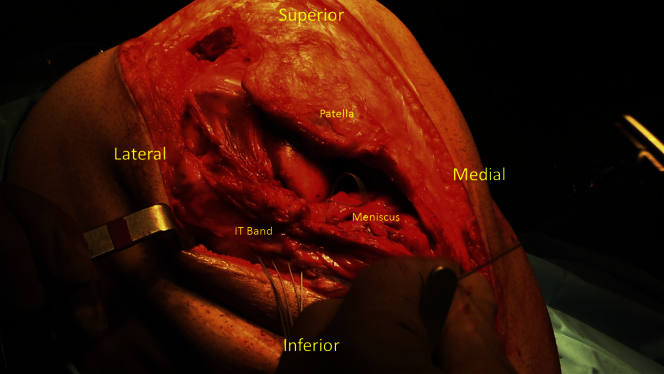
Closure
An incision is made through the iliotibial (IT) band in line with its fibers to reach the lateral capsule. This is done so that the capsule, and not the IT band, is being sutured, allowing the IT band to slide freely over the capsule. The meniscus allograft is sutured to the capsule starting just anterior to the popliteus tendon with at least 6 No. 2 FiberWire sutures in a vertical mattress fashion using an inside out technique (Fig 9). The lateral meniscus should have some excursion posteriorly, and therefore a posterior suture is not necessary. Radiographs are used to confirm congruence of the allograft with the tibia.
Fig 9.
With the patient placed supine on the operating table, this image is looking anteriorly and obliquely at the right knee. An incision is made through the IT band in line with its fibers to reach the lateral capsule. This is done so that the capsule, and not the IT band, is being sutured, allowing the IT band to slide freely over the capsule. The meniscus allograft is sutured to the capsule starting just anterior to the popliteus tendon with at least 6 No. 2 FiberWire sutures in a vertical mattress fashion using an inside-out technique. The lateral meniscus should have some excursion posteriorly, and therefore a posterior suture is not necessary. (IT, iliotibial.)
The area is then copiously lavaged. The capsule, retinaculum, and skin are closed and dressed. The patient is placed in a hinged brace locked in extension.
Postoperative Management
The patient is kept partially weightbearing for the first 2 weeks and advanced to weightbearing as tolerated with crutches (crutches discontinued at 4 weeks postoperation if gait is normalized). A hinged knee brace is worn for 6 weeks postoperation—locked in full extension for ambulation during the first 2 weeks, and ranged from 0° to 90° in weeks 3 to 6. Range of motion begins at 0° to 90° nonweightbearing for the first 2 weeks, and progressed to full nonweightbearing range of motion (ROM) as tolerated over weeks 2 to 8. At weeks 8 to 12, the patient is transitioned to full active ROM.
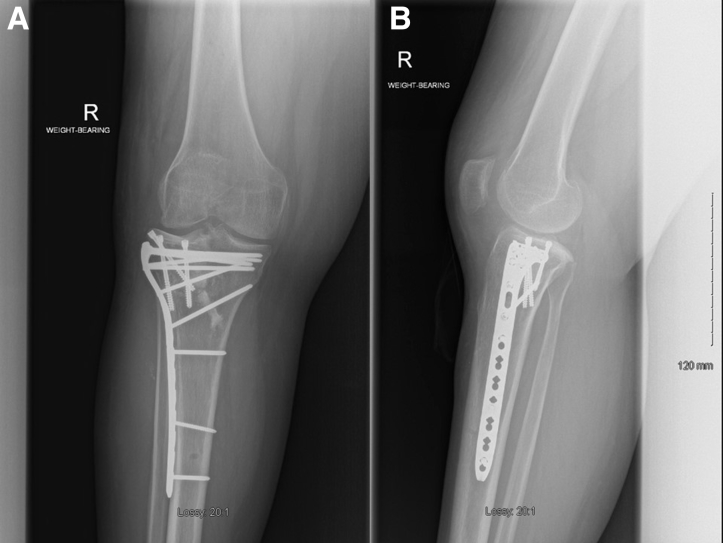
At the 2-month follow-up, the patient has a well-healed incision with much improved pain, trace effusion and 0° to 110° ROM. Radiographs reveal an intact osteochondral allograft with intact hardware with excellent alignment (Fig 10). Pearls and pitfalls for the procedure can be found in Table 1.
Fig 10.
Anteroposterior and lateral radiographs taken 2 months postoperatively showing an intact osteochondral allograft with intact hardware.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| The edges of the cut are smoothed with a box rasp. | Care is taken to avoid medial penetration of the cruciate ligaments with the anterior-to-posterior sagittal cut. |
| Obtain allograft height by measuring the height at the sagittal cut. | The lateral meniscus should have some excursion posteriorly, and therefore a posterior suture is not necessary. |
| Fluoroscopic assessment should then be used to ensure that the graft is flush in both the coronal and sagittal planes without overhang. | Ensure appropriate slope and coronal angulation of the jig before pinning to the tibia. |
| Suture the meniscus to the capsule, and not the IT band, allowing the IT band to slide freely over the capsule. |
IT, iliotibial.
Discussion
Historically, full-thickness cartilage lesions were seen as contraindications to MAT, whereas meniscus deficiency contraindicated cartilage restoration techniques.6, 7 Unfortunately these conditions frequently occur together, with many biomechanical studies clearly showing accelerated chondral damage in meniscus-deficient knees.8, 9 Furthermore, traumatic injuries such as tibial plateau fractures often result in damage to both the articular cartilage and the meniscus. The high prevalence of these combined pathologies has led to the development of combined MAT-OCA techniques, the major advantage of which is the ability to restore articular cartilage as well as the chondroprotective effects of the meniscus.
Although clinical outcomes and patient satisfaction following combined OCA and MAT are good, a major disadvantage of the combined MAT and OCA procedure is the risk of requiring reoperation. Approximately 50% of patients will require at least 1 additional procedure, most often arthroscopic debridement.6, 7 Despite high rates of reoperation, failure—as defined as the need for an additional operation resulting in removal or replacement of 1 or more of the grafts—is seen in only 12% of patients.6 Mean time to failure is reported to be 3.2 and 2.7 years for MAT and OCA, respectively.6 These failures are most commonly treatment with either allograft removal or conversion to total knee arthroplasty.6, 7 A trend toward worse results is seen in patients with advanced osteoarthritis, particularly if chondral damage requiring OCA is present on both the tibial plateau and distal femur.6 Table 2 summarizes the advantages and disadvantages of the MAT-OCA procedure.
Table 2.
Advantages and Disadvantages
| Advantages | Limitations |
|---|---|
| Restores articular cartilage and chondroprotective effect of meniscus | High rate of reoperation—up to 50% require at least 1 additional procedure |
| Good option for young patients with osteochondral and meniscal pathology who want to avoid joint arthroplasty | Requires normal knee alignment |
| Especially useful in the treatment of posttraumatic arthritis, such as following tibial plateau fractures. | Trend toward worse outcomes with significant knee osteoarthritis—particularly bipolar osteoarthritis |
It is important to note that the majority of patients indicated for MAT-OCA have complex osteochondral and meniscal pathologies that have failed one or more previous surgical treatments.6, 7 In the absence of graft failure, MAT-OCA has been shown to significantly improve symptoms in these difficult-to treat patients.1, 6, 7, 10 It has also been recommended that ideal candidates for MAT-OCA should have normal to near normal knee alignment and ligamentous stability.7 Currently, we would be reluctant to offer a combined MAT-OCA procedure to patients with advanced, bipolar osteoarthritis—particularly those older than 50 years—as joint arthroplasty may be the more appropriate surgical treatment option. However, we believe that combined MAT-OCA is an important treatment option for younger patients with painful, meniscus-deficient knees that desire a certain level of activity prohibited by joint replacement. It may be especially useful for those suffering from posttraumatic arthritis following tibial plateau fractures, particularly if identified before the development of bipolar chondral lesions.
Combined MAT-OCA procedures are a useful treatment option, especially in young patients with complex osteochondral and meniscal pathology. The high rates of reoperation should be discussed with patients before surgery. Evidence suggests early surgical treatment, before the development of bipolar chondral lesions.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
The patient is placed supine on the operating table. His right knee is draped and prepped in the usual sterile fashion. The patient's previous midline incision was used for the operative approach. The incision was carried down to the extensor retinaculum. A full-thickness flap was developed laterally and extended posteriorly around the lateral border of the tibia. A unicondylar knee arthroplasty guide was properly aligned to the lateral tibial plateau ensuring appropriate slope and coronal angulation. This guide was used to make the proximal tibial cut with a reciprocating saw after the corresponding measurements were made on the allograft. The proximal tibial plateau fragment was removed to expose the well-defined void in the lateral tibial plateau. On the back table, an osteochondral proximal tibial allograft was prepared with the meniscus attached at the anterior and posterior roots. The allograft was engaged within the tibia. Fluoroscopic assessment ensured that the graft was flush in both the coronal and sagittal planes without overhang. Three 4.5-mm cannulated headless compression screws were used to secure the allograft anteriorly, anterolaterally, and laterally. Stability of the plateau was assessed following placement of the screws. The wound was then closed in the usual fashion.
References
- 1.Abrams G.D., Hussey K.E., Harris J.D., Cole B.J. Clinical results of combined meniscus and femoral osteochondral allograft transplantation: Minimum 2-year follow-up. Arthroscopy. 2014;30:964–970. doi: 10.1016/j.arthro.2014.03.010. [DOI] [PubMed] [Google Scholar]
- 2.Saltzman B.M., Bajaj S., Salata M. Prospective long-term evaluation of meniscal allograft transplantation procedure: A minimum of 7-year follow-up. J Knee Surg. 2012;25:165–175. doi: 10.1055/s-0032-1313738. [DOI] [PubMed] [Google Scholar]
- 3.Verdonk P.C.M., Verstraete K.L., Almqvist K.F. Meniscal allograft transplantation: Long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc. 2006;14:694–706. doi: 10.1007/s00167-005-0033-2. [DOI] [PubMed] [Google Scholar]
- 4.Van Arkel E.R., de Boer H.H. Human meniscal transplantation. Preliminary results at 2 to 5-year follow-up. J Bone Joint Surg Br. 1995;77:589–595. [PubMed] [Google Scholar]
- 5.Fairbank T.J. Knee joint changes after menisectomy. J Bone Joint Surg Br. 1948;30:664–670. [PubMed] [Google Scholar]
- 6.Getgood A., Gelber J., Gortz S., De Young A., Bugbee W. Combined osteochondral allograft and meniscal allograft transplantation: A survivorship analysis. Knee Surg Sports Traumatol Arthrosc. 2015;23:946–953. doi: 10.1007/s00167-015-3525-8. [DOI] [PubMed] [Google Scholar]
- 7.Harris J.D., Cavo M., Brophy R., Siston R., Flanigan D. Biological knee reconstruction: A systematic review of combined meniscal allograft transplantation and cartilage repair or restoration. Arthroscopy. 2011;27:409–418. doi: 10.1016/j.arthro.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 8.McDermott I.D., Amis A.A. The consequences of meniscectomy. J Bone Joint Surg Br. 2006;88:1549–1556. doi: 10.1302/0301-620X.88B12.18140. [DOI] [PubMed] [Google Scholar]
- 9.McDermott I.D., Lie D.T.T., Edwards A., Bull A.M.J., Amis A.A. The effects of lateral meniscal allograft transplantation techniques on tibio-femoral contact pressures. Knee Surg Sports Traumatol Arthrosc. 2008;16:553–560. doi: 10.1007/s00167-008-0503-4. [DOI] [PubMed] [Google Scholar]
- 10.Rue J.-P.H., Yanke A.B., Busam M.L., McNickle A.G., Cole B.J. Prospective evaluation of concurrent meniscus transplantation and articular cartilage repair: Minimum 2-year follow-up. Am J Sports Med. 2008;36:1770–1778. doi: 10.1177/0363546508317122. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is placed supine on the operating table. His right knee is draped and prepped in the usual sterile fashion. The patient's previous midline incision was used for the operative approach. The incision was carried down to the extensor retinaculum. A full-thickness flap was developed laterally and extended posteriorly around the lateral border of the tibia. A unicondylar knee arthroplasty guide was properly aligned to the lateral tibial plateau ensuring appropriate slope and coronal angulation. This guide was used to make the proximal tibial cut with a reciprocating saw after the corresponding measurements were made on the allograft. The proximal tibial plateau fragment was removed to expose the well-defined void in the lateral tibial plateau. On the back table, an osteochondral proximal tibial allograft was prepared with the meniscus attached at the anterior and posterior roots. The allograft was engaged within the tibia. Fluoroscopic assessment ensured that the graft was flush in both the coronal and sagittal planes without overhang. Three 4.5-mm cannulated headless compression screws were used to secure the allograft anteriorly, anterolaterally, and laterally. Stability of the plateau was assessed following placement of the screws. The wound was then closed in the usual fashion.