Fig. 1.
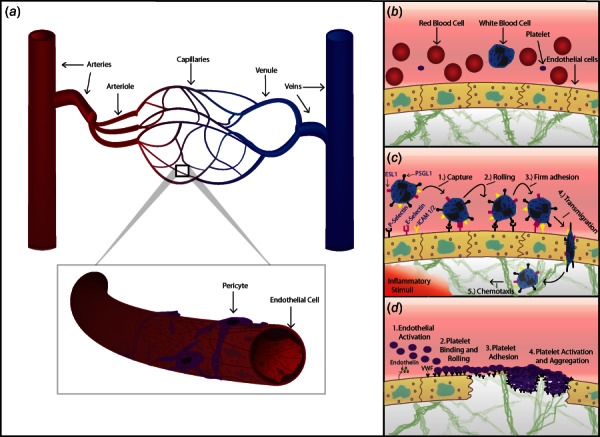
(a) Schematic of the systemic circulation. An artery is shown dividing into smaller arteries, arterioles, and capillaries. These drain into postcapillary venules, which collect into veins. A capillary is shown in magnification, consisting of a single layer of endothelial cells supported by scattered pericytes. (b) Circulating blood, including red blood cells, platelets, and a neutrophil are shown within a blood vessel bounded by endothelial cells. Vessels are supported by ECM components within the interstitium. (c) Leukocyte recruitment in response to inflammation. Cytokines released in response to inflammatory stimuli, such as infection, injury, allergen, or tumor, prompt endothelial cells to express leukocyte adhesion molecules including P-selectin and E-selectin. Initial capture occurs when these molecules bind ligands on circulating leukocytes such as P-selectin glycoprotein ligand-1 (PSGL-1) or E-selectin ligand-1 (ESL1). Leukocytes “roll” on these receptors and slow, allowing time for additional ligands on leukocytes to firmly adhere to the endothelium via receptors such as intercellular adhesion molecule (ICAM) 1 and 2. Leukocytes then transmigrate through the endothelium and toward inflammatory stimuli (chemotaxis). (d) Endothelial interactions and primary hemostasis. Upon vessel injury the endothelium rapidly adopts a procoagulant profile, secreting endothelin (which promotes local vasoconstriction), and releasing VWF which binds circulating platelets via their GP1B receptors. VWF is also expressed on subendothelial collagen and is exposed by injury. Platelets “carpet” the endothelium and roll forward until they slow and firmly adhere to exposed collagen. Platelet activation then occurs, which leads platelets to change shape, degranulate, and aggregate, forming the platelet plug of primary hemostasis.
