Abstract
Compared to non-microprocessor knees, the C-Leg microprocessor knee (MPK) is bioenergentically and economically more efficient and safer for transfemoral amputation (TFA) patients. The Genium MPK has demonstrated improvements in perceived function, knee kinematics, and physical functional performance compared to C-Leg. Clinical and health economic analyses have not been conducted with the Genium knee system. The purpose of this study was to determine if laboratory determined benefits of Genium are detectable using common clinical assessments and if there are economic benefits associated with its use. This study utilized a randomized AB crossover study with 60 d follow-up including cost-effectiveness analysis. Twenty TFA patients tested with both knees in mobility and preference measures. Incremental cost-effectiveness ratios (ICER) were calculated based on performance measures. Stair Assessment Index scores improved with Genium. Mean stair completion times and descent stepping rate were not different between knees. Stair ascent stepping rate for C-Leg was greater compared with Genium (p = 0.04). Genium use decreased Four square step test completion time and increased functional level and step activity (p ≤ 0.05). Further, Genium use improved (p ≤ 0.05) function and safety in three out of five Activities of Daily Living (ADL) survey domains. Finally, more subjects preferred Genium following testing. Functional measures were used to calculate ICERs. ICER values for Genium fall within established likely-to-accept value ranges. Compared with C-Leg, Genium use improved stair walking performance, multi-directional stepping, functional level, and perceived function. In this group of community ambulators with TFA, Genium was preferred, and, while more costly, it may be worth funding due to significant improvements in functional performance with ADLs.
Keywords: Amputee mobility predictor, Four square step test, Gait, Incremental cost-effectiveness ratio, Physical therapy, Preference, Rehabilitation, Stair assessment index, StepWatch
INTRODUCTION
Compared to non-microprocessor prosthetic knee systems (NMPK), the C-Leg microprocessor knee system (MPK; Otto Bock Healthcare, Duderstadt, Germany) is more efficient in terms of gait bioenergentics and health-economic measures as well as safer for persons with transfemoral amputation (TFA) (1). Recently, the Genium MPK system has demonstrated improvements in perceived functional measures (2), knee kinematics (3), and physical functional performance (4) compared to C-Leg. Clinimetric assessment and health economic analysis have not yet been conducted. Therefore, the purpose of this study was to determine if laboratory determined benefits of the Genium are detectable using common clinical outcome assessments. A second purpose was to determine if there are health-economic benefits associated with use of the Genium knee system.
METHODS
The study was approved by the University of South Florida’s Institutional Review Board and listed in a federal clinical trial registry. Subjects gave informed consent prior to participation in the study.
Study Design Overview
A randomized experimental crossover design, where TFA patients used Genium and C-Leg MPK systems, was used. Subjects tested on both knee systems in random order separated by an accommodation period of >2 weeks to <3 months, depending upon when they determined their readiness to test. Subjects were assessed in a university clinical laboratory setting using common clinical outcome measures as described below.
Randomization, Eligibility, and Interventions
Subjects had to be unilateral TFA patients from any etiology and not have impairments that adversely impacted their gait beyond their amputations (e.g., cardiopulmonary, orthopedic impairments). Additionally, subjects had to be C-Leg users for ≥1 year prior to enrollment. An electronic random number generator was used to assign subjects (off site) to either continue with the C-Leg or be fit with a Genium MPK at recruitment. The study prosthetist was notified of each subject’s assigned condition via telephone on the day of the subject’s knee fitting. All fittings and adjustments were performed by the same study prosthetist, who was state-licensed and certified by the American Board for Certification in Orthotics, Prosthetics, and Pedorthics as well as by Ottobock Healthcare for fitting both C-Leg and Genium MPK systems. Subjects’ prosthetic sockets and suspension systems were not changed for the experiment’s duration to reduce confounding effects from fitting and acclimation issues. Subjects were fit with an Ottobock Trias (standard height) or Axtion (low profile) prosthetic foot, based on limb length, for use over the study duration. Manufacturer specifications were used to set componentry alignment and were verified using the LASAR (Ottobock, Duderstadt, Germany) alignment system.
Fitting and Accommodation Periods
After enrollment, anthropometric and demographic data and the study foot were recorded. Knee fittings and alignment were conducted and settings recorded. Subjects were invited to return to the study prosthetist or physical therapist for adjustment, alignment, and training as many times as they wished to optimize fit, comfort, and function and to mirror real clinical practice and component prescription. Visits were counted and reasons for each visit recorded. All subjects, regardless of the knee system with which they began the study, received an initial training session from the study physical therapist for each knee system for training in transitional movements, obstacle crossing, ramps, stairs, speed variation, and variable surfaces. Portions of the study’s training techniques have been previously published (5,6).
The minimum accommodation period was two weeks. After this, subjects were contacted weekly to determine their ability to walk without personal assistance on 1) level ground, 2) inclines, 3) declines, 4) up & down stairs, and 5) on uneven ground. Subjects could contact investigators at any time after the two-week minimum to declare their readiness to physically demonstrate they had accommodated to their currently assigned knee and study foot. Subjects were considered accommodated after verbally acknowledging and physically demonstrating their ability to ambulate independently on all five of the previous terrains (7,8). Following accommodation, subjects were scheduled for initial data collection (phase A testing). Following initial testing, knee units were switched and the process repeated for the second data collection (phase B testing). Following the second data collection (phase B test), subjects were switched back into their C-Leg (original, pre-study knee). At this time, a third and final data collection (phase C testing) was administered 60 d following the second data collection. The third data collection (i.e., the 60 d follow-up) was administered via U.S. mail to subjects at their home addresses. Return of this survey marked the formal conclusion of subjects’ involvement in the study.
Testing and Outcomes
Objective Measures
Stair Assessment Index (SAI)
Subjects were asked to ascend and descend stairs compliant with the Americans with Disabilities Act (9) (four steps 17cm high × 28cm long × 91cm wide leading up to a platform with railing on both sides). Three trials ascending and three trials descending at a self-selected speed were timed using a stopwatch and video recorded. Stair assessment index (SAI) scores were determined later by two independent reviewers viewing the video recording using criteria outlined previously (7). The SAI is a stair gait evaluation instrument using a 13-point scale to determine gross motor pattern implementation of the subject and use of assistive devices (7,10). The SAI was found to have excellent inter-rater and intra-rater reliability for assessing both stair ascent and descent (11). Time to complete the test was recorded at data collection and SAI scores obtained from video review. Stepping rate was calculated by dividing the number of steps completed by time to complete the test.
Four Square Step Test (4SST)
The four square step test is a timed assessment of multi-directional stepping. Subjects step forward, backward, and to each side while stepping over canes oriented in a cross configuration to create four squares on the floor. In older adults, scores of ≥12 s are associated with fall risk, whereas in unilateral TTA patients, ≥24 s are associated with fall risk (12,13). Instructions were consistent with previous applications. Briefly, subjects were instructed to complete the test as quickly as possible but not to hop or jump over the canes. Three repeated trials were conducted and averaged to represent the subject’s final score. If a subject’s foot touched a cane, the trial was stopped and repeated until three successful trials were completed.
Amputee Mobility Predictor (AMP)
The AMP is a 21-item test of functional mobility used to determine a lower limb amputee’s ability to ambulate. AMP was shown to have moderate to strong concurrent validity with the six-minute walk test and the Amputee Activity Survey (14). Specific details of each item and test administration of the AMP have been described previously (14). The following is a synopsis of the mobility functions assessed by the AMP (14). Items 1 and 2 test the ability to maintain sitting balance. Items 3 through 7 test the ability to maintain balance while performing tasks of transferring from chair to chair and standing unchallenged. Items 8 through 13 test more challenging standing balance activities. Items 14 through 20 evaluate quality of gait and the ability to negotiate specific obstacles. Item 21 accounts for the use of particular assistive devices. Most AMP items offer three scoring choices: 0 indicates inability to perform the task, 1 indicates minimal level of achievement or that some assistance was required in completing the task, and 2 indicates complete independence or task mastery. The AMP test requires approximately 10 to15 min to administer and was administered by the study’s licensed physical therapist a single time at each data collection.
Step Activity Derived Functional Level (SAD-FL)
The Galileo cloud was accessed at https://galileo.orthocareinnovations.com (Orthocare Innovations, Mountlake Terrace, WA, USA), and subjects were registered in the cloud and the StepWatch device was programmed to start recording step activity. Subjects wore the StepWatch on the prosthetic limb’s lateral side just proximal to the approximate location of the anatomical ankle. The StepWatch recorded subjects’ step activity for a two-week period immediately prior to laboratory data collections. At the end of the two-week recording period, StepWatch data was uploaded into the Galileo cloud server. At the point of data upload, each subject’s body mass and the study physical therapist’s opinion of the subject’s functional level (i.e., Medicare K-level) was also entered into the Galileo software. Following upload, a report of step activity and functional level is generated. The report provides an estimated K-level (i.e., functional level) based on multiple factors, including cadence variability, potential to ambulate, ambulation requirement, and the clinician’s observation of functional level. Cadence variability includes the proportion of steps taken at low, medium, and high cadence rates. Potential to ambulate relates to the intensity of walking during minutes of activity with the highest number of steps taken. Ambulation requirement considers the energy exerted during walking. Additionally, the clinically observed K-level is included and all of these K-levels are averaged into an overall K-level that has one-tenth level precision. The report’s K-level was intended to be rounded to achieve the final K-level.
Perceptive Measures
The significance of patient input on prosthetic prescription, knee selection, and fabrication and its influence on successful outcomes is established (15). To circumvent some of the pitfalls associated with subjective data collection yet still include it because of the value of capturing participant input and preference, two methods were considered. The first was to use a functional survey previously deployed in this population (16). The second method was to directly query participants regarding their component preference, a method which has previously been described as having the ability to strengthen or refute other study findings (15). Finally, these subjective measures were administered at a 60 d follow-up after subjects were returned to their pre-study knee, which was the C-Leg, and followed the initial two data collections (one for each knee for the crossover). This is particularly important given that, historically, MPK studies have not offered a follow-up assessment.
Activities of Daily Living Survey
A questionnaire developed for a previous study (16) was used to survey subjects in activities of daily living (ADL) tasks (45 total items) divided into five activity categories: Personal Care and Dressing (four activities), Family and Social Roles, Leisure Time Activities (12 activities), Mobility and Transportation (19 activities), Health-related Exercise (four activities), and Other Activities (six activities). The individual ADL items are listed elsewhere (16). The survey has a portion for each comparative MPK system where subjects first rate the importance of ADLs and then rate the perceived difficulty and safety with the respective knee system. This was asked for each MPK at the respective test sessions for each knee. Finally, there is a third portion of the survey in which subjects are asked to subjectively compare the perceived difficulty and safety of performing the same 45 ADLs between the comparative MPK systems. This comparative survey was administered at a 60 d follow-up after the second (phase B) data collection. In this analysis, only the comparison of difficulty and safety were evaluated using an ordinal scale and non-parametric analysis consistent with survey’s authors (16). This provided insight into the difference in both functional ADL performance and safety between the two MPK systems from the patients’ perspective.
Preference
In order to capture true patient preference and exclude potential novelty effects or glitz bias (15), at the study’s conclusion (phase C test), subjects were asked which knee mechanism they preferred and would actually wish to continue using following the study’s conclusion. This measure was used to identify true subject preference regardless of the performance data. Subjects were asked four questions conducive to completing a 2 × 2 contingency table. Questions were: “Do you prefer and would you like to keep the C-Leg?” and “Do you reject and wish to stop using the C-Leg?” These were repeated for the Genium. Asked this way, subjects could ultimately choose to keep or reject either or both MPKs. Finally, subjects were asked, “If you could only keep either the Genium or the C-Leg, which would you prefer to keep as a permanent part of your prosthesis?”
Cost-Effectiveness
A previous report of the current randomized control trial analyzed function in activities of daily living using the Continuous Scale-Physical Functional Performance-10 assessment (CS-PFP-10), a measure shown to be valid, reliable, and sensitive to change in multiple diagnostic populations, including TFA patients (4,17-19). Incremental cost effectiveness ratios (ICER) were calculated using differences in scores for each of three domains (balance & coordination (BAL), upper body flexibility (UBF), and endurance (END)) that were significantly improved (p ≤ 0.05) when subjects used Genium compared with C-Leg on the CS-PFP-10 as source data for effects (denominator). Calculations for ICERs were conducted using the following equation:
The payor’s perspective was taken in order to understand if Genium use (new strategy) is cost-effective compared to the C-Leg (current practice) given the recent challenges with the reimbursement of advanced microprocessor prosthetic technologies. Private and federal sector prosthetic practitioners (i.e., expert opinion) were queried in terms of the differences reimbursed between the two study interventions. Because private sector practitioners commonly accept healthcare reimbursement from multiple payors, a considerable range of cost resulted. The range of differences in cost used for calculations was $30,000 and $55,000. ICERs were calculated in $5,000 increments across this range of reimbursement differences where the Genium is the more costly strategy. Assumptions used for ICER calculations included generalizability of the reported reimbursement across the U.S. given that practitioners were only queried from Florida. Another assumption is that discounting is built into the range of cost differences. An example is that some practitioners within the private sector receive volume purchasing discounts based on the size of their practice, and, further, federal sector practitioners may also receive discounted component costs. Uncertainty with the difference in performance was addressed by only using the domain score differences that were both improved and statistically significant from our previously published work (4). This was important given that Genium improved all domains of the CS-PFP-10, but not all domains were significantly improved. In terms of time horizon, ICERs were calculated based on the findings of the randomized clinical trial from which patients accommodated over a period <90 d. Therefore, ICER values were then projected over five years to project value over a common life expectancy for an MPK then amortized across this five-year period.
Statistical Analyses
Statistical analyses were performed with IBM SPSS (v21, Armonk, NY, USA). Data were compiled into a database, assessed for completeness, and descriptive analyses were performed (i.e., frequency, central tendency, variance). The Shapiro-Wilk test was used to determine if data were normally distributed. Between-knee comparisons were made for each dependent variable. Normally distributed continuous data were assessed using dependent samples t tests (i.e., 4SST times). For ordinal data or data that were not normally distributed, a Related-Sample Wilcoxon Signed Rank test was used. This test evaluates the distribution of the difference between related samples rather than the difference between means. The a priori level of significance was p ≤ 0.05. Cohen’s d was then calculated to represent the magnitude of effect size between knee conditions for continuously scaled data when statistically significant differences were present. Cohen’s d was interpreted as d = 0.2 representing a small effect, 0.5 representing a medium effect, and 0.8 representing a large effect (20). Investigators adopted the “last observation carried forward” or “next observation carried backward” methods as the study’s a priori intention-to-treat plan (21,22). To determine if there were significant differences for preference, chi-squares/Fishers exact tests were used (i.e., categorical variables (prefer/not prefer, accept/ reject)).
RESULTS
Subject Demographics
Twenty TFA subjects (n = 20) participated and completed all study tasks with complete data from both MPK systems. Most subjects were male (80%) with a mean (SD) age of 46.5 years (14.2) and BMI of 26.4 kg/m2 (4.2). The majority were employed (55%), 25% were governmentally classified as “disabled,” and the remaining 20% were students or retired. All subjects were independent, unlimited community ambulators (Medicare functional classification level 3). Mean time since amputation was 17.7 years (15.6), and amputation etiology was predominantly traumatic (70%) followed by malignancy (20%) and peripheral vascular disease (10%). Mean relative residual limb length (SD) was 70% (30%) of the sound side femur, and the mean hip flexion contracture was 12.8° (7.7) as measured with a manual goniometer in the Thomas test position. A variety of prosthetic sockets (e.g. ischial ramus containment, ischial support, subischial, quadrilateral) and suspension systems (e.g. locking liners, suction, elevated vacuum) were used. Sagittal knee alignment was not different (p > 0.05) between knee systems.
SAI
Mean and median SAI scores for trials one, two, and three using C-Leg during stair ascent were 5.6, 6.0, and 6.3 and 5, 6, and 6, respectively. Corresponding scores for Genium during stair ascent were 9.7, 9.9, and 10.1 with a median score of 11 for all trials. These results were significantly different (p = 0.001) between knee systems. Mean and median SAI scores for trials one, two, and three using C-Leg during stair descent were 11.0, 10.3, and 11.2 with a median of 11 for all trials. Corresponding scores for Genium during stair descent were 12, 11.7, and 11.8 with a median score of 11 for all trials. These results were also significantly different between interventions (p = 0.04).
Mean (SD) times, in seconds, for stair ascent using C-Leg were 4.4 (1.5), 4.4 (1.4), and 4.5 (1.5) for trials one, two, and three, respectively. Corresponding times, in seconds, for Genium were 5.0 (1.0), 5.2 (1.6), and 4.7 (1.3). Mean (SD) times, in seconds for stair descent using C-Leg were 3.8 (1.1), 3.8 (1.0), and 3.7 (1.0) for trials one, two, and three, respectively. Corresponding times, in seconds, for Genium were 3.8 (1.0), 3.7 (0.8) and 3.6 (0.8). Mean differences for completion times were not significantly different.
With C-Leg, subjects ascended stairs at a mean (SD) rate of 1.1 steps/s (0.5) compared to a mean rate of 0.8 steps/s (0.2) with Genium. The stepping rate was significantly increased when using C-Leg (p = 0.04; medium effect size). For descent, the mean (SD) stepping rate with C-Leg was 1.2 steps/s (0.4) compared to 1.1 steps/s (0.2) when using Genium. The stepping rate for descent was not significantly different between knee systems.
4SST, AMP, SAD-FL
Results for the 4SST, AMP, and SAD-FL are shown in Table 1. Use of the Genium decreased time to complete the 4SST by 1.1 s. Functional performance increased by two points with Genium use as measured by the AMP and also by 0.2 points as measured by step activity derived functional level. These differences were all significantly improved (p ≤ 0.05) following accommodation and use of the Genium MPK.
Table 1.
Objective Measures: 4SST, AMP, and SAD-FL
| Test | C-Leg | Genium | p value | ||
|---|---|---|---|---|---|
| Central Tendency |
Variance |
Central Tendency |
Variance |
||
| 4SST | 12.2 | 3.3 | 11.1 | 3.4 | 0.04 |
| AMP | 42 | 33 to 45 | 44 | 39 to 46 | ≤0.001 |
| SAD-FL | 3.4 | 1.8 to 4.0 | 3.6 | 2.0 to 4.3 | 0.01 |
4SST is a 4 square step test. AMP is amputee mobility predictor. SAD-FL is step activity derived functional level. Central Tendency is mean (SD) for 4SST and is median (range) for all other tests. Statistical Significance is p ≤0.05. Effect size for the 4SST was small (d = 0.33).
Activities of Daily Living Survey
Results for the ADL survey are in Table 2. Genium use resulted in improvements (p < 0.05) in perceived function and safety in three of five of the domains queried in the ADL survey. Improved domains included: 1) Family and Social Roles, Leisure Time Activities, 2) Mobility and Transportation, and 3) Other Activities. No differences were identified in the remaining two domains of the ADL survey: Personal Care and Dressing and Health-related Exercise.
Table 2.
Activities of Daily Living Survey
| Domain | Functional Improvement | Safety |
|---|---|---|
| Personal Care and Dressing | ND | ND |
| Family and Social Roles, Leisure Time Activities |
Genium | Genium |
| Mobility and Transportation | Genium | Genium |
| Health-related Exercise | ND | ND |
| Other Activities | Genium | Genium |
ND is not diferent between MPK systems. When an MPK is listed (Genium or C-Leg), it was identifed by subjects to be either a functional improvement or safer when used with the activities of daily living in the respective domain (p ≤ 0.05).
Preference
There was a significant difference (p < 0.001; Fisher’s Exact Test given cell counts <5) between those who selected accept Genium (80.0% responses or 16/20 vs. 4/20 C-Leg accept) and those who selected reject C-Leg (65% or 13/20 vs. 1/20 who replied reject Genium). Some subjects seemed to be undecided or had some preference for both devices.
Cost-Effectiveness
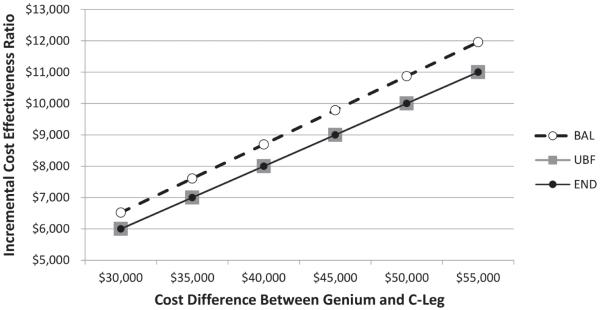
Subjects achieved significantly higher (p < 0.05) function with Genium use (4). Using these measures of function, incremental cost-effectiveness of Genium vs. C-Leg ranged from $6,000 to $6,522 per unit increase in function (END & UBF and BAL respectively) assuming a $30,000 difference in cost (Figure 1). Using these same measures of function, incremental cost-effectiveness of Genium vs. C-Leg ranged from $11,000 to $11,957 per unit increase in function (END & UBF and BAL respectively) assuming a $55,000 difference in cost. If these costs were divided across five equal annual payments (i.e., five-year service life), the annual cost per increase in function is $1,200 to $1,304 (assuming $30,000 increased cost) or up to $2,200 to $2,391. The total one-time reimbursed difference in cost divided into five equal annual payments (i.e., one payment per year for 5 years with no interest) is $6,000/year ($30,000 cost difference) or $11,000/year ($55,000 cost difference). These costs are not adjusted for inflation or discounting and are expressed in 2016 U.S. dollars. These costs also presume that each unit of functional increase occurs in isolation. However, this is not the case, as each of these units of functional gain occurred simultaneously (4), thereby increasing value.
Figure 1. Incremental cost effectiveness ratios for differences in cost between microprocessor knees based on functional improvements.
Incremental cost effectiveness ratios were determined based on the difference in cost of the interventions (Y axis), as a function of the ratio of the relative cost per unit of functional increase in three respective domains: balance (BAL), upper body flexibility (UBF), and endurance (END).
DISCUSSION
This study’s hypothesis was that laboratory determined benefits of Genium use previously identified (2,3,23-25) would translate into measurable improvements in common clinical outcome assessments as well. A second hypothesis was that, due to the increased functional benefits associated with Genium use, the technology could meet established thresholds acceptable to merit third-party reimbursement.
SAI, 4SST, AMP, and SAD-FL
Genium use resulted in significantly improved SAI scores and decreased stepping rate (medium effect size) while ascending stairs in a similar time. Further, Genium use improved SAI scores for stair descent with similar descent times and stepping rate. With Genium’s stair ascent mode, most subjects were able to use a step-over-step pattern as opposed to a skipping step pattern and were able to decrease handrail usage. The step-over-step pattern is more symmetrical and utilizes kinematic patterns more like those of non-amputees. Typical stair climbing patterns have demonstrated improved physiological costs relative to alternative stair gait patterns (26). Reduced energy demand resulting from an improved stair gait pattern is potentially corroborated by the significant reduction in stepping rate with use of the Genium. The reduction in handrail use is also clinically relevant, as it was used in recent Medicare/Medicaid Local Coverage Determination verbiage as a suggested factor in functional level determination with the use of a cane limiting a prosthetic user to the K2 level, which does not allow for reimbursement of MPK components (27).
Although median SAI scores were identical between knees for stair descent, Genium allowed all subjects to perform a step-over-step descent without assistive device use. The maximum score for C-Leg was 11 during descent with a minimum score of three. This range of scores likely contributed to the statistical difference between knees but suggests improved consistency with the Genium system. Although there was no aggregate difference in time or stepping rate for descent between MPK systems, the gross motor pattern implemented (i.e., SAI scores) and decreased assistive device use with Genium further suggests that engineering advancements included in the Genium allowed for increased stability and balance compared to C-Leg as has been previously identified in other functional activities.
The decreased time to complete the 4SST (small effect size), a test of multi-directional stepping, is also consistent with the notion of improved balance suggested here by improved stair climbing abilities resulting from Genium use. Beyond this, previous tests of function in ADLs demonstrated improvements in multi-directional stepping (4). Most notably, rearward directed steps and small steps were improved (4,25). In a previous test involving moving laundry from a washer to a dryer, a task involving small side steps and rearward steps, significant improvements were observed (4), which are consistent with the 9% improvement in 4SST times recorded in this study.
Two means were used to assess functional level in this study. One was the AMP test, a test of transitional movement, stepping and balance (14) and the second was a functional level based on step activity. Tasks improved on the AMP test associated with Genium use included stair gait, obstacle crossing, and variable cadence. Conversely, most subjects were unable to achieve single-limb balance on the prosthesis regardless of which MPK they were using. The 2.0 point increase observed with Genium use in this study did not reach the minimal detectable change (MDC) value of 3.4 points for the AMP reported by Resnik and Borgia (28). Because the difference in AMP scores did not reach the MDC, it could be argued that true change may not have occurred relative to this specific test. However, Resnik and Borgia’s sample was of mixed amputation level. Further, AMP scores were statistically significantly different, and key functions were improved with Genium use (e.g., stair gait, variable cadence, and obstacle crossing). Additional issues worthy of consideration include the test’s use of interval level data and the wide range of task difficulty.
Previous study has shown that TFA patients tend to not alter their usual living patterns and step activity based solely on receipt of a new knee system (29). However, in this study, there was a significant increase in functional performance based on step activity. These changes in activity took place while participants were in their community or home environments, as lab steps were not counted. Thus, subjects had sufficiently increased steps, steps/bout, or step intensity to elevate their step activity derived functional levels. It is possible that subjects took these additional steps or changed their stepping routine in part due to participation in the study while attempting to accommodate with the study knee. From an activity perspective, this is desirable and yielded positive changes in function as previously noted in stair and multi-directional stepping function. Further supporting true change is the fact that the AMP test also measured a significant increase in functional level using parameters other than step activity. While this was true for both functional level measurements, neither functional measure changed to a higher functional level. Instead, subjects’ function increased significantly within their respective functional level. For instance, the group did not change from limited community to unlimited community ambulation.
ADL Survey and Preference
In addition to the objective functional measures described above, perceptive measures were increased or unchanged. Subjectively, there were no decreased functional measures or decreased perceptions of safety associated with use of the Genium. It is note-worthy that Genium increased safety and function in areas requiring community engagement (e.g., family, social and leisure roles, mobility and transportation) because this is consistent with the type of subject enrolled in the study who was (on average) in their mid-forties and active in the community. The fact that there was no difference in self-care suggests C-Leg may be meeting many of these needs. Conversely, the lack of difference in exercise function could be that both components still leave room for improvement. Interestingly, there was a significant difference in preference among this group of unlimited community ambulators. The magnitude of difference was comparable to that previously observed when a more functionally diverse subject group was asked their preference between NMPKs and the C-Leg (15). It is unclear if preference would be so strong in more functionally diverse patient groups or patients more homogeneously located at higher or lower ends of the functional spectrum.
Cost-Effectiveness
In this study, using functional measures, the ICER for reimbursing Genium vs. C-Leg ranged from $6,000 to $6,522 per unit of functional increase assuming a $30,000 intervention cost difference. Assuming the component would not require replacement for five years, this cost would likely amortize over the five-year service period (i.e., five equal annual payments with no interest). Thus, the estimated annual cost for this functional increase is $1,200 to $1,304. Alternatively, depending upon discounting and other factors, if the cost difference between the interventions is higher, at $55,000, the ICER for reimbursing Genium vs. C-Leg ranges from $11,000 to $11,957 per unit of functional increase. Again this amortizes to $2,200 to $2,391 annually over a five-year service period. When the C-Leg was initially introduced as an alternative to NMPKs, the initial cost was notably higher. In time, it was proven that while C-Leg was more expensive, it was worth funding for numerous reasons, including reducing falls, reducing lost time for prosthetic maintenance, and others (1). In the case of the Genium, in higher-functioning patients, it is clear that higher function in ADLs, quality of life, and functional level are all domains that realize gains that are above what the C-Leg can provide (2-4,16,24,25). In this sense, our estimates of incremental cost-effectiveness may be conservative, as our ICERs are expressed in terms of a single functional measure.
Limitations
This study lacked blinding, which is difficult to incorporate in rehabilitation research for safety and ethical reasons. The findings are based upon the experiences and performance of patients who may not be representative of the entire TFA population, as these subjects were unlimited community ambulators who lost their limbs predominantly due to trauma and malignancy. Regarding the cost effectiveness portion of the study, the patient and societal perspectives were not considered in the economic analysis. Future studies need to carefully consider the impact of improvement in functional measures on productivity. Our cost-effectiveness analysis only considered improvement in specific functional measures individually and not improvement simultaneously in these measures, which likely yielded conservative estimates. Future studies will need to consider overall health-related quality of life and quality-adjusted life years.
CONCLUSION
Accommodation and use of the Genium knee system compared with C-Leg improved stair walking performance, multi-directional stepping, functional level, and perceived function. Genium was also preferred compared to C-Leg in this group of high-functioning community ambulators with unilateral transfemoral amputation. Finally, Genium is a more costly microprocessor knee system but, in this group of patients, is worth funding due to significant differences in functional performance with activities of daily living.
ACKNOWLEDGMENTS
Contents of this manuscript represent the opinions of the authors and not necessarily those of the U.S. Department of Defense, U.S. Department of the Army, U.S. Department of Veterans Affairs, or any academic or health care institution. Authors declare no conflicts of interest. This project was funded by:
The Florida High Tech Corridor/USF Connect (Grant #FHT 10-26).
Otto Bock Healthcare (USF Grant #6140101200).
The National Institutes of Health Scholars in Patient Oriented Research (SPOR) grant (1K30RR22270).
REFERENCES
- 1.Highsmith MJ, Kahle JT, Bongiorni DR, Sutton BS, Groer S, Kaufman KR. Safety, energy efficiency, and cost efficacy of the C-Leg for transfemoral amputees: a review of the literature. Prosthet Orthot Int. 2010;34:362–77. doi: 10.3109/03093646.2010.520054. [DOI] [PubMed] [Google Scholar]
- 2.Highsmith MJ, Kahle JT, Miro RM, Mengelkoch LJ. Perceived differences between the Genium and the C-Leg microprocessor prosthetic knees in prosthetic-related function and quality of life. Technol Innov. 2014;15(4):369–75. [Google Scholar]
- 3.Lura DJ, Wernke MM, Carey SL, Kahle JT, Miro RM, Highsmith MJ. Differences in knee flexion between the Genium and C-Leg microprocessor knees while walking on level ground and ramps. Clin Biomech (Bristol, Avon) 2015;30:175–81. doi: 10.1016/j.clinbiomech.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 4.Highsmith MJ, Kahle JT, Miro RM, Cress ME, Lura DJ, Quillen WS, Carey SL, Dubey RV, Mengelkoch LJ. Functional performance differences between the Genium and C-Leg prosthetic knees and non-Amputees. J Rehabil Res Dev. Forthcoming. doi: 10.1682/JRRD.2014.06.0149. [DOI] [PubMed] [Google Scholar]
- 5.Highsmith MJ, Kahle JT, Lewandowski AL, Kim SH, Mengelkoch LJ. A method for training step-over-step stair descent gait with stance yielding prosthetic knees. J Prosthet Orthot. 2012;24:10–5. [Google Scholar]
- 6.Highsmith MJ, Kahle JT, Lura DJ, Lewandowski AL, Quillen WS, Kim SH. Stair ascent and ramp gait training with the Genium knee. Technol Innov. 2014;15(4):349–58. [Google Scholar]
- 7.Hafner BJ, Willingham LL, Buell NC, Allyn KJ, Smith DG. Evaluation of function, performance, and preference as transfemoral amputees transition from mechanical to microprocessor control of the prosthetic knee. Arch Phys Med Rehabil. 2007;88:207–17. doi: 10.1016/j.apmr.2006.10.030. [DOI] [PubMed] [Google Scholar]
- 8.Highsmith MJ. Microprocessor knees: considerations for accommodation and training. J Prosthet Orthot. 2013;25:60–4. [Google Scholar]
- 9.US Department of Justice . ADA standards for accessible design. US Department of Justice; Washington (DC): 2010. [Google Scholar]
- 10.Buell NC, Willingham LL, Allyn KJ, Hafner BJ, Smith DG. Evaluation of gait style to ascend and descend stairs for lower limb amputees. In: Boone D, editor. Proceedings of the 11th World Congress of the International Society of Prosthetics and Orthotics; Hong Kong National Society of the International Society for Prosthetics and Orthotics; Hong Kong. Aug 1-6, 2004. 2004. p. 367. Hong Kong. [Google Scholar]
- 11.Highsmith MJ, Kahle JT, Kaluf B, Miro RM, Mengelkoch LJ, Klenow TD. Psychometric evaluation of the HAI and SAI in transfemoral amputees using a microprocessor knee system. Technol Innov. Forthcoming. 2016 Aug; doi: 10.21300/18.2-3.2016.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dite W, Connor HJ, Curtis HC. Clinical identification of multiple fall risk early after unilateral transtibial amputation. Arch Phys Med Rehabil. 2007;88:109–14. doi: 10.1016/j.apmr.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 13.Dite W, Temple VA. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil. 2002;83:1566–71. doi: 10.1053/apmr.2002.35469. [DOI] [PubMed] [Google Scholar]
- 14.Gailey RS, Roach KE, Applegate EB, Cho B, Cunniffe B, Licht S, Maguire, Nash MS. The amputee mobility predictor: an instrument to assess determinants of the lower-limb amputee’s ability to ambulate. Arch Phys Med Rehabil. 2002;83:613–27. doi: 10.1053/apmr.2002.32309. [DOI] [PubMed] [Google Scholar]
- 15.Kahle JT, Highsmith MJ, Hubbard SL. Comparison of nonmicroprocessor knee mechanism versus C-Leg on Prosthesis Evaluation Questionnaire, stumbles, falls, walking tests, stair descent, and knee preference. J Rehabil Res Dev. 2008;45:1–14. doi: 10.1682/jrrd.2007.04.0054. [DOI] [PubMed] [Google Scholar]
- 16.Kannenberg A, Zacharias B, Mileusnic M, Seyr M. Activities of daily living: Genium bionic prosthetic knee compared with C-Leg. J Prosthet Orthot. 2013;25:110–7. [Google Scholar]
- 17.Cress ME, Buchner DM, Questad KA, Esselman PC, deLateur BJ, Schwartz RS. Continuous-scale physical functional performance in healthy older adults: a validation study. Arch Phys Med Rehabil. 1996;77:1243–50. doi: 10.1016/s0003-9993(96)90187-2. [DOI] [PubMed] [Google Scholar]
- 18.Cress ME, Petrella JK, Moore TL, Schenkman ML. Continuous-scale physical functional performance test: validity, reliability, and sensitivity of data for the short version. Phys Ther. 2005;85:323–35. [PubMed] [Google Scholar]
- 19.Highsmith MJ, Kahle JT, Miro RM, Cress ME, Quillen WS, Carey SL, Dubey RV, Mengelkoch LJ. Concurrent validity of the continuous scale physical functional performance-10 (CS-PFP-10) test in transfemoral amputees. Technol Innov. Forthcoming. 2016 Aug; doi: 10.21300/18.2-3.2016.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen J, editor. Statistical power analysis for the behavioral sciences. 2nd Erlbaum; Hillsdale (NJ): 1988. [Google Scholar]
- 21.Buhi ER, Goodson P, Neilands TB. Out of sight, not out of mind: strategies for handling missing data. Am J Health Behav. 2008;32:83–92. doi: 10.5555/ajhb.2008.32.1.83. [DOI] [PubMed] [Google Scholar]
- 22.Kenward MG, Molenberghs G. Last observation carried forward: a crystal ball? J Biopharm Stat. 2009;19:872–88. doi: 10.1080/10543400903105406. [DOI] [PubMed] [Google Scholar]
- 23.Highsmith MJ, Kahle JT, Lura DJ, Dubey RV, Carey SL, Quillen WS, Mengelkoch LJ. Short and mid-distance walking and posturography with a novel microprocessor knee. Technol Innov. 2014;15(4):359–68. [Google Scholar]
- 24.Bellmann M, Schmalz T, Ludwigs E, Blumentritt S. Stair ascent with an innovative microprocessor-controlled exoprosthetic knee joint. Biomed Tech. 2012;57:435–44. doi: 10.1515/bmt-2011-0029. [DOI] [PubMed] [Google Scholar]
- 25.Bellmann M, Schmalz T, Ludwigs E, Blumentritt S. Immediate effects of a new microprocessor-controlled prosthetic knee joint: a comparative biomechanical evaluation. Arch Phys Med Rehabil. 2012;93:541–9. doi: 10.1016/j.apmr.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 26.Shiomi T. Effects of different patterns of stair-climbing on physiological cost and motor efficiency. J Hum Ergol. 1994;23:111–20. [PubMed] [Google Scholar]
- 27.NHIC, Corp . Proposed/Draft Local Coverage Determination (LCD): Lower limb prostheses (DL33787) NHIC, Corp; Hingham (MA): 2015. A CMS Contractor. Contract #16003. [accesse 2016 Aug 12]. http://www.amputee-coalition.org/ content/documents/medicare-alert-2015/doc_LLP_Draft_LCD_071615.pdf. [Google Scholar]
- 28.Resnik L, Borgia M. Reliability of outcome measures for people with lower-limb amputations: distinguishing true change from statistical error. Phys Ther. 2011;91:555–65. doi: 10.2522/ptj.20100287. [DOI] [PubMed] [Google Scholar]
- 29.Klute GK, Berge JS, Orendurff MS, Williams RM, Czerniecki JM. Prosthetic intervention effects on activity of lower-extremity amputees. Arch Phys Med Rehabil. 2006;87:717–22. doi: 10.1016/j.apmr.2006.02.007. [DOI] [PubMed] [Google Scholar]