Abstract
Atrial Fibrillation (AF) is a highly prevalent heart rhythm disturbance, often associated with underlying (cardio)vascular disease. Due to this the management of AF is often complex and current practice calls for a more comprehensive, multifactorial and patient-centred approach. Therefore an Integrated Chronic Care approach in AF was developed and implemented in terms of a nurse-led specialized outpatient clinic for patients with AF. A randomised controlled trial comparing the nurse-led approach with usual care demonstrated superiority in terms of cardiovascular hospitalization and death as well as cost-effectiveness in terms of Quality Adjusted Life Years (QALYs) and life years, in favour of the nurse-led approach. Implementing such approach can be difficult since daily practice can be persistent. To highlight the importance of integrated care wherein the nurse fulfils a significant role, and to provide a guide in developing and continuing such approach, this paper presents the theoretical framework of the AF-Clinic based on the principles of the Taxonomy for Integrated Chronic Atrial Fibrillation Management.
Introduction
Atrial fibrillation (AF) is a highly prevalent heart rhythm disturbance, associated with an increased risk of thromboembolic events, and often accompanied by underlying heart disease.[1,2] Since recurrences in AF are most likely the arrhythmia is considered a chronic condition. The management of AF is a complex process, not only focussing on the arrhythmia (rate or rhythm control) but also on detection and treatment of associated cardio(vascular) diseases and prevention of thromboembolic events. Although international evidence based guidelines are available,[3,4] prior research demonstrated that guideline-adherent management of AF throughout Europe is suboptimal,[5,6] leading to increased morbidity and mortality in these patients. The prevalence of AF is estimated at 2-3% in general population, accounting for 33.5 million patients globally.[7] From a practical and logistical point of view, it is worth mentioning that AF prevalence is age-related[8] and due to an aging population it is expected that the number of AF patients will rise dramatically in the near future.[2,9] The prognosis is set on a 3-fold multiplication of the prevalence rate until 2050, accounting for 12.1 million AF patients in the US alone.[10] This evolution will go hand in hand with capacity shortcomings in providing health care, increasing waiting lists, limited accessibility to care, extremely high healthcare costs, and consequently further fragmentation of healthcare.[11] In short, current practice calls for a more comprehensive AF management approach. There is a need for changing the routine delivery of AF care through concepts of integrated and coordinated care management including principles of patient-centred care and collaborating multidisciplinary teams. In fact, it has been demonstrated that involving nurses in the care for specific patient groups improves patient outcomes,[12-15] demonstrating the importance of a multidisciplinary approach to care. In daily practice such approaches have scarcely been established in AF-care yet.
As a first response to redesign AF management, an integrated chronic AF approach was developed and implemented in the Maastricht University Medical Centre (MUMC) in terms of a specialized nurse-led outpatient clinic (AF-Clinic).[16] This clinic integrates significant care components and focusses on the collaboration between important disciplines and involving patients in the care process, following a patient-centred approach. Based on this approach recognized experts in the field advocate for nurse-coordinated management in AF and outline the rationale and fundamentals of such management approach.[17]
In a proved intervention as presented here, accountability and monitoring its performance and impact is essential. To this end, qualitative indicators in terms of guideline recommendations and process variables as well as the intended clinical effects of the intervention, were defined prior to the implementation of the AF-Clinic.[16] Hence, this integrated approach demonstrates that integrating significant components and evaluable indicators can contribute to more efficient care processes and improved patient outcomes. This reflects the aim of this paper which is to advocate for integrated chronic AF management and illustrate its practicability by presenting the AF-Clinic as a best practice example.
Redesigning Health Care As A Theoretical Framework In Developing Integrated Care: An Overview
The increasing prevalence of chronic diseases over the past decades, the associated extremely high healthcare costs and the fragmented nature of care for chronic patients, contributed to increased awareness of the necessity to reorganize medical treatment for chronic illness[18] Disease management programs were considered suitable for this, since potential benefits of disease management may include improved health outcomes, greater patient satisfaction, better quality of life, and reduced healthcare costs.[18,19] However, standardization was lacking (e.g. a specific definition of disease management was missing and there was a broad variety in existing disease management models). Although disease management programs were disease specific from the start, their focus was mainly to save money associated with onesize fits all organisation of care. Consequently, in the initial programs patients often received care that they actually did not want or need[20] In addition, long term beneficial effects were lacking, both concerning health outcomes as well as costs.[21,22]
Chronic Care Model
As a response to these disease indiscriminate management programs, the Chronic Care Model (CCM) was developed to contribute to improve patient outcomes by changing the routine delivery of care. Wagner et al. advocate the provision of care by fusion of six interrelated elements, in order to deliver patient-centred, evidence-based care.[23,24] The CCM was developed as a synthesis of the best available evidence of system changes needed to improve the quality of disease management, and covering:
The CCM pursues high quality management of chronic diseases, by focussing on interrelated elements including self-management support, delivery system design, decision support, clinical information systems, health care organization, and community resources.[27] These elements are meant to provide a practical system for restructuring the management of chronic care. By coordinating activities in primary care rather than focusing on the roles of specific personnel, the CCM aims to improve organizational and health outcomes.[21,23,24] This ‘integrated approach to care’ enables to address overall healthcare efficiency (process) and effectiveness (impact),[28] which is particularly important for multi-problem patients with high-risk conditions like patients with AF.
The Four Pillars of Integrated Chronic Care Management in Atrial Fibrillation
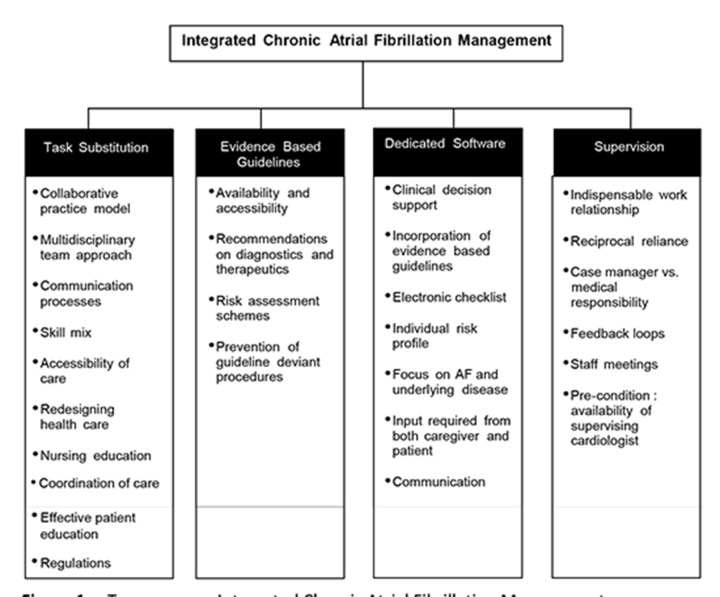
Based on the CCM, the integrated chronic care approach in AF is defined by four essential pillars, which together form the comprehensive, integrated approach.[23,24] The approach consists of a nurse-led, guideline-based, software supported outpatient clinic, named the AF-Clinic. The approach is schematically arranged in the Taxonomy of Integrated Chronic Atrial Fibrillation Management (Figure 1).
Figure 1. Taxonomy on Integrated Chronic Atrial Fibrillation Management.
Task Substitution
The increasing number of chronically ill patients, the changing consumer expectations and the limited capacity of resources and health care costs are the main drivers for task substitution from physicians to allied professionals.[29,30] Tasks that used to be reserved for medical doctors are now performed by nurse specialists, based on an efficient skill mix – identified care needs of AF population matched to the staff available in the AF-Clinic – and a multidisciplinary team approach.[31] In the literature the effectiveness of this principle was demonstrated in a variety of studies. The findings demonstrate a larger but more judicious use of resources in nursing care (e.g. requesting more diagnostic tests) and the duration of visits to the nurse are significantly longer – but qualitatively different – compared to physicians.[29] Such approach wherein nurses and physicians work closely together is more likely to provide effective patient education and the care is easily accessible, than in practices where physicians are working alone.[30,32]
Task substitution is an important pillar of the integrated chronic care approach. The fact that several disciplines work together in a collaborative practice model can be interpreted in terms of redesigning health care. The nurse specialist has a leadership role in managing AF, is highly trained and educated, responsible for the coordination of continued care, operating largely independently and consulting the supervising cardiologist in case tasks go beyond the traditional borders of the nursing profession.[33] This requires significant communication processes between both disciplines. As a consequence of task substitution, professional roles are changing and allied professional roles have been extended to the medical domain. The Netherlands Law regarding Professions in the Individual Health Care (Wet BIG)[34] has been changed (by adding article 36a) to create a legal basis for assigning an independent competence for physician associates and nurse specialists to perform restricted medical actions like prescribing medication or performing elective electrical cardioversions.[35,36] These new regulations are in effect, but content and practicability are as yet not sufficiently clear.[37] Obviously, their dissemination needs time.[36,38]
Evidence Based Guidelines
The importance of guideline adherence in the management of AF might be obvious, but prior research demonstrated significant gaps between the evidence-based guidelines on the management of AF and daily practice.[5,6,39,40] Considering the enormous attention given to the guidelines by stakeholders, on websites, in research and publications, and also taking into account the improved accessibility, the availability of pocket versions, and the regular revisions of guidelines in the last decade, one may expect an excellent adherence to guideline recommendations among health care providers these days. In addition, the use of risk assessment schemes is recommended in the guidelines. A remarkable example is the appropriate use of oral anticoagulation conform the individual stroke risk analysis based on the CHADS2-score[41] and CHA2DS2-VASc scores,[42] as demonstrated in the AF-Clinic.[43]
Dedicated Software
The use of clinical decision support technology in patient care, incorporating evidence based guidelines, and primarily used by care providers, has grown tremendously in recent decades.[44-46] In heart failure, telemonitoring is a well-known example, in which the patient is the primary user, resulting in a reduction of heart failure related hospitalizations and death.[47] In AF, systems are marginally available to determine whether or not to prescribe guideline adherent oral anticoagulation in AF patients.[48] No alternatives are available that focus on the management of AF and the underlying diseases, in terms of guideline adherent diagnostics and therapeutics, and in which input is required from both patient and care provider. Therefore, the development of the dedicated knowledge software system within the AF-Clinic is regarded innovative. The decision support software, based on the current guidelines[3,49] is developed as an assisting tool throughout the care process for both the care provider (e.g. guidelineadherent checklist) and the patient (in order to provide tailormade care, active patient input is required). The system provides an individual patient risk profile and acts as an electronic checklist to ensure adherence to all diagnostic and therapeutic guideline recommendations. Moreover, it ensures a more complete approach by focussing on underlying cardiovascular diseases rather than treating the arrhythmia alone. An additional effect of using the software is that it stimulates and facilitates communication processes in the multidisciplinary team (e.g. discussing guideline deviant decisions) which also has a teaching effect.
Supervision
The multidisciplinary approach is built on the indispensable work relationship between cardiologists and nurse specialists, as these disciplines work closely together within the AF-Clinic. Both disciplines are in charge of care delivery to patients with AF, each in a specified role: the nurse specialist being the case manager and care provider, and the cardiologist being the supervising, and medically responsible health professional. The question always is, which discipline is most suited to provide the care the individual patient needs and at what time? Task substitution contributes to improved accessibility and quality of care, yet depends on additional expertise of medical specialists. Its expression may also be steered by down-to-earth financial incentives.[50] However that may be, the relationship between involved disciplines is based on reciprocal reliance, which is vital in revealing clinically relevant findings on which therapeutic decisions can be made. According to this, staff meetings and feedback loops are of vital importance and contribute to multidisciplinary communication processes. Moreover, the educational level and expertise of the nurse specialist as well as the duration and intensity of the relationship between stakeholders are critical success factors in nurse-led care. Both parties should feel safe to give and receive feedback, as this is an essential cornerstone in the integrated approach. Like in the aviation industry, pilot and co-pilot should cooperate and rely on each other to warrant a safe flight.[51] The same holds for the cardiologist and nurse specialist in the AF-Clinic to secure guideline-based decisions and justify reciprocally guidelinedeviant behaviour in order to provide the best available treatment strategy. In this respect, availability of the supervising cardiologist in this redesigned best practice model is of utmost importance.
Implementation of Integrated Care
Implementation of this type of care is often a complex process, which necessitates important changes to the traditional care processes. In fact, integrated care requires a redesign of daily practice. This will only be possible in a system that supports and facilitates the development and implementation of such an approach. On a practical level structural and organizational prerequisites are recommended to facilitate an integrated care approach.[52] This includes an adjustment of the vision of care (including change of professional roles, development of multidisciplinary teams, intensive patient involvement in care and decision making, and deliberately providing guideline-based management), availability and education of skilled personnel (e.g. a nurse specialised in AF and the presence of a supervising cardiologist, practical facilitation of the outpatient clinic and software support). The importance of implement integrated care activities on multiple levels has been described before. On the operational level it is necessary to (re)organize information flows including patient transfers between health care providers. To realize sustainability of integrated care it is necessary to achieve commitment of representatives on a strategic level, while on a macro level the need for performance indicators should be discussed.[53]
Clinical Implications
Patient Centred Care By Means Of Education And Activating Self-Management
AF awareness in patients is increasing since many websites, apps and other supporting tools are available. However, attention for patient education and self-management is often lacking in AF care, while self-care is considered essential in the management of chronic illness.[54] Not surprisingly, patient education is often not structured and therefore insufficiently provided in current practice. It is important to tailor education to the individual patient and his specific situation and abilities.[55] For this reason the nurse specialist in the AF-Clinic extensively informs patients and their carers about pathophysiology and symptoms of AF, possible complications, results of diagnostic tests and personalised treatment options. Also lifestyle management and how to achieve desirable goals is addressed. Moreover, there is a specific focus on activating self-management activities to demonstrate patients how they can contribute to their own care process. This is achieved by assessing patient capabilities for self-management, resulting in an individualized tailored approach matching the patients’ level, capacities and needs.[56]
Nurse-Led Care
Coordination of care is a significant precondition of the continuity of the care process. In the context of task substitution, nurse specialists are considered suitable professionals to coordinate continued care. Generally, in consulting hours with nurse specialists there is more time reserved for counselling and coordination of care, compared to consulting hours with the physician. Also, nursing education focusses on developing specific communication skills that are required in patient care. These skills might be underlying the fact that clinical outcomes of nurse-led care for specific patient groups are better compared to standard care.[30,57-60] In line with prior findings, the AF-Clinic study demonstrated that nurse-led integrated care is associated with improved outcomes in patients with AF. The challenge of integrated AF care in daily practice is therefore to coordinate the continuum of care across the relevant fields of interest. This requires simultaneously collaboration, differentiation and integration[61] which enables further development of the AF-Clinic concept (e.g. integration of primary care, emergency care). In line with the epidemiological evolution of AF, it is highly recommended to extend the integrated care approach beyond the hospital setting alone.
Guideline Adherence
Ten years ago the Euro Heart Survey on AF already demonstrated guideline deviant behaviour in the management of AF and related effects.[5,6] Recent observational research confirmed this behaviour and demonstrated guideline deviant behaviour in prescribing oral anticoagulation, despite the use of stroke risk scores.[40] Apparently the medical society didn’t adapt to research findings and practical guideline recommendations in the last decade. To overcome this issue, integrated care can be a solution in closing the gap between guidelines and daily practice. This is illustrated by the fact that in the AF-Clinic study only 83% of patients in the usual care received appropriate oral anticoagulation treatment compared to 99% of patients in the nurseled care group. As a consequence, a significant number of patients was not adequately protected against thromboembolic complications. A diagnostic guideline recommendation is to measure thyroid stimulating hormone levels at least once.[3,4] Notably, this procedure was performed in only half of the patients in the usual care (54%) versus 91% in the nurse-led care. These findings reason the fact that integrated chronic care prevents patients from receiving incomplete diagnostic and therapeutic management procedures.
Moreover, implementing dedicated software as an assisting tool in daily practice can be helpful in achieving this goal. This contributes to guideline adherent behaviour but also to downsizing the complexity of AF management. However, one should bear in mind to use the software as an assisting, navigating tool rather than blindly trust it. Clinical thinking is still an essential task of the professional in collaboration with the patient.
Effectiveness of Integrated AF Care
In a randomised controlled trial the AF-Clinic was compared with usual care (Clincaltrials.gov identifier NCT00753259).[16] The trial demonstrated superiority of this approach in terms of major cardiovascular events compared to usual care. The primary outcome – a composite endpoint of cardiovascular hospitalisation or cardiovascular death – occurred in 14.3% of patients in the integrated nurse-led approach versus 20.8% of patients receiving usual care, demonstrating a relative risk reduction of 35% in favour of the AFClinic. Moreover, adherence to guideline recommendations in AF management was significantly better in the nurse-led approach versus usual care; adherence to a maximum of six practical guideline recommendations was 82% vs 39% respectively (P<0.001).[43] Although quality of life improved over time in both groups, patients in the nurse-led approach demonstrated higher levels of AF-related knowledge[62] and were more satisfied with the treatment process.[11] In addition, the cost-effectiveness analysis of this study demonstrated this approach to be cost saving in terms of QALYs (0.009 QALY gain with a reduced cost of € 1109 per patient) and life years (0.02 life years gained with a reduced cost of € 735 per patient) compared to usual care and is therefore considered a cost-effective management strategy for patients with AF.[63] These results confirm the beneficial effects of an integrated care approach.
Research Implications
Research and Guidelines
Since the AF population is growing rapidly, the need for coordination of care within an integrated chronic care setting will be more and more important. The Taxonomy of Integrated Chronic AF Management can act as an important redesign-model to contribute in overcoming ‘the epidemic of this millennium’. Therefore widespread dissemination is needed as well as more clinical research in this area. Currently a multicentre randomized controlled trial in the Netherlands is ongoing to further investigate the effects of specialized AF-Clinics. This ‘IntegRAted CaRe for AF study (RACE-4) aims to include 1716 AF patients from 8 participating centres in the Netherlands and first results are expected in 2016.[64] Despite the current available data it is striking that the current guidelines in the management of AF[3] do not advocate integrated chronic care management yet, while one would have expected that opinion leaders are convinced about the approach by now. Especially in the light of new results that again demonstrate poor management in patients with AF, following the conservative approach.[40]
Many initiatives are undertaken to (re)structure daily practice,[17] but research is missing or still ongoing in this field. This strengthens the necessity of more research in the field of integrated AF management. Moreover, following Nolte et al.[65] the same holds for research to support the implementation of integrated care services. This includes provision of adequate finances to develop new care structures and to incorporate these into daily practice, and to create systems that enable patients to effectively self-manage their care, steered by supportive information technology.
Conclusions
To achieve successful integrated chronic care management as demonstrated in the AF-Clinic, it is vital to integrate significant components of care including patients, care providers, infrastructure, finance and research. The AF-Clinic is an example of a best practice model that contributes to efficient care processes and improved clinical outcomes. Given the growing patient population that goes hand in hand with an increasing demand for care and a growing burden of the health care system, necessitates expansion of this approach. Hence, we advocate to go beyond the outpatient borders, in order to create new or improve existing collaborative relationships and achieve sustainable healthcare for patients with AF. This is also reflected in research and innovation programs like Horizon 2020, which aims to break down barriers and create possibilities for research and innovation in Europe. The same holds for the Netherlands organisation for health services research and care innovation (ZonMW) presenting a research theme focussing on integrated care in order to create sustainable healthcare.
Disclosures
None.
References
- Camm A John, Kirchhof Paulus, Lip Gregory Y H, Schotten Ulrich, Savelieva Irene, Ernst Sabine, Van Gelder Isabelle C, Al-Attar Nawwar, Hindricks Gerhard, Prendergast Bernard, Heidbuchel Hein, Alfieri Ottavio, Angelini Annalisa, Atar Dan, Colonna Paolo, De Caterina Raffaele, De Sutter Johan, Goette Andreas, Gorenek Bulent, Heldal Magnus, Hohloser Stefan H, Kolh Philippe, Le Heuzey Jean-Yves, Ponikowski Piotr, Rutten Frans H. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur. Heart J. 2010 Oct;31 (19):2369–429. doi: 10.1093/eurheartj/ehq278. [DOI] [PubMed] [Google Scholar]
- Go A S, Hylek E M, Phillips K A, Chang Y, Henault L E, Selby J V, Singer D E. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001 May 9;285 (18):2370–5. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- Camm A John, Kirchhof Paulus, Lip Gregory Y H, Schotten Ulrich, Savelieva Irene, Ernst Sabine, Van Gelder Isabelle C, Al-Attar Nawwar, Hindricks Gerhard, Prendergast Bernard, Heidbuchel Hein, Alfieri Ottavio, Angelini Annalisa, Atar Dan, Colonna Paolo, De Caterina Raffaele, De Sutter Johan, Goette Andreas, Gorenek Bulent, Heldal Magnus, Hohloser Stefan H, Kolh Philippe, Le Heuzey Jean-Yves, Ponikowski Piotr, Rutten Frans H. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur. Heart J. 2010 Oct;31 (19):2369–429. doi: 10.1093/eurheartj/ehq278. [DOI] [PubMed] [Google Scholar]
- Fuster Valentin, Rydén Lars E, Cannom David S, Crijns Harry J, Curtis Anne B, Ellenbogen Kenneth A, Halperin Jonathan L, Le Heuzey Jean-Yves, Kay G Neal, Lowe James E, Olsson S Bertil, Prystowsky Eric N, Tamargo Juan Luis, Wann Samuel. ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation-executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients with Atrial Fibrillation). Eur. Heart J. 2006 Aug;27 (16):1979–2030. doi: 10.1093/eurheartj/ehl176. [DOI] [PubMed] [Google Scholar]
- Nieuwlaat Robby, Capucci Alessandro, Camm A John, Olsson S Bertil, Andresen Dietrich, Davies D Wyn, Cobbe Stuart, Breithardt Günter, Le Heuzey Jean-Yves, Prins Martin H, Lévy Samuel, Crijns Harry J G M. Atrial fibrillation management: a prospective survey in ESC member countries: the Euro Heart Survey on Atrial Fibrillation. Eur. Heart J. 2005 Nov;26 (22):2422–34. doi: 10.1093/eurheartj/ehi505. [DOI] [PubMed] [Google Scholar]
- Nieuwlaat Robby, Capucci Alessandro, Lip Gregory Y H, Olsson S Bertil, Prins Martin H, Nieman Fred H, López-Sendón José, Vardas Panos E, Aliot Etienne, Santini Massimo, Crijns Harry J G M. Antithrombotic treatment in real-life atrial fibrillation patients: a report from the Euro Heart Survey on Atrial Fibrillation. Eur. Heart J. 2006 Dec;27 (24):3018–26. doi: 10.1093/eurheartj/ehl015. [DOI] [PubMed] [Google Scholar]
- Wong Christopher X, Lau Dennis H, Sanders Prashanthan. Atrial fibrillation epidemic and hospitalizations: how to turn the rising tide? Circulation. 2014 Jun 10;129 (23):2361–3. doi: 10.1161/CIRCULATIONAHA.114.010073. [DOI] [PubMed] [Google Scholar]
- Heeringa Jan, van der Kuip Deirdre A M, Hofman Albert, Kors Jan A, van Herpen Gerard, Stricker Bruno H Ch, Stijnen Theo, Lip Gregory Y H, Witteman Jacqueline C M. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur. Heart J. 2006 Apr;27 (8):949–53. doi: 10.1093/eurheartj/ehi825. [DOI] [PubMed] [Google Scholar]
- Stewart S, Hart C L, Hole D J, McMurray J J. Population prevalence, incidence, and predictors of atrial fibrillation in the Renfrew/Paisley study. Heart. 2001 Nov;86 (5):516–21. doi: 10.1136/heart.86.5.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyasaka Yoko, Barnes Marion E, Gersh Bernard J, Cha Stephen S, Bailey Kent R, Abhayaratna Walter P, Seward James B, Tsang Teresa S M. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006 Jul 11;114 (2):119–25. doi: 10.1161/CIRCULATIONAHA.105.595140. [DOI] [PubMed] [Google Scholar]
- Hendriks JM. Integrated chronic care for patients with atrial fibrillation. Maastricht: Universitaire Pers Maastricht. 2013;0:0–0. [Google Scholar]
- Metzelthin Silke F, Daniëls Ramon, van Rossum Erik, Cox Karen, Habets Herbert, de Witte Luc P, Kempen Gertrudis I J M. A nurse-led interdisciplinary primary care approach to prevent disability among community-dwelling frail older people: a large-scale process evaluation. Int J Nurs Stud. 2013 Sep;50 (9):1184–96. doi: 10.1016/j.ijnurstu.2012.12.016. [DOI] [PubMed] [Google Scholar]
- Lambrinou Ekaterini, Kalogirou Fotini, Lamnisos Demetris, Sourtzi Panayota. Effectiveness of heart failure management programmes with nurse-led discharge planning in reducing re-admissions: a systematic review and meta-analysis. Int J Nurs Stud. 2012 May;49 (5):610–24. doi: 10.1016/j.ijnurstu.2011.11.002. [DOI] [PubMed] [Google Scholar]
- Tierney Stephanie, Cook Gary, Mamas Mamas, Fath-Ordoubadi Farzin, Iles-Smith Heather, Deaton Christi. Nurses' role in the acute management of patients with non-ST-segment elevation acute coronary syndromes: an integrative review. Eur J Cardiovasc Nurs. 2013 Jun;12 (3):293–301. doi: 10.1177/1474515112451555. [DOI] [PubMed] [Google Scholar]
- Laurant M, Harmsen M, Faber M, Wollersheim H, Sibbald B, Grol R. Revision of professional roles and quality improvement: a review of the evidence. London: The Health Foundation. 2010;0:0–0. [Google Scholar]
- Hendriks Jeroen M L, de Wit Rianne, Vrijhoef Hubertus J M, Tieleman Robert G, Crijns Harry J G M. An integrated chronic care program for patients with atrial fibrillation: study protocol and methodology for an ongoing prospective randomised controlled trial. Int J Nurs Stud. 2010 Oct;47 (10):1310–6. doi: 10.1016/j.ijnurstu.2009.12.017. [DOI] [PubMed] [Google Scholar]
- Berti Dana, Hendriks Jeroen M L, Brandes Axel, Deaton Christi, Crijns Harry J G M, Camm A John, Hindricks Gerhard, Moons Philip, Heidbuchel Hein. A proposal for interdisciplinary, nurse-coordinated atrial fibrillation expert programmes as a way to structure daily practice. Eur. Heart J. 2013 Sep;34 (35):2725–30. doi: 10.1093/eurheartj/eht096. [DOI] [PubMed] [Google Scholar]
- Krumholz Harlan M, Currie Peter M, Riegel Barbara, Phillips Christopher O, Peterson Eric D, Smith Renee, Yancy Clyde W, Faxon David P. A taxonomy for disease management: a scientific statement from the American Heart Association Disease Management Taxonomy Writing Group. Circulation. 2006 Sep 26;114 (13):1432–45. doi: 10.1161/CIRCULATIONAHA.106.177322. [DOI] [PubMed] [Google Scholar]
- Congressional Budget Office. An analysis of the literature on disease management programs. [cited 2014 March 10th]. Available from: http://www.cbo.gov/publication/16076. 2004;0:0–0. [Google Scholar]
- Coleman Katie, Austin Brian T, Brach Cindy, Wagner Edward H. Evidence on the Chronic Care Model in the new millennium. Health Aff (Millwood) 2009 Jan 7;28 (1):75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrijhoef HJ. Chronically ill are the future (in Dutch: Chronisch zieken hebben de toekomst), Inaugural Speech. Tilburg: Tilburg University. 2010;0:0–0. [Google Scholar]
- Mattke Soeren, Seid Michael, Ma Sai. Evidence for the effect of disease management: is $1 billion a year a good investment? Am J Manag Care. 2007 Dec;13 (12):670–6. [PubMed] [Google Scholar]
- Wagner E H, Austin B T, Von Korff M. Improving outcomes in chronic illness. Manag Care Q. 1996;4 (2):12–25. [PubMed] [Google Scholar]
- Wagner E H, Austin B T, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74 (4):511–44. [PubMed] [Google Scholar]
- Wagner E H, Davis C, Schaefer J, Von Korff M, Austin B. A survey of leading chronic disease management programs: are they consistent with the literature? Manag Care Q. 1999;7 (3):56–66. [PubMed] [Google Scholar]
- Bonomi Amy E, Wagner Edward H, Glasgow Russell E, VonKorff Michael. Assessment of chronic illness care (ACIC): a practical tool to measure quality improvement. Health Serv Res. 2002 Jun;37 (3):791–820. doi: 10.1111/1475-6773.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodenheimer Thomas, Wagner Edward H, Grumbach Kevin. Improving primary care for patients with chronic illness. JAMA. 2002 Oct 9;288 (14):1775–9. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- Kodner Dennis L. All together now: a conceptual exploration of integrated care. Healthc Q. 2009;13 Spec No ():6–15. doi: 10.12927/hcq.2009.21091. [DOI] [PubMed] [Google Scholar]
- Laurant Miranda, Harmsen Mirjam, Wollersheim Hub, Grol Richard, Faber Marjan, Sibbald Bonnie. The impact of nonphysician clinicians: do they improve the quality and cost-effectiveness of health care services? Med Care Res Rev. 2009 Dec;66 (6 Suppl):36S–89S. doi: 10.1177/1077558709346277. [DOI] [PubMed] [Google Scholar]
- Laurant M, Harmsen M, Faber M, Wollersheim H, Sibbald B, Grol R. Revision of professional roles and quality improvement: a review of the evidence. London: The Health Foundation. 2010;0:0–0. [Google Scholar]
- Buchan James, Dal Poz Mario R. Skill mix in the health care workforce: reviewing the evidence. Bull. World Health Organ. 2002;80 (7):575–80. [PMC free article] [PubMed] [Google Scholar]
- Laurant M, Reeves D, Hermens R, Braspenning J, Grol R, Sibbald B. Substitution of doctors by nurses in primary care. Cochrane Database Syst Rev. 2005; (2):CD001271. doi: 10.1002/14651858.CD001271.pub2. [DOI] [PubMed] [Google Scholar]
- Lanuza Dorothy M, Davidson Patricia M, Dunbar Sandra B, Hughes Suzanne, De Geest Sabina. Preparing nurses for leadership roles in cardiovascular disease prevention. Eur J Cardiovasc Nurs. 2011 Jul;10 Suppl 2 ():S51–7. doi: 10.1016/S1474-5151(11)00116-2. [DOI] [PubMed] [Google Scholar]
- Inspectie voor de Gezondheidszorg, Ministerie van Volksgezondheid Welzijn en Sport. Wet op de beroepen in de individuele gezondheidszorg (Wet BIG) Available from: http://www.igz.nl/onderwerpen/handhavingsinstrumenten/wetten/wet_big/ 2012;0:0–0. [Google Scholar]
- Eerste Kamer der Staten Generaal. Wijziging van de Wet op de beroepen in de individuele gezondheidszorg onder andere in verband met de opneming van de mogelijkheid tot taakherschikking. Available from: http://www.eerstekamer.nl/wetsvoorstel/32261_wijziging_van_de_wet_op_de. 2014;0:0–0. [Google Scholar]
- D De Bruijn-Geraets, Y van Eijk-Hustings, B Vrijhoef. Nulmeting Evaluatieonderzoek ARt. 36a Wet BIG met betrekking tot de inzet van de Physician Assistant en de Verpleegkundig Specialist: een samenvatting. Available from: https://www.orde.nl/assets/structured-files/AFB%20%20DOWNL_BEROEPSBELANGEN/DOWNLOADS_BEROEPSBELANGEN/Samenvatting%20Nulmeting%20Evaluatieonderzoek%20Art%2036a%20Wet%20BIG.pdf. 2014;0:0–0. [Google Scholar]
- Dierick-van Daele Angelique T M, Spreeuwenberg Cor, Derckx Emmy W C C, van Leeuwen Yvonne, Toemen Thea, Legius Marja, Janssen Joyce J M, Metsemakers Job F M, Vrijhoef Hubertus J M. The value of nurse practitioners in Dutch general practices. Qual Prim Care. 2010;18 (4):231–41. [PubMed] [Google Scholar]
- VS V&VN, VS en PA Platform. Physician assistants en verpleegkundig specialisten wettelijk op eigen benen. Available from: http://www.platformzorgmasters.nl/cms/wp-content/uploads/2012/06/Physician-assistants-en-verpleegkundig-specialisten-ookwettelijk-op-eigen-benen.pdf. 2014;0:0–0. [Google Scholar]
- Nieuwlaat Robby, Prins Martin H, Le Heuzey Jean-Yves, Vardas Panos E, Aliot Etienne, Santini Massimo, Cobbe Stuart M, Widdershoven Jos W M G, Baur Leo H, Lévy Samuel, Crijns Harry J G M. Prognosis, disease progression, and treatment of atrial fibrillation patients during 1 year: follow-up of the Euro Heart Survey on atrial fibrillation. Eur. Heart J. 2008 May;29 (9):1181–9. doi: 10.1093/eurheartj/ehn139. [DOI] [PubMed] [Google Scholar]
- Kakkar Ajay K, Mueller Iris, Bassand Jean-Pierre, Fitzmaurice David A, Goldhaber Samuel Z, Goto Shinya, Haas Sylvia, Hacke Werner, Lip Gregory Y H, Mantovani Lorenzo G, Turpie Alexander G G, van Eickels Martin, Misselwitz Frank, Rushton-Smith Sophie, Kayani Gloria, Wilkinson Peter, Verheugt Freek W A. Risk profiles and antithrombotic treatment of patients newly diagnosed with atrial fibrillation at risk of stroke: perspectives from the international, observational, prospective GARFIELD registry. PLoS ONE. 2013;8 (5):e63479. doi: 10.1371/journal.pone.0063479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gage B F, Waterman A D, Shannon W, Boechler M, Rich M W, Radford M J. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001 Jun 13;285 (22):2864–70. doi: 10.1001/jama.285.22.2864. [DOI] [PubMed] [Google Scholar]
- Lip Gregory Y H, Nieuwlaat Robby, Pisters Ron, Lane Deirdre A, Crijns Harry J G M. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010 Feb;137 (2):263–72. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- Hendriks Jeroen M L, de Wit Rianne, Crijns Harry J G M, Vrijhoef Hubertus J M, Prins Martin H, Pisters Ron, Pison Laurent A F G, Blaauw Yuri, Tieleman Robert G. Nurse-led care vs. usual care for patients with atrial fibrillation: results of a randomized trial of integrated chronic care vs. routine clinical care in ambulatory patients with atrial fibrillation. Eur. Heart J. 2012 Nov;33 (21):2692–9. doi: 10.1093/eurheartj/ehs071. [DOI] [PubMed] [Google Scholar]
- Lobach D F, Hammond W E. Computerized decision support based on a clinical practice guideline improves compliance with care standards. Am. J. Med. 1997 Jan;102 (1):89–98. doi: 10.1016/s0002-9343(96)00382-8. [DOI] [PubMed] [Google Scholar]
- Persson M, Mjörndal T, Carlberg B, Bohlin J, Lindholm L H. Evaluation of a computer-based decision support system for treatment of hypertension with drugs: retrospective, nonintervention testing of cost and guideline adherence. J. Intern. Med. 2000 Jan;247 (1):87–93. doi: 10.1046/j.1365-2796.2000.00581.x. [DOI] [PubMed] [Google Scholar]
- Milani Richard V, Lavie Carl J, Dornelles Adriana C. The impact of achieving perfect care in acute coronary syndrome: the role of computer assisted decision support. Am. Heart J. 2012 Jul;164 (1):29–34. doi: 10.1016/j.ahj.2012.04.004. [DOI] [PubMed] [Google Scholar]
- Inglis Sally C, Clark Robyn A, McAlister Finlay A, Ball Jocasta, Lewinter Christian, Cullington Damien, Stewart Simon, Cleland John Gf. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev. 2010; (8):CD007228. doi: 10.1002/14651858.CD007228.pub2. [DOI] [PubMed] [Google Scholar]
- Wess Mark L, Schauer Daniel P, Johnston Joseph A, Moomaw Charles J, Brewer David E, Cook E Francis, Eckman Mark H. Application of a decision support tool for anticoagulation in patients with non-valvular atrial fibrillation. J Gen Intern Med. 2008 Apr;23 (4):411–7. doi: 10.1007/s11606-007-0477-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camm A John, Lip Gregory Y H, De Caterina Raffaele, Savelieva Irene, Atar Dan, Hohnloser Stefan H, Hindricks Gerhard, Kirchhof Paulus. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur. Heart J. 2012 Nov;33 (21):2719–47. doi: 10.1093/eurheartj/ehs253. [DOI] [PubMed] [Google Scholar]
- Raad voor de Volksgezondheid en Zorg. Taakherschikking in de gezondheidszorg. Available from: http://rvz.net/publicaties/bekijk/taakherschikking-in-de-gezondheidszorg. 2014;0:0–0. [Google Scholar]
- Buljac-Samardzic Martina, Dekker-van Doorn Connie M, van Wijngaarden Jeroen D H, van Wijk Kees P. Interventions to improve team effectiveness: a systematic review. Health Policy. 2010 Mar;94 (3):183–95. doi: 10.1016/j.healthpol.2009.09.015. [DOI] [PubMed] [Google Scholar]
- Nederlandse Vereniging voor Hart en Vaat Verpleegkundigen, Werkgroep Atriumfibrilleren. Zorgmodel Atriumfibrilleren - Een zorgmodel voor de poliklinische behandeling en begeleiding van patiënten met atriumfibrilleren door de Verpleegkundig Specialist onder supervisie van de Cardioloog. Available from: http://www.nvhvv.nl/userfiles/Zorgmodel_final_2.pdf. 2014;0:0–0. [Google Scholar]
- J Glasby. Hospital discharge: integrating health and social care. Abingdon. Radcliffe Medical Press. 2003;0:0–0. [Google Scholar]
- Riegel Barbara, Jaarsma Tiny, Strömberg Anna. A middle-range theory of self-care of chronic illness. ANS Adv Nurs Sci. 2012 Jun 29;35 (3):194–204. doi: 10.1097/ANS.0b013e318261b1ba. [DOI] [PubMed] [Google Scholar]
- Lee Geraldine A. Always fibrillating: is your patient handling their atrial fibrillation? Eur J Cardiovasc Nurs. 2013 Apr;12 (2):107–8. doi: 10.1177/1474515112468631. [DOI] [PubMed] [Google Scholar]
- Hibbard Judith H, Greene Jessica, Tusler Martin. Improving the outcomes of disease management by tailoring care to the patient's level of activation. Am J Manag Care. 2009 Jun;15 (6):353–60. [PubMed] [Google Scholar]
- Vrijhoef H J, Diederiks J P, Spreeuwenberg C, Wolffenbuttel B H. Substitution model with central role for nurse specialist is justified in the care for stable type 2 diabetic outpatients. J Adv Nurs. 2001 Nov;36 (4):546–55. doi: 10.1046/j.1365-2648.2001.02007.x. [DOI] [PubMed] [Google Scholar]
- Meulepas Marianne A, Jacobs Johanna E, Smeenk Frank W J M, Smeele Ivo, Lucas Annelies E M, Bottema Ben J A M, Grol Richard P T M. Effect of an integrated primary care model on the management of middle-aged and old patients with obstructive lung diseases. Scand J Prim Health Care. 2007 Sep;25 (3):186–92. doi: 10.1080/02813430701573943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houweling S T, Kleefstra N, van Hateren K J J, Kooy A, Groenier K H, Ten Vergert E, Meyboom-de Jong B, Bilo H J G. Diabetes specialist nurse as main care provider for patients with type 2 diabetes. Neth J Med. 2009 Aug 19;67 (7):279–84. [PubMed] [Google Scholar]
- Houweling Sebastiaan T, Kleefstra Nanne, van Hateren Kornelis J J, Groenier Klaas H, Meyboom-de Jong Betty, Bilo Henk J G. Can diabetes management be safely transferred to practice nurses in a primary care setting? A randomised controlled trial. J Clin Nurs. 2011 May;20 (9-10):1264–72. doi: 10.1111/j.1365-2702.2010.03562.x. [DOI] [PubMed] [Google Scholar]
- Shortell S M, Gillies R R, Anderson D A. The new world of managed care: creating organized delivery systems. Health Aff (Millwood) 1994;13 (5):46–64. doi: 10.1377/hlthaff.13.5.46. [DOI] [PubMed] [Google Scholar]
- Hendriks Jeroen M L, Vrijhoef Hubertus J M, Crijns Harry J G M, Brunner-La Rocca Hans Peter. The effect of a nurse-led integrated chronic care approach on quality of life in patients with atrial fibrillation. Europace. 2014 Apr;16 (4):491–9. doi: 10.1093/europace/eut286. [DOI] [PubMed] [Google Scholar]
- Hendriks Jeroen, Tomini Florian, van Asselt Thea, Crijns Harry, Vrijhoef Hubertus. Cost-effectiveness of a specialized atrial fibrillation clinic vs. usual care in patients with atrial fibrillation. Europace. 2013 Aug;15 (8):1128–35. doi: 10.1093/europace/eut055. [DOI] [PubMed] [Google Scholar]
- Clinicaltrials.gov. Available from: http://clinicaltrials.gov/ct2/show/ NCT01740037?term=Crijns&rank=2. 2014;0:0–0. [Google Scholar]
- Nolte E, McKee M. Caring for people with chronic conditions - A health system perspective. Berkshire, England: Open University Press. 2008;0:0–0. [Google Scholar]