Abstract
Radicular cyst (RC) is the most common odontogenic cyst of inflammatory origin affecting the jaws; involves the roots of the carious or traumatic non-vital tooth. Different therapeutic modalities, such as nonsurgical endodontic therapy or surgical enucleation with primary closure, decompression etc., were proposed for the management of such lesions. Presenting a case of a 28-year-old otherwise healthy male patient who reported with pain and swelling with respect to tooth #41, 31. Diagnosis of infected RC at a rare location was established on the basis of clinical, radiographical and fine needle aspiration cytological examination. Looking after the clinical characteristics, origin, extension, size of cystic lesion and patient cooperation; nonsurgical endodontic therapy utilizing Bhasker's hypothesis was opted. One year post-operative result suggested that nonsurgical endodontic therapy along with minimally invasive treatment utilizing Bhasker's hypothesis is an effective tool to transform infected radicular cystic lesion to healthy periapical periodontal tissue.
Keywords: Minimal invasive treatment, nonsurgical endodontic therapy, odontogenic cyst, radicular cyst
Introduction
Radicular cyst (RC) is generally defined as a cyst arising from epithelial residues (cell rests of Malassez) in the periodontal ligament as a consequence of inflammation, usually following the death of dental pulp; most commonly found at the apices of the involved teeth but may also be found on the lateral aspects of the roots in relation to lateral accessory root canals.[1] Their size may regress, remain static or grow and may be found when intraoral periapical (IOPA) radiographs are taken of teeth with nonvital pulp; as round- or pear-shaped unilocular radiolucent lesion.[2] The cyst may displace adjacent teeth or cause mild root resorption. Different treatment modalities available for the management of localized RC. For small lesion, conventional root canal therapy alone is sufficient, but if the lesion is large, endodontic therapy should be associated with surgical intervention such as enucleation or marsupialization or decompression as cited in report of Narula et al.[1] Although the opinion varies among professionals as some opt for conservative endodontic therapy whereas other prefer surgical intervention. However, surgical intervention may have its own drawbacks such as patient apprehension and discomfort, devitalization of adjacent tooth, loss of bony support, or sometimes paresthesia.[3] The aim of the present rare case report is not only to describe the diagnosis but also the successful management of RC through nonsurgical endodontic therapy in collaboration with minimally invasive approach utilizing “Bhasker's Hypothesis.”
Case Report
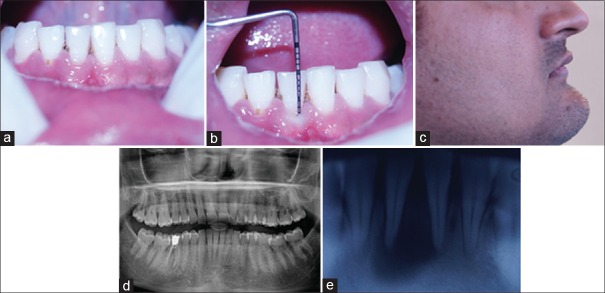
A 28-year-old male patient reported to the outpatient Department of Periodontology with a chief complaint of severe pain on biting from right lower front teeth and presented with a sensation of mild, gradual increase in swelling on the right front aspect of the chin since 10 days. Patient's past history revealed accidental injury of mandibular anterior teeth 2 years back. Intraoral examination showed vertical tenderness on percussion in tooth #41 with raised and fluctuating vestibule up to mucogingival junction of periodontally healthy teeth #31, # 41 [Figure 1a and b] with slight evidence of extra-oral swelling with respect to the mentolabial sulcus region and obliteration of the same [Figure 1c]. Orthopantomogram and IOPA X-ray revealed pear shaped radiolucency (approximately 1.5 cm × 1.5 cm) circumscribing the roots of #41 extending up to #31 with thin radiopaque border [Figure 1d and e]. Tooth #41 reported as nonvital whereas #31 vital after vitality testing. On the basis of clinical and radiographical findings, provisional diagnosis of infected radicular cyst with respect to #41 was established and was further confirmed by fine needle aspiration cytological examination at ×10, ×40 showed numerous chronic inflammatory cells chiefly consisting of lymphocytes in a dirty background and few small and medium size cholesterol crystals of variable shapes [Figure 2a and b].
Figure 1.
(a) Raised and fluctuating vestibule up to mucogingival junction of tooth #31, #41; (b) normal gingival sulcus depth of 3 mm; (c) extraoral swelling on mental region of chin; and (d and e) orthopantomogram and intraoral periapical showing radiolucency with respect to tooth #41 extending up to mesial aspect of #31
Figure 2.
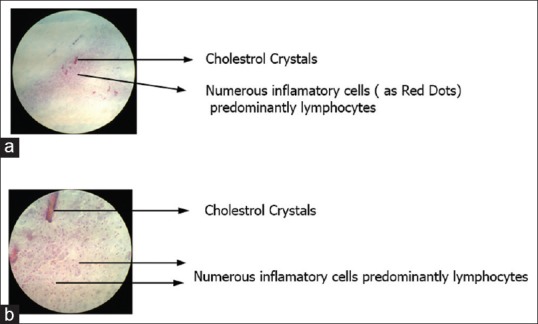
(a and b) Inflammatory cells predominately lymphocytes with cholesterol crystals in dirty background at ×10 and ×40, respectively
Under local anesthesia, emergency access opening was made in #41 and necrotic pulp was extirpated followed by copious irrigation with sodium hypochlorite, hydrogen peroxide and normal saline and filled with calcium hydroxide mixed in 2% chlorhexidine followed by closed dressing utilizing cavit (3M) an intermediate restorative material (IRM). After listening to clinician's advice carefully; patient submitted signed written consent in favor of endodontic therapy utilizing Bhasker's hypothesis. Utilizing step back technique, biomechanical preparation (BMP) was done followed by minimal over instrumentation beyond apical foramen as recommended by Bhasker's hypothesis, after 7 days of working length determination following the access opening [Figure 3a], followed by thorough irrigation with sodium hypochlorite, hydrogen peroxide and normal saline. Root canal was replenished with a mixture of calcium hydroxide and chlorhexidine followed by closed dressing of IRM. The intracanal irrigation and medicament repeated 4 times, at 5 days intervals each. Complete regression of swelling on the lateral aspect of the chin was reported by the patient just 10 days after BMP and clinically mentolabial fold could be appreciated too [Figure 3b] whereas root canal was sterilized by the end of 3 weeks post-BMP. Three-dimensional root canal obturation was carried out utilizing simple lateral condensation technique. The patient was reevaluated at 3, 6, 9 and 12 months postoperatively. The radiographs depicted continuous regression in cystic lesion from 3 months onwards which was almost completely resolved at 1year post-operatively [Figure 3c–f] without any clinical signs or symptoms of recurrence with healthy soft tissue.
Figure 3.
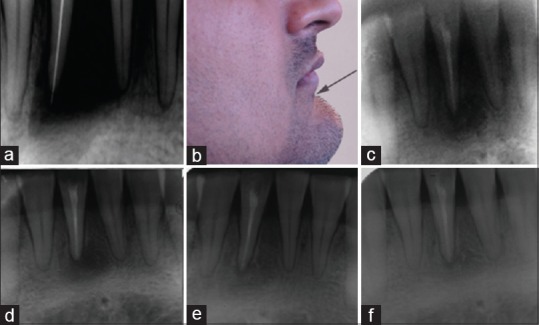
Intraoral periapical X-rays, (a) over instrumentation of 1–2 mm, (b) reduction in swelling on mental region of chin whereas (c-f) regression/resolution of lesion at 3, 6, 9, and 12 months postoperatively
Discussion
RC is the most common cystic lesion comprising about 52%–68% of all the cysts affecting human jaw;[4] anatomically, the periapical cysts occur in all tooth-bearing sites of the jaw but incidence is more frequent in the maxilla[4,5] and least (8.5%) in mandibular anterior region.[6] Etiology being infection in the periradicular space either because of trauma or caries etc., usually sterile unless it is secondarily infected.[1] The most frequent clinical manifestation was swelling, followed by a combination of pain and swelling;[6] similar findings were observed, but lesion observed at rare location of mandibular anterior region which made this case a rare entity.
RC represents chronic inflammatory process and develops only over a prolong period. However, few cases of RC may undergo an acute exacerbation of the inflammatory process and rapidly develop into abscess which may lead to cellulitis or form a draining fistula;[7] reason for sudden flare up is not known till date, but it may be the result of loss of local or general tissue resistance that may be the reason for early sign of sensation and recognition of swelling on chin in the present case.
The choice of treatment depends on the size, location of lesion, bony integrity of the cystic wall, its proximity to vital structures.[1] Endodontic therapy alone is not efficient for the management of large lesion and it should be accompanied by enucleation or marsupialization or decompression as cited in the report of Narula et al.[1] However, in the present case, the lesion was large (≥1.5 cm) and in direct communication with root canal system in spite of surgical requirement, nonsurgical endodontic treatment along with minimally invasive treatment modality utilizing Bhasker's hypothesis was opted because tooth #31 was vital as surgical intervention may lead to devitalization[3] of same and secondly patient was interested in nonsurgical management.
Sodium hypochlorite is the most frequently recommended endodontic irrigants because of two-fold advantages; pulp tissue dissolution and antimicrobial effect whereas hydrogen peroxide has shown to be active against viruses, bacteria, bacterial spores and yeasts through the production of hydroxyl free radicals which attack their proteins and DNA as cited in the report of Iqbal.[8] Calcium hydroxide's anti microbial action is influenced by the speed of its dissociation into calcium ions and hydroxyl ions and by inactivating enzymes of the cytoplasmic membrane of microorganisms, thus causing toxic effects on the bacterial cells; another mechanism of action of this medication is its ability to absorb carbon dioxide, thus leading to the death of CO2- dependent bacteria. Chlorhexine may also present residual antimicrobial activity on the dentine surface after prolonged contact within root canal and also improve antimicrobial efficacy against calcium hydroxide resistant microorganisms.[9] Therefore, used as root canal irrigants and as an intracanal dressing for asepsis of root canal in the present case.
During the treatment, minimal over instrumentation was carried out as proposed by Bhaskar who suggested that 1 mm over instrumentation beyond the apical foramen, elicit an inflammatory reaction that destroys the cyst lining and converting the lesion into a granuloma,[10] or it could also facilitate cystic resolution by relieving the intra cystic pressure[11] which will heal on its own spontaneously once etiology is eliminated; that may be the reason for regression of the large cystic lesion after successful endodontic therapy in the present case report. Although the reasons proposed by these techniques might work only theoretically but clinical success was claimed.[12]
The results of present case report showed continuous regression in cystic lesion from 3 to 12 months post-operatively, but cystic lesion healed almost completely (transformed into healthy periapical periodontal tissue) at 1 year post-operatively with evident radiographic signs of progressive change in bone density within the lesion, trabecular reformation, lamina dura formation confirmed healing associated without clinical sign and symptoms of recurrence with healthy soft tissue.[13] The results of the present report is in accordance with the report of Marina Fernandes and De Ataide[14] and Murphy et al.[15] but due to ethical concerns re-entry was not performed.
Conclusion
Nonsurgical endodontic therapy with an emphasis on thorough debridement, degenerate the cystic lining utilizing Bhasker's hypothesis, disinfection, and obturation of root canal system is a simple and effective tool to transform the infected periapical RC to healthy periapical periodontal tissue.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Narula H, Ahuja B, Yeluri R, Baliga S, Munshi AK. Conservative non-surgical management of an infected radicular cyst. Contemp Clin Dent. 2011;2:368–71. doi: 10.4103/0976-237X.91806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bodner L. Cystic lesions of the jaws in children. Int J Pediatr Otorhinolaryngol. 2002;62:25–9. doi: 10.1016/s0165-5876(01)00583-3. [DOI] [PubMed] [Google Scholar]
- 3.Neaverth EJ, Burg HA. Decompression of large periapical cystic lesions. J Endod. 1982;8:175–82. doi: 10.1016/S0099-2399(82)80214-8. [DOI] [PubMed] [Google Scholar]
- 4.Nair PN. New perspectives on radicular cysts: Do they heal? Int Endod J. 1998;31:155–60. doi: 10.1046/j.1365-2591.1998.00146.x. [DOI] [PubMed] [Google Scholar]
- 5.Rees JS. Conservative management of a large maxillary cyst. Int Endod J. 1997;30:64–7. doi: 10.1111/j.1365-2591.1997.tb01100.x. [DOI] [PubMed] [Google Scholar]
- 6.Selvamani M, Donoghue M, Basandi PS. Analysis of 153 cases of odontogenic cysts in a South Indian sample population: A retrospective study over a decade. Braz Oral Res. 2012;26:330–4. doi: 10.1590/s1806-83242012005000007. [DOI] [PubMed] [Google Scholar]
- 7.Gupta A, Adwani DG, Naphade MV, Adwani N. Surgical enucleation of an infected maxillary radicular cyst with associated infraorbital space infection: A case report. Int J Sci Med Dent Res. 2014;1(1):10–13. Available from: http: // www.ijsmdr.org . (C) International Journal of science for medical and dental research [10-13] [Google Scholar]
- 8.Iqbal A. Antimicrobial irrigants in endodontic therapy. Int J Health Sci (Qassim) 2012;6:153–8. [PMC free article] [PubMed] [Google Scholar]
- 9.Silveira CF, Cunha RS, Fontana CE, de Martin AS, Gomes BP, Motta RH, et al. Assessment of the antibacterial activity of calcium hydroxide combined with chlorhexidine paste and other intracanal medications against bacterial pathogens. Eur J Dent. 2011;5:1–7. [PMC free article] [PubMed] [Google Scholar]
- 10.Bhaskar SN. Nonsurgical resolution of radicular cysts. Oral Surg Oral Med Oral Pathol. 1972;34:458–68. doi: 10.1016/0030-4220(72)90325-8. [DOI] [PubMed] [Google Scholar]
- 11.Shear M. Cysts of the oral and maxillofacial region. 3th ed. Sã Paulo: Editora Santos; 1999. [Google Scholar]
- 12.Esposito JV. Apical violation in periapical area cases. Blasphemy or therapy? Dent Clin North Am. 1990;34:171–8. [PubMed] [Google Scholar]
- 13.Ismail H, Monira P, Tasnim W, Farid U. Non-surgical management of non-vital teeth with periapical pathosis by conventional root canal treatment: A clinical and radiological evaluation. Int J Dent Med. 2015;1:13–6. [Google Scholar]
- 14.Fernandes M, De Ataide I. Non-surgical management of a large periapical lesion using a simple aspiration technique: A case report. Int Endod J. 2010;43:536–42. doi: 10.1111/j.1365-2591.2010.01719.x. [DOI] [PubMed] [Google Scholar]
- 15.Murphy WK, Kaugars GE, Collett WK, Dodds RN. Healing of periapical radiolucencies after nonsurgical endodontic therapy. Oral Surg Oral Med Oral Pathol. 1991;71:620–4. doi: 10.1016/0030-4220(91)90374-l. [DOI] [PubMed] [Google Scholar]