Abstract
Pacific Islanders experience high rates of cervical cancer incidence and mortality. This cross-sectional study examined the extent to which Samoan, Chamorro, and Tongan women’s perceived receipt of social support from their husbands or male partners was associated with rates of routine cancer screening- specifically Pap testing. A total of 585 Pacific Islander women who live in the United States completed a self-report survey. Women who reported having a Pap test within the past 3 years had significantly higher scores on support from their husbands/ male partners. Furthermore, the relationship of emotional support and informational support with increased Pap testing was significantly stronger for Tongan women. The findings suggest that men play an important role in promoting women’s cancer prevention behaviors in Pacific Islander and potentially other collectivistic populations. Incorporating social support messages into interventions may be a simple yet effective strategy to increase women’s Pap testing.
Keywords: Chamorro, Pap test, Samoan, Tongan, cervical cancer, social support
Introduction
Pacific Islanders (PIs) experience high cervical cancer health disparities in the United States. Age-adjusted incidence rates among Native Hawaiians (12.3 per 100 000) and Samoans (15.1 per 100 000) are significantly higher than for non-Hispanic whites (NHWs) (8.1 per 100 000).1 Stage of diagnosis is also later for PIs than NHWs: only approximately 40% of NHW cervical cancers are found at the regional or distant stage, compared with nearly 60% among Native Hawaiian and Samoan women.2 Pap tests remain an important cervical cancer prevention and detection method for U.S. women.3 The Pap test is severely underutilized among Asian Americans and Pacific Islanders (AAPIs), with only 71% of AAPI women age 25+ years having received a Pap test within the past 3 years (US average = 82%).4 Healthy People 2020 aims to achieve a cervical cancer screening rate of 93% among all women by 2020.2 In a review of the literature of health care systems in the Asia-Pacific region, cervical cancer screening and preliminary treatment in one visit is feasible, with high patient satisfaction.5
The perceived receipt of social support is believed to be a motivator for multiethnic women to get routine cancer screenings. Studies of African American and others have found positive associations between subjective perceptions of support for breast and cervical cancer screening (eg, having friends or family who encouraged screening) and actual cancer screening behaviors. Conversely those who receive social support may not necessarily perceive the support as helpful, and could even lead to negative health-related consequences such as psychological stress.6
According to the US Census Bureau (2010), California alone had 286 145 PIs, the second largest US population of PIs outside of Hawaii. Southern California is an ideal geographic area to examine Pap testing among PI women, as there are close to 110 000 PIs living in the Los Angeles area, growing 22% from 2000 to 2010. This region has the largest number of Chamorro Americans and Samoans Americans in the continental United States, and the third largest population of Tongan Americans in the United States.7 Educational attainment, health insurance coverage, and per capita income are lower for PIs compared with most other racial/ethnic groups.8 Social support is particularly relevant in PI communities.
The Tongan and Samoan cultures have been described by their elders as collectivist, in which the supportive social environment that their large networks provide positively affects the health of all who belong to the network. Social support is one essential function that social networks, including marital relationships provide,9 and can be categorized into 4 broad types of supportive behaviors or acts: emotional, instrumental, informational, and appraisal.6,10 Such social support underscores the importance of relational culture, or “… the processes of interdependence and interconnectedness among individuals and groups, and the prioritization of these connections above virtually all else,”11 which is exemplified in Samoans saying tausi le mafutaga (taking care of relationships), Chamorros saying inafa’maolek (the interdependence of family), and Tongans saying tauhi ‘e vaa (taking care of relationships).
The way in which social support is provided, as well as its effects on cancer-related outcomes, varies across cultures such as PI subgroups.12 For example, a support group intervention found that Samoan breast cancer survivors were generally reluctant, at the beginning, to share their feelings and emotions (as it is perceived as a sign of weakness, of complaining, and of being a burden to the family). However, over time, they were able to share their feelings and emotions freely and ask for much-needed support from friends and family.13 Similar outcomes have been reported from supportive lay health activities in the Chamorro community.14 For AAPIs, the importance of friends and family support are also related to their rates of cancer screening. The Wai‘anae Cancer Research Project tested the impact of social support from other women, belonging to kokua groups, on Native Hawaiian women’s Pap testing and found an 8% increase in Pap compliance over a 3-year period.15 In the Life is Precious Hmong Breast Health Study, women who received a social support intervention specifically from their husbands were significantly more likely to have performed breast self-examinations, received a clinical breast exam, and mammogram at one year follow-up compared with controls.16
The Present Study
No study to date has examined the impact of husband’s support on PI women’s Pap testing. Building on the work of both Wai‘anae and Life is Precious, the purpose of this study was to examine whether PI women’s perceived receipt of social support from her husband or long-term partner was related to her likelihood of receiving a Pap test within the past 3 years. We predicted that such an association would exist. This article is part of a larger intervention study that tests the impacts of a culturally tailored intervention on increasing women’s Pap testing rates in 3 PI communities of Southern California. Although Chamorro, Samoan, and Tongan communities are known to have collectivistic values,12-14 they may vary in the extent to which social support influences women’s health screening behaviors. Therefore, we also examined whether relationships between social support and receipt of a Pap test within the past 3 years varied among Chamorro, Samoan, and Tongan women (who have the lowest educational attainment and income compared to the other PI groups).
The findings of this study may be especially relevant to women who are native to and live in the Pacific Islands, as it has been noted that smaller Pacific Islands face challenges to effectively deliver public health services due to a paucity of health workers in less densely populated areas. Hence, interventions that draw on women’s family connections may be more sustainable when the presence of health workers is limited.17
Methods
Study Design
The data used for these analyses were derived from baseline self-report responses from a 5-year longitudinal study that used community-based participatory research (CBPR) strategies to develop and test the efficacy of a social support intervention targeting Chamorro, Samoan, and Tongan women aged 21 to 65 years, and their male partners, to increase women’s Pap testing behaviors. The CBPR partnership involved staff from 3 community-based organizations and 1 university, along with a Community Advisory Board composed of Chamorro, Samoan, and Tongan community leaders and cancer survivors. Information on the CBPR approaches and outcomes have been previously described.18 A cross-sectional design was chosen for this study to test the theoretical premise that men’s social support is related to women’s receipt of a Pap test. Furthermore, using baseline data only maximized the sample size available for the analyses. Intervention findings, which will include the impact of changes in social support on Pap testing, will be presented in a subsequent article.
Participants
We recruited Samoan and Tongan faith-based organizations and Chamorro family clans into the study. Next, pairs of eligible women and their spouses/significant others from their respective organizations were identified and invited to participate in the study. Eligibility criteria for women included (a) Samoan, Tongan, and/or Chamorro woman who is a member in at least one of the organizations or clans recruited into this study, (b) between the ages of 21 and 65 years, and (c) married or in a long-term relationship with a man of any ethnicity for at least 5 years. For this study, only women’s data were analyzed. A total of 585 women met the inclusion criteria and completed the baseline survey.
Procedures
Recruitment
We used an organizational sampling approach to recruit Samoan and Tongan churches and Chamorro clans. Lists of these southern Californian clans and churches were compiled based on the authors’ previous community health partnerships and programs with the PI community. An official letter with contact information of the university and community partners, and $200 or food as compensation was offered to each church and clan that agreed to host a study session at their site. The project health educators spearheaded the recruitment process, which often involved multiple follow-up calls, in-person meetings, and attendance at social events such as family parties and church activities. Once the leader(s) of a given church or clan agreed to have the organization participate in the study, the leader(s) recruited eligible organizational members to participate in the study. Subsequently, the study health educator scheduled a meeting at the organization’s site to administer the baseline survey and implement the 1-hour intervention or control education session.
Survey Administration
The health educators administered the self-report surveys, with all female participants in one room. The surveys were provided in both English and in participants’ native language. Participants were instructed to complete one page at a time, and stop until everyone had completed that page. Therefore if any questions came up, the health educator was able to address the questions with the entire group. After the survey and education, all participants received a small thank you gift (a woven box with toiletries) and a $10 gift card. All procedures described here were approved by the university’s institutional review board.
Measures, Translation, and Pilot Testing
Pap Test Compliance
For this study, Pap test compliance was based on the following question that was included in the female participants’ baseline survey: “When did you have your most recent Pap test?” The American Cancer Society recommends that all women 21 years and older receive Pap tests at least once every 3 years.2 Hence, we categorized women who answered “within the past 3 years” as compliant (with American Cancer Society guidelines), and all other women as noncompliant.
Women’s Perceived Receipt of Social Support From Their Male Partners
For this study, we adopted the Emotional/Informational Support, Tangible Support, and Affectionate Support subscales of the MOS Social Support Survey.19 This scale assesses general social support, not support specifically related to cancer screening. We used 4 subscales:
Instrumental support (4 items, Cronbach’s α = .89, eg, “My husband/partner could take me to the doctor if needed.”)
Emotional support (3 items, Cronbach’s α = .93, eg, “My husband/partner showed me love and affection.”)
Informational support (4 items, Cronbach’s α = .83, eg, “My husband/partner gave me good advice about a crisis.”)
Appraisal support (3 items, Cronbach’s α = .84, eg, “I could count on my husband/partner to listen to me when I needed to talk.”)
The answers to all questions in the original version of the survey were on a 5-point Likert-type scale, ranging from “strongly disagree” to “strongly agree.” Scores on the 4 subscales were added to create a total score for women’s perceived receipt of social support. In this study, male partners (the female participants’ significant others) completed a 7-item scale that assessed their perceived provision of social support (adopted from the Berlin Social Support Scale20; Cronbach’s α = .88). Women’s perceived receipt of social support was significantly correlated with their male partners’ perceived provision of social support (R2 = .085, P = .000). Hence, women’s perceptions of social support corresponded, to some degree, with their male partners’ perceptions.
Demographic Variables
Some of the demographic variables assessed in this study included female participants’ age, PI ethnicity, health insurance coverage, preferred language to speak at home, and years in her current marriage/relationship. Participants also completed a short version of the Marlow-Crowne Social Desirability Scale,21 which consisted of 10 true/false items such as, “I never like to gossip.” Cronbach’s α was .67. Participants also completed 11 true/false items, which assessed participants’ knowledge about cervical cancer risk factors, including sexual history, human papilloma virus infection, smoking, diet, oral contraceptives, and family history. Questions came from existing surveys of PI cancer control, as well as questions from the National Health Interview Survey, Cancer Control Supplement.22,23 Last participants completed 5 true/false items regarding fatalistic attitudes toward cervical cancer screening, including benefits of early cancer detection, willingness to undergo treatment, whether they would want to know about their cancer status, and potential fears that cervical cancer may affect their relationships with husbands or other loved ones.23
Survey Translation
Survey translation from English into the native PI language was completed by a bilingual and bicultural translator, and then independently reviewed by a second translator for reading, clarity, simplicity, minimal use of jargon, utilization of conceptual equivalents of words and phrases rather than literal translation, and use of appropriate words with consideration to the audience. Any discrepancies between 2 translators were discussed, with resolutions shared with the Community Advisory Board members for final approval on specific wording or phrasing.
Pilot Testing
Surveys were pilot tested by 18 community members who met all eligibility requirements of the study but did not participate in the study. These community members consisted of 3 women from each of the 3 ethnic groups in the study. Pilot testing helped the study team determine the length of survey duration, quality of translation, comprehension of survey items, and clarity of answer categories. For instance, after pilot testing we found that respondents did not see a difference between some Likert categories, and thus answer categories were modified for the social support items from a 5-point to a 4-point scale, ranging from “none of the time” to “all of the time.” A previous study suggests that Asian Americans tend to avoid selecting extreme responses to multiple choice survey questions (for our study, responses such as “none of the time” and “all of the time”).24 To determine whether this aversion of extreme responses pertained to our sample of PI women, we examined frequency distributions for each of the 14 social support items. These results indicated that participants did not avoid extreme responses, as the most often selected answer for all of the social support items was “all of the time.” Participants selecting the “all of the time” answer ranged from as low as 27.8% (for the item “Take me to the doctor if needed”) to as high as 54.0% (for the item, “Provided me information to help me understand a situation”). Since participants in our study tended to choose the highest-scoring answer, there was less concern that the elimination of 1 point from the 5-point scale substantially reduced variation in responses to the social support items.
Statistical Analyses
Descriptive statistics were calculated for demographic variables and the social support subscales, stratified by Pap test status (had or not had a Pap test in the past 3 years). Then we ran unadjusted and adjusted logistic regression models—one for each subscale of women’s perceived receipt of social support and one for the entire social support scale, to determine its relation to Pap test status. All regression models included the social support subscale or total scale, Tongan ethnicity, the social support × Tongan ethnicity interaction term, and demographic covariates that were significantly associated with Pap test status. Tongan ethnicity and its interaction with social support were included in these models to determine whether the relationship between social support and Pap testing varied among the 3 communities. We specifically compared Tongans with Samoans and Chamorros in these analyses because Tongans had much lower rates of Pap testing compared with the other 2 communities. Figures were plotted and inspected to decipher the direction of the findings for the significant interaction terms.
Results
Descriptive Statistics by Pap Status
Table 1 presents descriptive statistics by Pap test within the past 3 years. Samoan and Chamorro women (61.3%), and women who had health insurance (60.,4%) had higher rates of Pap testing compared with Tongan women (31.4%) and women with no health insurance (26.6%). Furthermore, women who had a Pap test within 3 years answered more knowledge items correctly (M = 4.72 ± 3.00), had fewer fatalistic attitudes (M = 0.90 ± 1.06), and had higher scores on social desirability (M = 6.89 ± 2.15) compared with women who had not had a Pap test within the past 3 years (M = 1.52 ± 1.32, M = 6.46 ± 2.18, and M = 6.46 ± 2.18, respectively). Women who had received a Pap test within 3 years had higher scores on all 4 social support subscales (M = 14.51 ± 2.49 for instrumental support, M = 11.09 ± 1.76 for emotional support, M = 13.12 ± 2.77 for informational support, and M = 10.48 ± 2.14 for appraisal support), and the sum of these 4 subscales (M = 52.66 ± 8.46), compared with women who had not had a Pap test within the past 3 years (M = 13.68 ± 3.03 for instrumental support, M = 10.55 ± 2.21 for emotional support, M = 12.44 ± 2.98 for informational support, M = 9.89 ± 2.25 for appraisal support, and M = 49.94 ± 9.67 for the total social support scale). Rates of Pap testing did not vary by age, preferred language spoken at home, and number of years in their current marriage or relationship.
Table 1.
Descriptive Statistics of the Female Participants (n = 585).
| Pap Test Within 3 Years (n = 311) |
No Pap test Within 3 Years (n = 274) |
|||||
|---|---|---|---|---|---|---|
| f | % | f | % | χ 2 | P | |
| Demographic characteristics | ||||||
| Age <40 years | 131 | 54.4 | 110 | 45.6 | 0.25 | .970 |
| Age 40+ years | 179 | 52.6 | 161 | 47.4 | ||
| Tongans | 50 | 31.4 | 109 | 68.6 | 41.35 | .000 |
| Samoans and Chamorros | 261 | 61.3 | 165 | 38.7 | ||
| Have health insurance | 275 | 60.4 | 180 | 39.6 | 44.78 | .000 |
| No insurance | 33 | 26.6 | 91 | 73.4 | ||
| Other language preferred | 35 | 42.2 | 48 | 57.8 | 8.56 | .073 |
| English or other language | 128 | 52.0 | 118 | 48.0 | ||
| English language preferred | 144 | 57.1 | 108 | 42.9 | ||
|
| ||||||
| M | SD | M | SD | F | P | |
|
| ||||||
| Number of years in marriage/ relationship |
16.81 | 11.72 | 17.42 | 12.50 | 0.549 | .359 |
| Cervical cancer knowledge (out of 11) |
4.72 | 3.00 | 5.62 | 2.66 | 13.82 | .000 |
| Fatalism (out of 5) | 0.90 | 1.06 | 1.52 | 1.32 | 35.46 | .000 |
| Social desirability score (0-10) | 6.89 | 2.15 | 6.46 | 2.18 | 5.66 | .018 |
|
Women’s total perceived receipt of social support (α = .94) |
52.66 | 8.46 | 49.94 | 9.67 | 12.73 | .000 |
| Instrumental (α = .89) | 14.51 | 2.49 | 13.68 | 3.03 | 13.20 | .000 |
| Emotional (α = .93) | 11.09 | 1.76 | 10.55 | 2.21 | 10.44 | .001 |
| Informational (α = .83) | 13.12 | 2.77 | 12.44 | 2.98 | 7.93 | .005 |
| Appraisal (α = .84) | 10.48 | 2.14 | 9.89 | 2.25 | 11.55 | .001 |
Logistic Regression of Pap Test Status
Table 2 presents logistic regression of Pap test status; a separate model was run for each individual social support scale as a predictor, since including all scales as predictor variables in one model predicting Pap testing resulted in nonsignificant results due to high correlations among the scales. Each model also included a social support scale × Tongan ethnicity interaction term, to determine whether the relationship between social support and Pap testing varied between Tongans versus Samoans and Chamorros. This particular interaction term was chosen since Tongans had considerably lower rates of Pap testing compared to Samoans and Tongans. These models also adjusted for Tongan ethnicity, health insurance, fatalism, and social desirability, as these variables were both associated with Pap testing in the previous analyses.
Table 2.
Logistic Regression of Women’s Receipt of Pap Test Within the Past 3 Years.
| OR | 95% CI | P | AORa | 95% CI | P | |
|---|---|---|---|---|---|---|
| Instrumental support | 1.12 | 1.05-1.19 | .000 | 1.05 | 0.97-1.14 | .236 |
| Tongan ethnicity | 0.29 | 0.20-0.43 | .000 | 0.07 | 0.005-0.863 | .038 |
| Instrumental × Tongan | 1.14 | 0.98-1.33 | .099 | 1.13 | 0.95-1.35 | .164 |
| Emotional support | 1.15 | 1.05-1.25 | .002 | 1.04 | 0.93-1.16 | .530 |
| Tongan ethnicity | 0.29 | 0.20-0.43 | .000 | 0.02 | 0.001-0.36 | .009 |
| Emotional × Tongan | 1.23 | 0.98-1.56 | .074 | 1.34 | 1.01-1.77 | .040 |
| Informational support | 1.09 | 1.03-1.15 | .005 | 1.02 | 0.94-1.10 | .633 |
| Tongan ethnicity | 0.29 | 0.20-0.43 | .000 | 0.04 | 0.004-0.37 | .005 |
| Informational × Tongan | 1.16 | 0.996-1.35 | .056 | 1.20 | 1.01-1.42 | .039 |
| Appraisal support | 1.14 | 1.06-1.24 | .001 | 1.06 | 0.96-1.18 | .248 |
| Tongan ethnicity | 0.29 | 0.20-0.43 | .000 | 0.13 | 0.01-1.22 | .074 |
| Appraisal × Tongan | 1.13 | 0.92-1.38 | .245 | 1.11 | 0.90-1.38 | .325 |
| Total social support | 1.04 | 1.02-1.06 | .000 | 1.01 | 0,99-1.04 | .299 |
| Tongan ethnicity | 0.29 | 0.20-0.43 | .000 | 0.26 | 0.001-0.47 | .014 |
| Total × Tongan | 1.05 | 0.998-1.10 | .061 | 1.05 | 0.998-1.11 | .061 |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio.
Adjusted odds ratios were adjusted for health insurance, fatalism, and social desirability.
The unadjusted odds ratios presented in Table 2 indicate that all social support scales were positively related to Pap testing, with all odds ratios significantly greater than 1, and that Tongan ethnicity was related to lower rates of Pap testing, with an odds ratio significantly less than one. However in the adjusted models, none of the social support scales remained statistically significant. With the exception of the model that included appraisal support, Tongan ethnicity was significantly related to lower rates of Pap testing. Adjusted odds ratios (AORs) for Tongan ethnicity ranged from 0.02 for the model that included emotional support as a predictor variable, to 0.026 for the model that included the total social support scale. The interaction of Tongan ethnicity with social support was significantly related to Pap testing, specifically for emotional support (AOR = 1.34, P = .040) and for informational support (AOR = 1.20, P = .039). The interaction of Tongan ethnicity with the total social support scale was nearly significant (AOR = 1.05, P = .061).
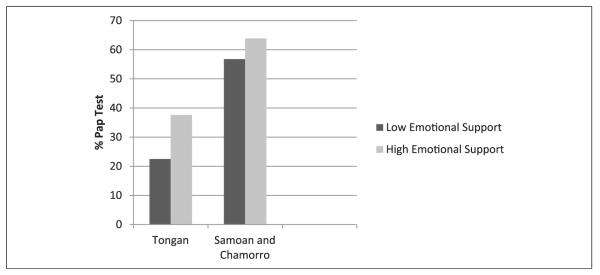
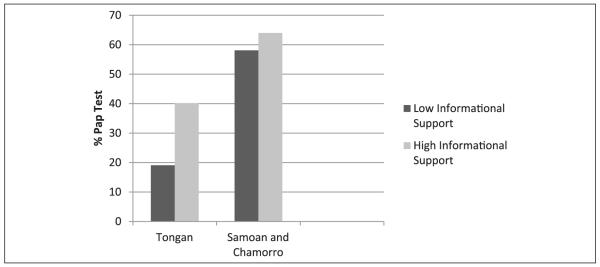
Figures 1 and 2 further illustrate the nature of the significant interaction terms found in Table 2. Specifically, we examined Pap testing rates among 4 categories of women, for emotional support and for informational support separately: (a) Tongans, low social support; (b) Tongans, high social support; (c) Samoans and Chamorros, low social support; and (d) Samoans and Chamorros, high social support. The dichotomous classification of social support (low level of support versus high level of support) was based on the median split, with scores equal to or above the median being classified as “high,” and scores less than the median being classified as “low.”
Figure 1.
Percentage of women who had a Pap test within the past 3 years, by ethnicity and level of emotional support. Emotional support was classified as “low” if scores were below the median of 12, while scores of 12 or higher were classified as “high.”
Figure 2.
Percentage of women who had a Pap test within the past 3 years, by ethnicity and level of informational support. Informational support was classified as “low” if scores were below the median of 13, while scores of 13 or higher were classified as “high.”
The general pattern seen in Figures 1 and 2 is that Tongan women have much lower rates of Pap testing compared with Samoan and Chamorro women. However, high levels of emotional support and informational support appear to more strongly increase Pap testing rates among Tongan women compared with Samoan and Chamorro women. For Tongan women, the difference in Pap testing rates between those with low levels of emotional support and those with high levels of emotional support was 15.1% (22.5% for low vs 37.6% for high). For Samoan and Chamorro women, there was only a 7.1% difference in Pap testing rates between the low emotional support group and the high emotional support group (56.8% vs 63.9%).
The effect of informational support on Pap testing appeared to be much greater for Tongans compared to Samoans and Chamorros. For Tongan women, the difference in Pap testing rates between the low informational support group and the high informational support group was 21.1% (19.1% for low vs 40.2% for high). For Samoan and Chamorro women, there was only a 5.9% difference in Pap testing rates between the low informational support group and the high informational support group (58.1% vs 64.0%).
Discussion
Our unadjusted findings of a relationship between PI women’s perceived social support and Pap testing behaviors are consistent with our prediction and the suggestion that enhancing the quality of women’s social networks, specifically their relationship with their husband/male partner, may facilitate cancer screening efforts above and beyond the impact of traditional cancer prevention strategies (eg, increasing knowledge of cancer risk factors).25 The relationship between social support and Pap testing may be especially relevant to Samoan, Tongan, and Chamorro populations, since their respective cultures place a greater importance on the well-being of others within their social network compared with themselves.13
A finer-grained analysis revealed the finding that Tongan women were especially likely to have received a Pap test within the past 3 years, compared with Samoan and Chamorro women, if they reported relatively high scores for the emotional support and informational support items. This finding is particularly encouraging, given that in our sample, Tongan women had the lowest rates of Pap testing and therefore may be most responsive to a men’s social support intervention to increase women’s Pap testing rates. It is important to note that the Tongan ethnicity by social support interaction effect was significant after statistically adjusting for the effects of health insurance coverage, which is typically a strong indicator of socioeconomic status. For this reason, we suggest that future research is needed to further understand why husbands’/male partners’ provision of social support in the Tongan culture may have a stronger influence on women’s health screenings relative to other PI cultures.
Limitations
There are a few limitations to this study that should be noted. First, the analytic sample was limited to primarily church-going or clan-involved PIs and thus may not generalizable to other populations. Second, the cross-sectional design of our analyses did not allow for the exploration of temporal relationships between the receipt of social support and Pap testing. Third, there is some possibility that changing the 5-point Likert-type scale to a 4-point Likert-type scale for the social support items may have slightly reduced the variation in scores, and therefore may have, to some extent, weakened the relationship between social support and Pap testing. Even with these study limitations, however, our findings add support to the growing area of research on social influences and cervical cancer screening. Past studies have shown that support by significant others (eg, friends, spouses, doctors) is significantly associated with increased Pap and other cancer screening.25-27
Conclusion
In summary, Pap testing remains one of the most important ways to prevent cervical cancer, and Healthy People 2020 recommends increasing to 93% the proportion of US women who receive screening.27 Among current best practices targeting women (including physician reminders, oneon-one and group education, and social marketing), interventions may have greater success if they include messages aimed at increasing family members’ support.27,28 In addition, interventions that aim to improve men’s cancer screening (such as colorectal and prostate) should consider incorporating women’s health reminders. It is also important to note that such social support interventions may be more effective among some ethnic populations relative to others, and further exploration is needed to better understand what communities might benefit the most from such collectivistic interventions. In future articles, we will share the outcomes of the culturally tailored intervention to increase husband’s social support and women’s Pap testing behaviors.
Acknowledgments
We would like to recognize the following individuals for their contributions to the project: Mohammed Aftab, Angela Lin, Alisa Chavarria, Laura Dandridge, Rine Fe’a, Mary Anne Foo, Ualani Ho’opai, Brian Hui, Jason Lacsamana, Darlene March, Vanessa Tui’one May, Noelle Moananu, Ciara Paige, Alisi Tulua, Lourdes Tuliau, and Jennifer Xiong, Additionally, we would like to recognize the churches, clans, and Community Advisory Board members who participated in this study. We dedicate this paper to the memory of Caroline Fe’a Pele, who we lost to cancer on July 4, 2015.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was funded by the National Cancer Institute’s Center to Reduce Cancer Health Disparities (grant number 5R01CA149324).
Footnotes
Authors’ Note
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute’s Center to Reduce Cancer Health Disparities.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Miller BA, Chu KC, Hankey BF, Ries LA. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes Control. 2008;19:227–256. doi: 10.1007/s10552-007-9088-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Cancer Society . Cancer Facts & Figures 2012. American Cancer Society; Atlanta, GA: [Accessed August 25, 2015]. 2012. http://www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2012/ [Google Scholar]
- 3.Castle PE, Fetterman B, Poitras N, Lorey T, Shaber R, Kinney W. Five-year experience of human papillomavirus DNA and Papanicolaou test cotesting. Obstet Gynecol. 2009;113:595–600. doi: 10.1097/AOG.0b013e3181996ffa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kagawa-Singer M, Pourat N. Asian American and Pacific Islander breast and cervical carcinoma screening rates and Healthy People 2000 objectives. Cancer. 2000;89:696–705. doi: 10.1002/1097-0142(20000801)89:3<696::aid-cncr27>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 5.Mannava P, Abdullah A, James C, Dodd R, Annear PL. Health systems and noncommunicable diseases in the Asia-Pacific region: a review of the published literature. Asia Pac J Public Health. 2013;27:NP1–NP19. doi: 10.1177/1010539513500336. [DOI] [PubMed] [Google Scholar]
- 6.Heaney CA, Israel BA. Social networks and social support. In: Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education: Theory, Research, and Practice. 3rd ed Jossey-Bass; San Francisco, CA: 2002. pp. 185–209. [Google Scholar]
- 7.US Census Bureau . 2010 Census SF1, Tables P5 and P6. US Census Bureau; Washington, DC: [Accessed August 25, 2015]. 2010. www.factfinder.census.gov/ [Google Scholar]
- 8.Empowering Pacific Islander Communities. Asian American Advancing Justice . A Community of Contrasts: Native Hawaiians and Pacific Islanders in the United States. Empowering Pacific Islander Communities, Asian American Advancing Justice; Los Angeles, CA: [Accessed August 25, 2015]. 2014. http://www.advancingjustice.org/sites/default/files/A_Community_of_Contrasts_NHPI_US_2014-1.pdf. [Google Scholar]
- 9.Heaney CA, Israel BA. Social networks and social support. In: Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education: Theory, Research, and Practice. 4th ed Jossey-Bass; San Francisco, CA: 2008. pp. 189–210. [Google Scholar]
- 10.Langford CP, Bowsher J, Maloney JP, Lillis PP. Social support: a conceptual analysis. J Adv Nurs. 1997;25:95–100. doi: 10.1046/j.1365-2648.1997.1997025095.x. [DOI] [PubMed] [Google Scholar]
- 11.Pasick RJ, Barker JC, Otero-Sabogal R, Burke NJ, Joseph G, Guerra C. Intention, subjective norms, and cancer screening in the context of relational culture. Health Educ Behav. 2009;36(5 suppl):91S–110S. doi: 10.1177/1090198109338919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen JY, Diamant AL, Kagawa-Singer M, Pourat N, Wold C. Disaggregating data on Asian and Pacific Islander women to assess cancer screening. Am J Prev Med. 2004;27:139–145. doi: 10.1016/j.amepre.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 13.Special Service for Groups, Inc . REACH 2010–PATH for Women—Voices From the Community—Eight Personal Experiences With Community Participatory Action Research. Special Service for Groups, Inc; Los Angeles, CA: [Accessed August 25, 2015]. 2004. http://ocapica.org/us/wp-content/uploads/2011/09/PATH_Voices-2004.pdf. [Google Scholar]
- 14.Tisnado DM, Sablan-Santos L, Guevara L, et al. A case study in Chamorro community and academic engagement for a community-partnered research approach. Calif J Health Promot. 2010;8(Special Issue: Cancer Control Among Pacific Islanders):39–51. [PMC free article] [PubMed] [Google Scholar]
- 15.Matsunaga DS, Enos R, Gotay CC, et al. Participatory research in a Native Hawaiian community. The Wai’anae Cancer Research Project. Cancer. 1996;78(7 suppl):1582–1586. [PubMed] [Google Scholar]
- 16.Kagawa-Singer M, Tanjasiri SP, Valdez A, Yu H, Foo MA. Outcomes of a breast health project for Hmong women and men in California. Am J Public Health. 2009;99(suppl 2):S467–S473. doi: 10.2105/AJPH.2008.143974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hokama T, Binna C. Progress in island health in the Asia-Pacfic region. Asia Pac J Public Health. 2015;27:29–32. doi: 10.1177/1010539514561085. [DOI] [PubMed] [Google Scholar]
- 18.Tanjasiri SP, Weiss J, Sablan-Santos L, et al. Cultural adaptations of study recruitment procedures in a randomized study of Pap testing among Pacific Islander women and men in southern California. Prog Community Partnersh. 2015 In press. [Google Scholar]
- 19.Sherbourne CD, Stewart AL. The MOS Social Support Survey. Soc Sci Med. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 20.Shulz AJ, Israel BA, Lantz P. Instrument for evaluating dimensions of group dynamics within community-based participatory research partnerships. Eval Program Plann. 2003;26:249–262. [Google Scholar]
- 21.Strahan R, Gerbasi K. Short, homogeneous versions of the Marlow-Crowne social desirability scale. J Clin Psychol. 1972;28:191–193. [Google Scholar]
- 22.Mishra SI, Aoelua PL, Hubbell FA. Knowledge of and attitudes about cancer among American Samoans. Cancer Detect Prev. 2000;24:186–195. [PubMed] [Google Scholar]
- 23.Dang J, Lee J, Tran JH. Knowledge, attitudes, and beliefs regarding breast and cervical cancer screening among Cambodian, Laotian, Thai, and Tongan women. J Cancer Educ. 2010;25:595–601. doi: 10.1007/s13187-010-0082-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang R, Hempton B, Dugan J, Komives S. [Accessed August 25, 2015];Cultural differences: why do Asians avoid extreme responses? Survey Pract. 2013 1(3) http://www.surveypractice.org/index.php/SurveyPractice/article/view/224. [Google Scholar]
- 25.Tanjasiri SP, Mouttapa M, Sablan-Santos L, Quitugua LF. Exploring factors promoting cervical cancer screening among Chamorro women in California. J Cancer Educ. 2012;27:725–730. doi: 10.1007/s13187-012-0394-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tanjasiri SP, Kagawa-Singer M, Foo MA, et al. Breast cancer screening among Hmong women in California. J Cancer Educ. 2001;16:50–54. doi: 10.1080/08858190109528725. [DOI] [PubMed] [Google Scholar]
- 27.US Department of Health and Human Services [Accessed May 19, 2014];Office of Disease Prevention and Health Promotion. Healthy People 2020. http://www.healthypeople.gov/2020/
- 28.US Prevention Services Task Force [Accessed May 19, 2014];The community guide: what works to promote health. http://www.thecommunityguide.org/index.html.