1. Introduction
The association between trauma-related disorders, such as post-traumatic stress disorder (PTSD), and problematic substance use remains alarmingly high. In the National Epidemiologic Survey on Alcohol and Related Conditions (2011), almost half (46.6%) of individuals meeting criteria for lifetime PTSD had a comorbid substance use disorder (SUD). Additional studies have found that comorbidity rates for PTSD and SUD range between 25%–55% across various clinical populations (Brown & Ryan, 2004; Brown, Read, & Kahler, 2003; Kessler et al., 1995; Pietrzak, Goldstein, Southwick, & Grant, 2011). Several studies have shown that experienced trauma is associated with multiple indices of substance abuse, including problematic use (Lisak & Miller, 2003), severity of substance-related negative consequences (Asberg & Renk, 2012), and heightened risk for relapse following treatment (Souza & Spates, 2008). While these maladaptive coping strategies may temporarily help alleviate or avoid discomfort, they often lead to longer-term negative consequences (Tiet, Rosen, Cavella, Moos, Finney, & Yesavage, 2006).
Research suggests that there may be bidirectional effects that perpetuate this cycle, such that consequences of substance use exacerbate PTSD symptoms, and PTSD symptoms increase risk of problematic substance use and increase risk of exposure to situations in which traumatic experiences and resulting PTSD are more likely to occur (Read, Griffin, Wardell, & Ouimette, 2014, Stewart & Conrod, 2003). The presence of an SUD not only increases risk for and symptom expression of PTSD, it also predicts poorer treatment outcomes for those individuals who do seek treatment (Ouimette, Finney & Moos, 1999).
Several studies indicate that a factor underlying both SUDs and PTSD is mindfulness, often described as an intentional, present-centered and nonjudgmental awareness (Kabat-Zinn, 1990). The Five-Facet Mindfulness Questionnaire (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006), commonly used in psychology literatures, describes mindfulness as comprised of 5 constituents factors: acting with awareness, observing, describing, nonjudgment, and nonreactivity. Levels of mindfulness may be negatively affected by trauma, as evidenced in a study by Elices and colleagues(2015) suggesting childhood abuse is negatively associated with mindfulness, particularly factors of acting with awareness and nonjudgment (Michal, Beutel, Jordan, Zimmermann, Wolters, & Heidenreich, 2007). Mindfulness has also been shown to be inversely related to addictive behaviors (Karyadi, VanderVeen, & Cyders, 2014) with lower levels of mindfulness negatively predicting the presence of a SUD (Levin, Dalrymple, & Zimmerman, 2014), as well as intensity of the disorder, and comorbid PTSD and depression (Shorey, Brasfield, Anderson, & Stuart, 2014).
Conversely, mindfulness has been shown to be positively associated with approach-based coping and improvement to treatment outcomes in individuals with trauma history (Vujanovic, Niles, Pietrefesa, Schmertz, & Potter, 2011), and negatively related to severity of avoidance-related PTSD symptoms (Thompson & Waltz, 2010), with evidence that the non-reactivity element of mindfulness (Baer et al., 2006) may be uniquely associated with overall positive PTSD outcomes (Kalill, Treanor, & Roemer, 2014). The nonjudgmental acceptance of experience, a central aspect of mindfulness (Kabat-Zinn, 1990), appears to predict a reduction in PTSD symptomology and an increase in potential treatment efficacy (Vujanovic, Youngwirth, Johnson, & Zvolensky, 2009). These findings suggest that mindfulness training may foster more adaptive coping responses for individuals with comorbid PTSD and SUDs, as it is associated with the symptom sets independently (Karyadi, VanderVeen, & Cyders, 2014; Shorey, Brasfield, Anderson, & Stuart, 2014; Vujanovic et al., 2009), as well with mechanisms that may underlie PTSD-SUD comorbidity.
Other recent studies exploring this relationship have yielded similar results, indicating that global measures of dispositional mindfulness, including factors of observing, describing, acting with awareness, and non judgmental acceptance, have a inverse predictive influence on post traumatic stress symptoms and craving (Garland & Lewis, 2013), and that nonjudgmental acceptance of experience exhibits a partial mediating role in the relationship between cannabis and alcohol use motives and PTSD symptom severity with nonjudgmental acceptance negatively predicting motives for substance use (Bonn-Miller, Vujanoiv, Twohig, Medina, & Huggins, 2010)
Given the common processes and mechanisms underlying mindfulness and the development and maintenance of PTSD symptoms and SUDs, the potential benefits of mindfulness in this endemic comorbidity is worthy of further exploration. The current study aims to replicate and expand the foundation of literature assessing effects of mindfulness in the PTSD-addiction cycle by assessing whether mindfulness, and its constituent facets, have a mediating role in the relationship between PTSD symptoms and severity of substance dependence. The study assesses a broader index of substance abuse that includes psychological components of addictive behavior, such as feeling out of control and worry regarding use (Gossop, et al., 1995), rather than solely amount of use of a specific substance, cravings, or motives for use. It was hypothesized that mindfulness would be a significant mediator in the relationship between PTSD symptoms and substance use, such that levels of mindfulness would partially explain the predictive relationship between PTSD symptoms and severity of substance dependence. Results of this study may provide valuable information on these interrelated processes, and potentially inform interventions for dually-diagnoses populations, specifically highlighting potential mindfulness-based mechanisms that may help substance abuse treatment for individuals with PTSD.
2. Method
2.1 Participants
Data in the current study were drawn from a larger multi-site study of Mindfulness-Based Relapse Prevention, an outpatient aftercare program for adults (N=286) with substance use disorders recruited via flyers posted at the treatment facilities and informational sessions held by researchers (see Bowen, et al., 2014 for full study description). This population has reported high rates of trauma exposure in previous studies (Brown & Ryan, 2004; P. J. Brown, Read, & Kahler, 2003; Kessler et al., 1995; Pietrzak, Goldstein, Southwick, & Grant, 2011), providing an opportunity to assess the role of mindfulness in the PTSD-SUD cycle. The current sample reported an average 2.34 (0.84) on PTSD checklist items, indicating moderate levels of PTSD symptoms (Weathers, Litz, Herman, Huska, & Keane, 1994). Data for the current study were drawn from selected measures administered prior to random assignment to original study treatment condition. All procedures were approved by the associated Institutional Review Board.
2.2 Measures
PTSD symptoms were assessed in the current sample with the PTSD Checklist – Civilian Version (PCL-C; Weathers, et al., 1994). The PCL-C is a commonly used measure of PTSD symptoms, with items corresponding to DSM-IV criteria for PTSD. Items ask about severity of experienced symptoms, such as “Repeated disturbing memories, thoughts, or images of a stressful experience from the past” on a 5-item Likert response scale. Participants were instructed to indicate to what extent they had been bothered by each of a list of problems in response to stressful life experiences (e.g., repeated disturbing memories, thoughts, or images of a stressful experience) over the past month. While not a diagnostic tool, higher endorsement of trauma-symptoms on the PCL-C can indicate the presence of PTSD. Across studies, the PCL-C has demonstrated good to acceptable psychometric properties (Wilkins, Lang, & Norman, 2011), including in the current sample (α = .93).
Substance use severity was measured by the Severity of Dependence Scale (SDS: Gossop, et al., 1995). The SDS is a five-item assessment of the psychological components linked to substance dependence and use over the 90 days prior to entering treatment, scored on a 4-point scale (0–4), with items such as, “Do you think your use of drugs and/or alcohol was out of control?”. The SDS has demonstrated good psychometric properties across multiple samples in the initial validation study (Amaro, Spear, Vallejo, Conron, & Black, 2014; Gossop et al., 1995), with α = .86 in the current sample.
The Five Facet Mindfulness Questionnaire (FFMQ; Baer et al., 2006) is a 39-item measure assessing individuals’ dispositional tendency to be mindful in daily life as indicated by a 5-point Likert-type scale, with items such as, “When I'm walking, I deliberately notice the sensations of my body moving.” The FFMQ is based on exploratory and confirmatory factor analyses of previous questionnaires. In past research, the FFMQ was found to demonstrate good internal consistency and convergent validity (Baer et al. 2006, 2008). Reliability was excellent in the current sample (α =.86).
2.3 Analysis
Multiple regression analses assessed the relation between PTSD symptoms and mindfulness (A-path), mindfulness and severity of dependence, (B-path), and PTSD symptoms and severity of dependence (C-Path). The indirect effect (AB path) was calculated using a 95% confidence interval from a 1000 bootstrapped sampling distribution, following Preacher and Hayes (2008). Confidence intervals for the AB path that do not contain zero indicate a significant indirect effect (i.e., mediation).
3. Results
The primary goal of our analyses was to assess the association between PTSD symptoms, mindfulness, and severity of substance abuse using a cross-sectional model. Data were examined for outliers and normality of distribution, and found to be within the acceptable ranges. Descriptive statistics and bivariate correlation coefficients for all variables in the analyses are shown in Tables 1 and 2, respectively.
Table 1.
Descriptive Statistics
| Variable | No. | (%) |
|---|---|---|
| Gender | ||
| Male | 200 | 71.4 |
| Female | 79 | 28.2 |
| Other | 1 | 0.4 |
| Race/ethnicity | ||
| Hispanic or Latino/Latina | 22 | 7.8 |
| White | 145 | 51.4 |
| Black or African American | 61 | 21.6 |
| Native American | 18 | 6.4 |
| Asian | 2 | 0.7 |
| Native Hawaiian/Pacific | 2 | 0.7 |
| Islander | 27 | 9.6 |
| Mixed | 5 | 1.8 |
| Employment | ||
| Employed | 103 | 36.3 |
| Unemployed | 181 | 63.7 |
| Education level | ||
| Did not complete high school | 26 | 9.2 |
| High school graduate/GED | 129 | 45.7 |
| Some college | 69 | 24.5 |
| Community college | 42 | 14.9 |
| College degree | 16 | 5.7 |
| Variable | Mean (SD) | Range |
| Age | 38.47 (10.93) | 19–62 |
| PCL Average Response Value | 2.34 (0.84) | 1–5 |
| SDS Total Score | 9.42 (4.18) | 0–15 |
| FFMQ Average Response Value | 3.38 (0.45) | 2.1–4.5 |
Abbreviations: GED, General Educational Development; PCL, Patient Checklist; SDS, Severity of Dependence Scale; FFMQ, Five Facet Mindfulness Questionnaire
Table 2.
Intercorrelations of PTSD Symptoms, Mindfulness and Severity of Dependence
| Variable | 1 | 2 | 3 |
|---|---|---|---|
| 1. PCL-C Average Response Value |
- | ||
| 2. SDS Total Score | .27** | - | |
| 3. FFMQ Average Response Value |
−.44** | −.23** | - |
Note. PCL-C – PTSD Checklist-Civilian Version; SDS – Severity of Dependence Scale; FFMQ – Five Facet Mindfulness Questionnaire
p < .01
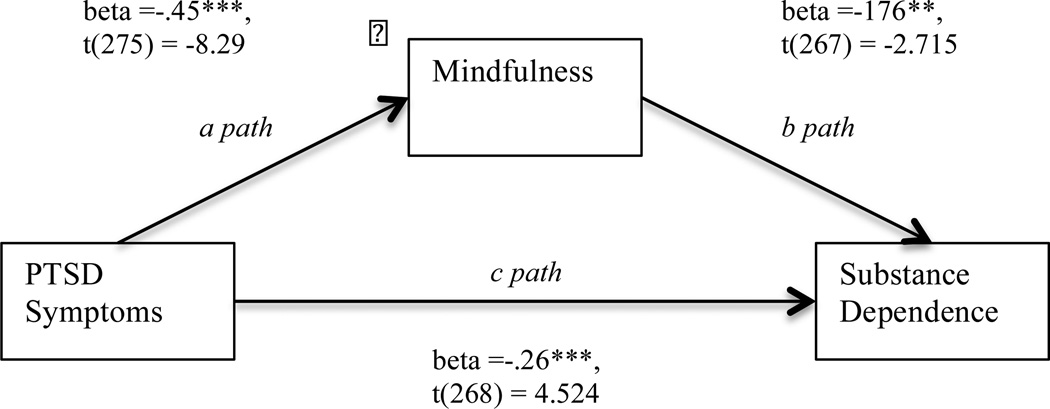
In the following analyses, gender and age were included as a covariates, as it they were significantly correlated with the dependent variable, substance dependence (gender: rpb = .216, p <.001; age: r = .162, p < .01) To assess the mediating role of mindfulness in the relationship between PTSD symptoms and severity of substance dependence, we first used linear regressions to test the direct effect of PTSD symptoms on severity of substance dependence (C-path). The direct effect was significant (beta = .272, t(264) = 4.765, p <.001), with PTSD symptom severity positively associated with severity of substance dependence. Next, we assessed whether mindfulness was significantly predicted from PTSD symptoms (A-Path), and found this relationship to be significant (beta = −.452, t(271) = −8.288, p < .001), with higher PTSD symptom severity predicting lower levels of mindfulness. The relationship between mindfulness and substance use, accounting for effects of PTSD symptoms (B path) was also significant (beta = −.165, t(263) = −2.577, p = .011), yielding an inverse relationship between mindfulness and severity of dependence (see Figure 1). To assess whether mindfulness mediated the relation between PTSD symptoms and severity of dependence, we calculated the indirect effect (AB path) using a 99% CI from a 1000 bootstrapped sampling distribution, using the PROCESS macro (Hayes, 2002) for SPSS version 22. Significance for the AB path was determined if the 95% CI did not include 0. Results indicated a significant mediating role of the total FFMQ score in the relationship between PTSD symptoms in the prediction of SDS (indirect effect AB = 0.39, 95% CI [0.10, .70]). The mediation model explained approximately 29% of the variance in severity of dependence (PM = .289).
Figure 1.
Mediation Model
To further elucidate the mediating role of mindfulness, we assessed each of the five facets of the FFMQ. The CI for facets of observe (95% CI [−0.12, .04]), describe (95% CI [−.02, .34]), and nonreact (95% CI: [−.28, .004]) each included 0, indicating nonsignificance. However, both acting with awareness (indirect effect AB = .67, 95% CI [.29, 1.04]), and nonjudging (indirect effect AB =.41, 95% CI [.12, .77] were significant mediators. In separate models testing these factors as mediators, acting with awareness explained approximately 49% of the variance between PTSD symptoms and severity of dependence, and nonjudging approximately 31%.
The relationship of interest in the current study was potentially protective effects of mindfulness coupled with PTSD symptoms, rather than the possible buffering effects of mindfulness in individuals with substance dependence. However, due to the cross-sectional nature of the data, and to the cyclical and bidirectional nature of PTSD symptoms and substance abuse, an alternative reverse mediation hypothesis was also tested, assessing mindfulness as a mediator between severity of substance dependence and PTSD symptoms. This allowed us to assess the role of mindfulness in relationships previously discussed that suggest substance dependence increases risk of trauma, and subsequently PTSD symptoms.
Results from the reverse alternative model indicated a significant mediating role of the total FFMQ score (indirect effect AB = 0.02, 95% CI [0.01, .04]). The mediation model explained approximately 40% of the variance in severity of dependence (PM = .40).
Subsequent to this finding, we again assessed each of the five facets of the FFMQ in separate models. The CI for facets of observe (95% CI [−0.003, .003]), and nonreact (95% CI: [−.01, .003]) each included 0, indicating nonsignificance. However, the facets describe (indirect effect AB = .01, 95% CI [.003, .02]), acting with awareness (indirect effect AB = .03, 95% CI [.02, .05]), and nonjudging (indirect effect AB =.02, 95% CI [.01, .04] were each significant mediators: describe explained approximately 16% of the variance between PTSD symptoms and severity of dependence, acting with awareness approximately 59%, and nonreact approximately 40%.
4. Discussion
The current findings support the hypothesis that mindfulness is a significant mediating factor in the relationship between symptoms of PTSD and severity of substance dependence, such that higher levels of PTSD symptoms are associated with lower levels of mindfulness, and subsequently more severe substance dependence. Specifically, acting with awareness and nonjudging emerged as significant mediating facets.
The relationship between PTSD and SUDs has been established in numerous studies, and research suggests avoidant coping styles play a mediating role in this relationship (Asberg & Renk, 2012; P. Ouimette & Brown, 2003; Brown, Read & Kahler, 2003; Grosso, et al., 2014). By its nature, mindfulness training exposes an individual to any and all experienced phenomena, even that which is typically or habitually avoided. Through a gentle, nonjudgmental and curious exploration of experience, mindfulness practitioners learn to approach challenging or aversive experiences, including the cognitive and affective discomfort characteristic of PTSD, rather than reactively avoiding them. Via awareness of this process, practice of alternative approach-based skills, increasing awareness and allowing an accepting, gentle interoceptive exposure to these internal aversive phenomena, mindfulness may shift avoidant-based coping, such as substance use, in the presence of PTSD symptoms.
While treatments for PTSD and comorbid SUD may maintain a primary focus on symptom reduction (Ouimette & Brown, 2003; Norman et al., 2012), the current study suggests that presence of symptoms may not be the sole factor in the PTSD-addiction cycles. An individual’s relationship to these symptoms, and the manner in which they relate or react to symptoms, may be critical to assess, particularly in relation to substance abuse. Specifically, results from the current study suggest that acting with awareness in the presence of symptoms (versus reacting habitually), and having an accepting/nonjudging stance towards experience, may be critical factors in attenuating the relationship between trauma symptoms and substance dependence. Similar to findings by Vujanovic and colleagues(2009), a nonjudgmental acceptance of experience appears to be inversely related to PTSD symptomology, and, as suggested by their study, may be a means by which treatment efficacy can be increased.
The relationship between problematic substance use and mindfulness can be further illustrated by the salutary effects of mindfulness-based interventions specifically designed to target problematic substance use. Relationship patterns between variables seen in the current study provide promise for mindfulness-based approaches in comorbid PTSD-SUD populations.
Beyond the positive primary impact on both PTSD and SUD symptoms, it appears that training in mindfulness could potentially disrupt the relationship between symptoms of PTSD and subsequent problematic substance use. Training in mindfulness, such as that seen in mindfulness-based interventions (MBIs; Kabat-Zinn et al., 1990; Segal, Williams, & Teasdale, 2013; Bowen Chawla & Marlatt, 2011), has shown promise in disrupting the pattern of avoidance and subsequent symptom development for individuals who have experienced trauma. Future clinical studies should assess how mindfulness-based treatments specifically target these processes, perhaps emphasizing awareness of one’s actions and an strengthening an accepting, nonjudgmental stance, and whether such targeted changes predict symptoms of PTSD and substance-related outcomes and treatment and relapse trajectories.
Results from the alternative reverse mediation hypothesis, supporting mindfulness as a mediating factor in the relationship between substance dependence and PTSD symptoms, also holds potential clinical value, and suggests mindfulness may be important in attenuating both causal directions of this comorbidity; increases in mindfulness, specifically ability to describe and respond nonjudgmentally towards inner experiences, and awareness of one’s actions, may help break the cyclical pattern of substance dependence and PTSD symptoms, wherein each increases risk for occurrence or severity of the other.
Alongside the potential contributions of the current study, there are also considerable limitations to consider. Foremost, data used in the study are cross-sectional, limiting the extent to which causal inferences can be drawn. Further limitations include assessment of PTSD symptoms. Data were collected via self-report measures, and are thus subject to over- or under-reporting, or influence by social desirability factors, and PTSD symptoms were assessed in accordance with DSM-IV criteria and need to be replicated using DSM 5 criteria. Regarding use of the PCL-C to measure PTSD symptoms, participants did not specify whether they had experienced a traumatic event, but were asked to answer items in response to traumatic events in the past. Thus, the construct validity of the measure may be influenced, and scores may be reflective of negative affect (Conybeare, Behar, Solomon, Newman, & Borkovec, 2012). Finally, although the FFMQ has demonstrated psychometric strengths (Baer et al., 2008), there is significant debate about the validity of any self-report measures of mindfulness (Brown & Ryan, 2004), specifically in clinical populations (Manuel, Somohano & Bowen, under review).
The experience of trauma has both immediate and long-lasting effects on impacted individuals. Traumatic experiences can lead to a diagnosis of PTSD, higher levels of negative affect, and to the development of maladaptive coping styles in attempt to ameliorate these states. These resultant effects put an individual at greater risk for problematic substance use and dependence. A more sophisticated understanding of the multiple, interrelated processes underlying substance use disorders in individuals exposed to trauma and subsequent PTSD may help inform interventions. Knowledge on this topic can be informed through the furthered investigation of other SUD populations (i.e., non-treatment seeking, inpatient, mandated) to indicate differences and/or similarities between these interconnected variables. With such an understanding, clinicians can better target these processes, and disrupt the link between PTSD symptoms, harmful behaviors, and lasting consequences.
Highlights.
Mindfulness has shown an inverse relationship with avoidant coping styles, PTSD symptoms, and substance use disorders.
Both trait levels of mindfulness and mindfulness training are associated with reduced symptomology and increase treatment efficacy for comorbid substance abuse and PTSD.
The current study suggests a mediating role of mindfulness in the relationship between PTSD symptoms and severity of substance dependence; specifically, the acting with awareness and nonjudging mindfulness facets were significant mediators.
An alternative reverse mediation model suggests mindfulness also mediates the relationship between substance dependence and PTSD symptoms, which may point to its role in the bidirectional and often cyclical nature of this common comorbidity.
These findings contribute to our understanding of the underlying processes of comorbid PTSD symptoms and substance use, and may inform key treatment targets for this population.
Acknowledgments
Role of Funding Sources
Funding for this study was provided by NIDA Grant R01 DA025764-01A1. NIDA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Disclosure
Contributors All authors must have materially participated in the manuscript preparation. Authors De Boer and Bergman conducted literature searches and provided summaries of previous research studies. Author Bowen conducted the statistical analysis. All authors contributed to original drafts and have approved the final manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest.
References
- Amaro H, Spear S, Vallejo Z, Conron K, Black DS. Feasibility, acceptability, and preliminary outcomes of a mindfulness-based relapse prevention intervention for culturally-diverse, low-income women in substance use disorder treatment. Subst Use Misuse. 2014;49(5):547–559. doi: 10.3109/10826084.2013.852587. [DOI] [PubMed] [Google Scholar]
- Asberg K, Renk K. Substance use coping as a mediator of the relationship between trauma symptoms and substance use consequences among incarcerated females with childhood sexual abuse histories. Subst Use Misuse. 2012;47(7):799–808. doi: 10.3109/10826084.2012.669446. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, Williams JMG. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Bartone PT, Hystad SW, Eid J, Brevik JI. Psychological hardiness and coping style as risk/resilience factors for alcohol abuse. Military Medicine. 2012;177(5):517–524. doi: 10.7205/milmed-d-11-00200. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Vujanovic AA, Twohig MP, Medina JL, Huggins JL. Posttraumatic stress symptom severity and marijuana use coping motives: A test of the mediating role of non-judgmental acceptance within a trauma-exposed community sample. Mindfulness. 2010;1(2):98–106. [Google Scholar]
- Bowen S, Chawla N, Marlatt GA. Mindfulness-based relapse prevention for addictive behaviors: A clinician's guide. New York, NY, US: Guilford Press; 2011. [Google Scholar]
- Bowen S, Enkema MC. Relationship between dispositional mindfulness and substance use: Findings from a clinical sample. Addictive Behaviors. 2012;39(3):532. doi: 10.1016/j.addbeh.2013.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi S, Grow J, Chawla N, Hsu S, Larimer ME. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders. Jama Psychiatry. 2014;71(5):547–556. doi: 10.1001/jamapsychiatry.2013.4546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, Ryan RM. Perils and promise in defining and measuring mindfulness: Observations from experience. Clinical Psychology: Science and Practice. 2004;11(3):242–248. [Google Scholar]
- Brown PJ, Read JP, Kahler CW. Comorbid posttraumatic stress disorder and substance use disorders: Treatment outcomes and the role of coping. In: Brown PJ, editor. Trauma and Substance Abuse: Causes, Consequences, and Treatment of Comorbid Disorders. Washington, DC, US: American Psychological Association; 2003. pp. 171–188. [Google Scholar]
- Brown KW, Ryan RM. Perils and Promise in Defining and Measuring Mindfulness: Observations From Experience. Clinical Psychology: Science and Practice. 2004;11(3):242–248. [Google Scholar]
- Bryant RA, Keane TM. Post-traumatic stress disorder. In: Castonguay LG, Oltmanns TF, editors. Psychopathology: From science to clinical practice. New York, NY: Guilford; 2013. pp. 172–198. [Google Scholar]
- Chiesa A, Serretti A. Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Subst Use Misuse. 2014;49(5):492–512. doi: 10.3109/10826084.2013.770027. [DOI] [PubMed] [Google Scholar]
- Conybeare D, Behar E, Solomon A, Newman MG, Borkovec TD. The PTSD Checklist—Civilian Version: Reliability, validity, and factor structure in a nonclinical sample. Journal Of Clinical Psychology. 2012;68(6):699–713. doi: 10.1002/jclp.21845. [DOI] [PubMed] [Google Scholar]
- Dakwar E, Mariani JP, Levin FR. Mindfulness impairments in individuals seeking treatment for substance use disorders. The American Journal of Drug and Alcohol Abuse. 2011;37(3):165–169. doi: 10.3109/00952990.2011.553978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dermody SS, Cheong J, Manuck S. An evaluation of the stress-negative affect model in explaining alcohol use: The role of components of negative affect and coping style. Subst Use Misuse. 2013;48(4):297–308. doi: 10.3109/10826084.2012.761713. [DOI] [PubMed] [Google Scholar]
- Elices M, Pascual JC, Carmona C, Martín-Blanco A, Feliu-Soler A, Ruiz E, Soler J. Exploring the relation between childhood trauma, temperamental traits and mindfulness in borderline personality disorder. BMC Psychiatry. 2015;15:180. doi: 10.1186/s12888-015-0573-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Roberts-Lewis A. Differential roles of thought suppression and dispositional mindfulness in posttraumatic stress symptoms and craving. Addictive behaviors. 2013;38(2):1555–1562. doi: 10.1016/j.addbeh.2012.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gossop M, Darke S, Griffiths P, Hando J, Powis B, Hall W, Strang J. The Severity of Dependence Scale (SDS): psychometric properties of the SDS in English and Australian samples of heroin, cocaine and amphetamine users. Addiction. 1995;90(5):607–614. doi: 10.1046/j.1360-0443.1995.9056072.x. [DOI] [PubMed] [Google Scholar]
- Grosso JA, Kimbrel NA, Dolan S, Meyer EC, Kruse MI, Gulliver SB, Morissette SB. A Test of Whether Coping Styles Moderate the Effect of PTSD Symptoms on Alcohol Outcomes. Journal of Traumatic Stress. 2014;27(4):478–482. doi: 10.1002/jts.21943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J University of Massachusetts Medical, C. W.,& Stress Reduction, C. Full Catastrophe Living : Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York, NY: Delacorte Press; 1990. [Google Scholar]
- Kalill K, Treanor M, Roemer L. The Importance of non-reactivity to posttraumatic stress symptoms: A case for mindfulness. Mindfulness. 2014;5(3):314–321. [Google Scholar]
- Karyadi KA, VanderVeen J, Cyders MA. A meta-analysis of the relationship between trait mindfulness and substance use behaviors. Drug and Alcohol Dependence. 2014:1–10. doi: 10.1016/j.drugalcdep.2014.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. 1995 doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv Rev Psychiatry. 1997;4(5):231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Levin ME, Dalrymple K, Zimmerman M. Which facets of mindfulness predict the presence of substance use disorders in an outpatient psychiatric sample? Psychol Addict Behav. 2014;28(2):498–506. doi: 10.1037/a0034706. [DOI] [PubMed] [Google Scholar]
- Lisak DM, PM . PTSD and Substance Abuse Comorbidity. Washington DC: American Psychological Association; 2003. Childhood abuse, PTSD, substance abuse and violence; pp. 73–88. [Google Scholar]
- Manuel J, Somohano V, Bowen S. Mindfulness Practice and its Relationship to the Five-Facet Mindfulness Questionnaire. Mindfulness. (under review) [Google Scholar]
- Ménard KS, Arter ML. Police officer alcohol use and trauma symptoms: Associations with critical incidents, coping, and social stressors. International Journal of Stress Management. 2013;20(1):37–56. [Google Scholar]
- Michal EM, Beutel EM, Jordan EJ, Zimmermann EM, Wolters ES, Heidenreich ET. Depersonalization, mindfulness, and childhood trauma. The Journal of Nervous and Mental Disease. 2007;195(8):693–696. doi: 10.1097/NMD.0b013e31811f4492. [DOI] [PubMed] [Google Scholar]
- Moore TM, Seavey A, Ritter K, McNulty JK, Gordon KC, Stuart GL. Ecological momentary assessment of the effects of craving and affect on risk for relapse during substance abuse treatment. Psychology of Addictive Behaviors. 2014;28(2):619–624. doi: 10.1037/a0034127. [DOI] [PubMed] [Google Scholar]
- Norman S, Myers U, Wilkins K, Goldsmith A, Hristova V, Huang Z, McCullough K, Robinson S. Review of biological mechanisms and pharmacological treatments of comorbid PTSD and substance use disorder. Neuropharmacology. 2012;62:542–551. doi: 10.1016/j.neuropharm.2011.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouimette P, Brown PJ. Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders. American Psychological Association. 2003;315 [Google Scholar]
- Ouimette PC, Finney JW, Moos RH. Two-year posttreatment functioning and coping of substance abuse patients with posttraumatic stress disorder. Psychology of Addictive Behaviors. 1999;13(2):105–114. [Google Scholar]
- Palmer A, Rodger S. Mindfulness, stress, and coping among university students. Canadian Journal of Counselling. 2009;43(3):198–212. [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Anxiety Disord. 2011;25(3):456–465. doi: 10.1016/j.janxdis.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Read JP, Griffin MJ, Wardell JD, Ouimette P. Coping, PTSD symptoms, and alcohol involvement in trauma-exposed college students in the first three years of college. Psychology of Addictive Behaviors. 2014;28(4):1052–1064. doi: 10.1037/a0038348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Williams JG, Teasdale JD. Mindfulness-based cognitive therapy for depression. 2nd. New York, NY, US: Guilford Press; 2013. [Google Scholar]
- Shorey RC, Brasfield H, Anderson S, Stuart GL. Mindfulness deficits in a sample of substance abuse treatment seeking adults: A descriptive investigation. Journal of Substance Use. 2014;19(1–2):194–198. doi: 10.3109/14659891.2013.770570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza T, Spates CR. Treatment of PTSD and substance abuse comorbidity. (Report) The Behavior Analyst Today. 2008;9(1):11. [Google Scholar]
- Stewart SH, Conrod PJ. Psychosocial models of functional associations between posttraumatic stress disorder and substance use disorder. In: Brown PJ, editor. Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders. Washington, DC, US: American Psychological Association; 2003. pp. 29–55. [Google Scholar]
- Thompson BL, Waltz J. Mindfulness and experiential avoidance as predictors of posttraumatic stress disorder avoidance symptom severity. Journal of Anxiety Disorders. 2010;24(4):409–415. doi: 10.1016/j.janxdis.2010.02.005. [DOI] [PubMed] [Google Scholar]
- Tiet QQ, Rosen C, Cavella S, Moos RH, Finney JW, Yesavage J. Coping, symptoms, and functioning outcomes of patients with posttraumatic stress disorder. Journal of Traumatic Stress. 2006;19(6):799–811. doi: 10.1002/jts.20185. [DOI] [PubMed] [Google Scholar]
- Veenstra MY, Lemmens PH, Friesema IH, Tan FE, Garretsen HF, Knottnerus J, Zwietering PJ. Coping style mediates impact of stress on alcohol use: A prospective population-based study. Addiction. 2007;102(12):1890–1898. doi: 10.1111/j.1360-0443.2007.02026.x. [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Bonn-Miller MO, Marlatt GA. Posttraumatic stress and alcohol use coping motives among a trauma-exposed community sample: The mediating role of non-judgmental acceptance. Addictive behaviors. 2011;36(7):707–712. doi: 10.1016/j.addbeh.2011.01.033. [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Niles B, Pietrefesa A, Schmertz S, Potter CM. Mindfulness in the treatment of posttraumatic stress disorder among military veterans. Professional Psychology-Research And Practice. 2011;42(1):24–31. [Google Scholar]
- Vujanovic AA, Youngwirth NE, Johnson KA, Zvolensky MJ. Mindfulness-based acceptance and posttraumatic stress symptoms among trauma-exposed adults without axis I psychopathology. Journal of Anxiety Disorders. 2009;23(2):297–303. doi: 10.1016/j.janxdis.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers LBF, Herman D, Huska J, Keane T. The PTSD Checklist: Reliability, validity, & diagnositic utility; Paper presented at the Annual Meeting of the Internation Society of Traumatic Stress Studies; San Antonio, TX. 1993. [Google Scholar]
- Weinstein N, Brown KW, Ryan RM. A multi-method examination of the effects of mindfulness on stress attribution, coping, and emotional well-being. Journal of Research in Personality. 2009;43(3):374–385. [Google Scholar]
- Wilkins KC, Lang Aj Fau - Norman SB, Norman SB. Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depress Anxiety. 2011;28(7):596–606. doi: 10.1002/da.20837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Black DS. Unresolved issues in the application of mindfulness-based interventions for substance use disorders. Subst Use Misuse. 2014;49(5):601–604. doi: 10.3109/10826084.2014.852797. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S. Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. Journal of Consulting and Clinical Psychology. 2010;78(3):362–374. doi: 10.1037/a0019172. [DOI] [PMC free article] [PubMed] [Google Scholar]