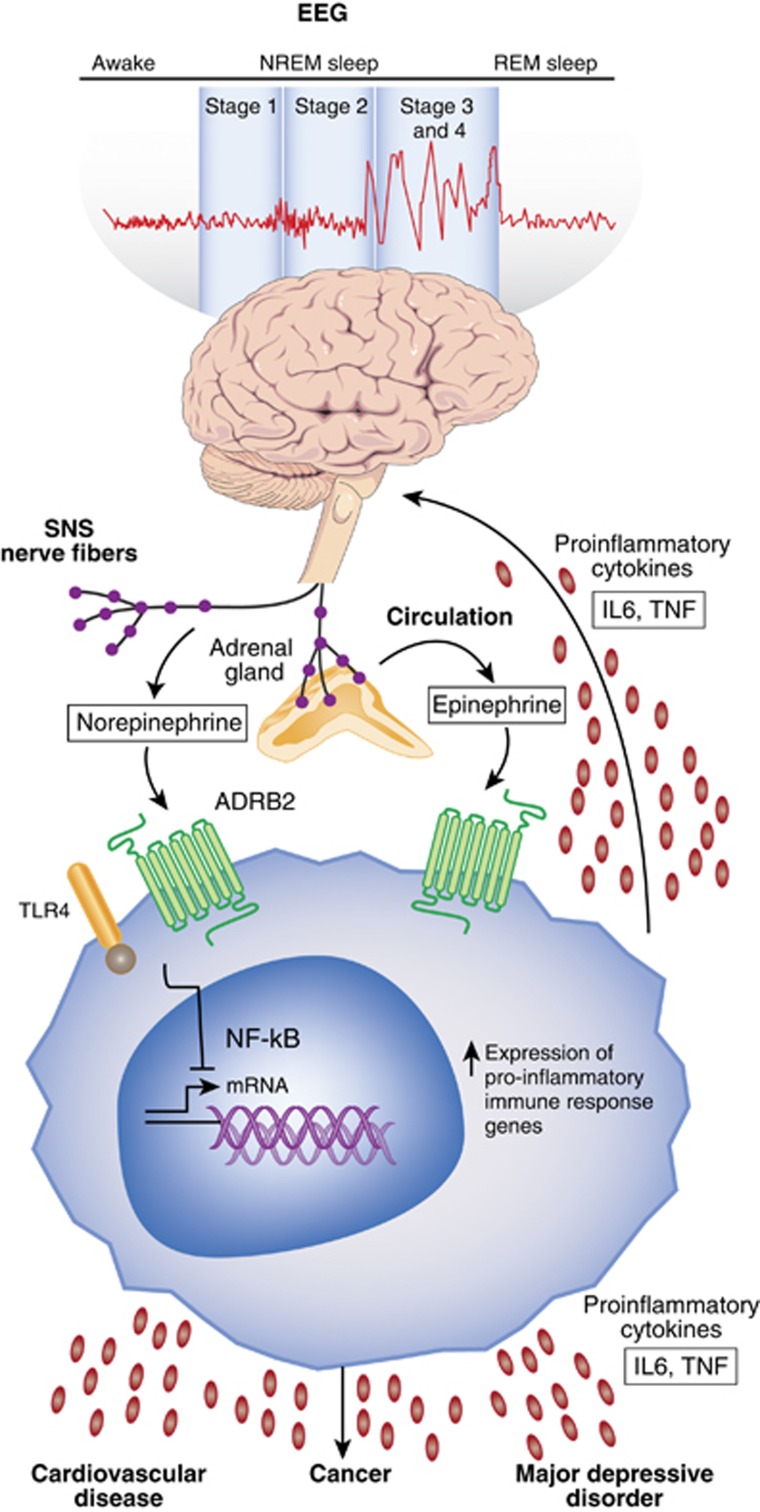
Figure 1.
Sleep disturbance and innate immunity. Following a night of sleep loss, or during a period of sleep disturbance, nerve fibers from the SNS release the neurotransmitter norepinephrine into primary and secondary lymphoid organs and stimulate the adrenal gland to release stored epinephrine into the systemic circulation. Both neuromediators stimulate leukocyte adrenergic receptors (eg, ADRB2) and activate nuclear factor (NF)-κB-mediated inflammatory programs. Intrinsic circuits detect microbes via pattern recognition receptors (PRRs) such as the toll-like receptor 4 (TLR4) and stimulate inflammatory gene expression via transcription factors such as nuclear factor (NF)-κB. The production of proinflammatory cytokines interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α) occurs. Bidirectional links between the brain and periphery allow the brain to regulate inflammatory activity, and inflammatory activity in turn can influence neural processes in the brain and alter sleep. When this dynamic is induced by sustained sleep disturbance, a feed-forward dysregulation of sleep can occur, which may also confer activation of the conserved transcriptional response to adversity (CTRA). CTRA activation leads to increases in proinflammatory gene expression and increased risk for inflammation-related disorders such as cardiovascular disease, cancer, and major depressive disorder, and to decreases in antiviral gene expression and increased risk of infectious diseases.