Abstract
Introduction:
South African men are less likely to get tested for HIV than women and are more likely to commence antiretroviral treatment (ART) at later stages of disease, default on treatment, and to die from AIDS compared with women. The purpose of this study was to conduct formative research into the ideational and behavioral factors that enable or create obstacles to mens' uptake of HIV counseling and testing (HCT) and ART. The study consulted men with a goal of developing a communication campaign aimed at improving the uptake of HIV testing and ART initiation among men.
Methods:
Eleven focus groups and 9 in-depth interviews were conducted with 97 male participants in 6 priority districts in 4 South African provinces in rural, peri-urban, and urban localities.
Results:
Fears of compromised masculine pride and reputation, potential community rejection, and fear of loss of emotional control (“the stress of knowing”) dominated men's rationales for avoiding HIV testing and treatment initiation.
Conclusions:
A communication campaign was developed based on the findings. Creative treatments aimed at redefining a ‘strong’ man as someone who faces his fears and knows his HIV status. The resultant campaign concept was: “positive or negative—you are still the same person.”
Key Words: HIV counseling and testing, antiretroviral therapy, men, uptake, adherence, communication, fear, stigma
INTRODUCTION
Compared with women, South African men have significantly lower levels of uptake of HIV counseling and testing (HCT) and antiretroviral treatment (ART) initiation and adherence.
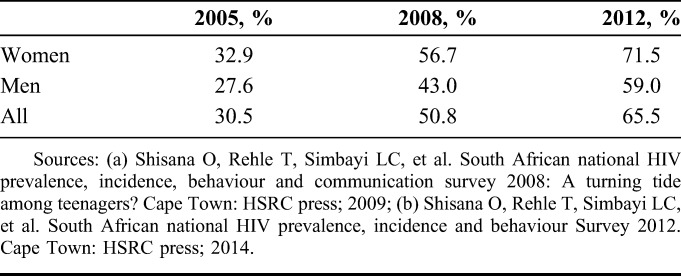
Overall rates of South African men and women 15 years and older having ever tested for HIV increased by 20.3% from 2005 to 2008 (Table 1). There was an overall increase of 14.7% from 2008 to 2012, partially attributed to the South African Government's national HCT campaign, initiated in 2010.1 In these national surveys, women reported ever being tested at a significantly higher level than men. A national survey in 2013 indicated an unchanged HCT rate, with 65% of the respondents reporting they had ever tested for HIV; persons who had higher exposure to health communication programs were more likely to have discussed HCT with their partners and those who discussed HIV testing were 3.5 times more likely to test.2
TABLE 1.
Percentage of the South African Population 15 Years and Older Ever Tested for HIV 2005–2012
The higher HCT rates for women, compared to men, are attributed to 3 diverse factors: (1) The effect of the national prevention of mother-to-child HIV transmission (PMTCT) program that includes HIV testing as part of routine prenatal appointments3; (2) Men's work-related mobility, lower perceptions of HIV risk compared with women, fear of stigma, and rejection by communities because of being seen standing in queues at health centers, lack of trust in health workers (especially lack of confidentiality), and perceptions of demasculization by being attended to by female health workers4–6; and (3) The anticipated psychological burden of living with HIV, including inability to cope with an HIV positive result, an associated lack of will to live, perceptions that an HIV-positive status hastens death, and that HCT results in being perceived by others as having been sexually promiscuous.6
Men are proportionately under-represented in ART initiation and successful treatment outcomes: Although approximately 55% of all people living with HIV in South Africa are female, more than 66% of those seeking ART at public facilities are female,3 and a significantly greater proportion of females living with HIV of all ages have been initiated on ART (34.7%), compared with males (25.7%).6 Furthermore, men living with HIV are 33% less likely than women living with HIV to start ART within 1 year of qualifying for ART and are 30% more likely to die within 1 year after ART initiation.7 Men are more likely to access ART at a later disease stage and are 1.47 times more likely to die on ART than women, even when disease stage is adjusted for.8
Reasons for lower attendance by men at public health care facilities for HCT or ART include these facilities' focus on family planning and pregnancy, reinforcing a perception that they are “women's places” because of the preponderance of female patients, nurses, and counsellors.9,10 Consequently, according to the Human Sciences Research Council (HSRC), addressing men's fears of testing and treatment is an issue of major concern.3,11
Social and community network norms (eg, views on manhood, culture, HIV stigma, perceptions of treatments, and other belief systems) influence men's health-seeking behavior (such as accessing ART) in a number of ways, including how men make decisions about whether or not to seek help, where, and from whom. For example, where masculinity is framed as being strong and not needing help, and where cultural beliefs associate weakness with illness, men are less likely to seek help at health facilities.12
Stigma around HIV threatens masculine notions of respectability, independence and emotional control and can prevent men from admitting illness and making use of health services. The experience of being sick and taking treatment forces men to redefine their sense of identity and masculinity.13 Communication programs that encourage people to discuss HIV-related issues create an enabling environment for long-term behavior change.14,15
Brothers for Life (B4L) is a South African national campaign seeking to influence social norms that define masculinity and gender norms, knowledge and practice in HIV prevention and treatment, medical male circumcision (MMC), and sexual and gender-based violence. B4L integrates epidemiological data, formative research, pretesting of materials, and postbroadcast evaluations conducted with target audiences as a model of practice.
The purpose of the current study was to provide evidence-based data to inform the design of a national B4L campaign to promote HCT in men, to encourage men living with HIV to seek early ART and adhere to ART, and to support the attainment of UNAIDS's 90-90-90 targets.16 The focus was identifying men's underlying social, interpersonal, and personal beliefs and attitudes toward HCT and ART. This study formed part of a larger study that included both women and men. This report focuses solely upon findings reported by men.
METHODS
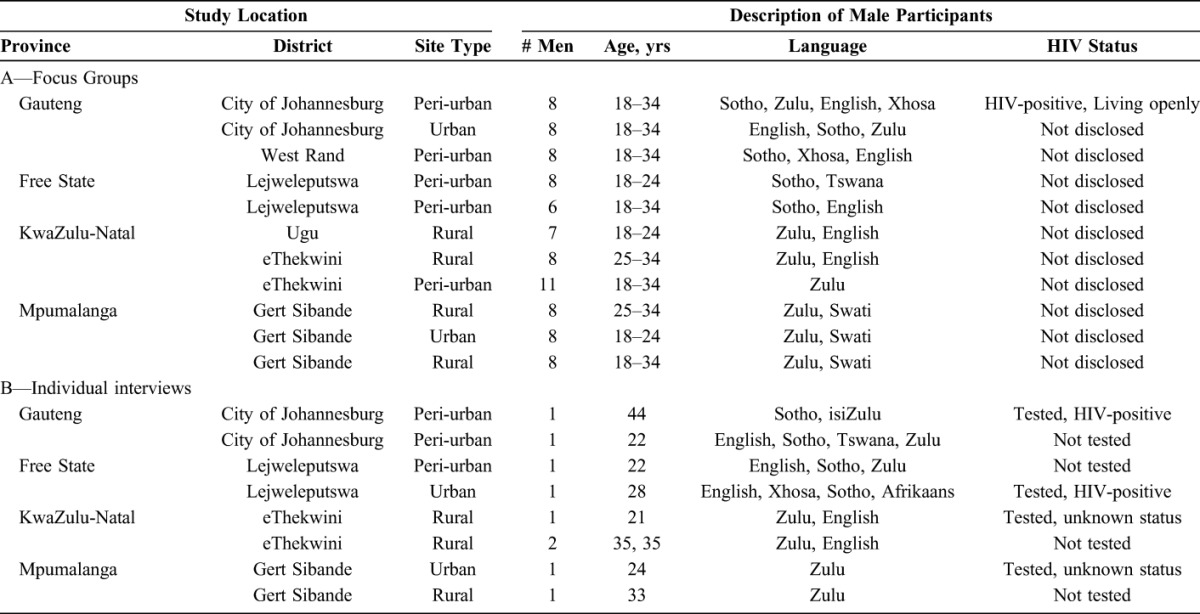
Eleven focus groups (n = 88 males aged 18–35 years) and 9 individual interviews (n = 9 males aged 21–44 years) were conducted in urban, peri-urban, and rural sites in 6 districts across 4 South African provinces (Table 2). The study sites correspond to “priority” districts identified by the South African government given their high HIV prevalence rates and for having highly mobile and migrant worker populations.
TABLE 2.
Study Locations and Participant Description
Criteria for recruitment of focus group participants and interviewees were that participants represented the target audience for the intended communication campaign: males aged 18–35 years (primary target audience) and males 35 years or older (secondary target audience) from urban, peri-urban, and rural localities; willingness to talk openly about the areas of study; provided informed consent for the study and for audio recording of discussions, and the use of data in a way that protected their identity. Ethical clearance was obtained from the Human Sciences Research Council.
Of the 97 men participating, 10 (8 in one focus group and 2 in individual interviews) were HIV positive and living openly. They were recruited to explore their views about barriers to HCT and ART. In each province, one man was interviewed who had tested for HIV, and one who had never tested for HIV. Interviews allowed for in-depth discussion of personal experiences and motivations. Focus group discussions and interviews occurred in the preferred language of participants (isiZulu, Sesotho, SiSwati, English), with translation when needed.
Focus group and interview discussion guides incorporated open-ended questions focused upon barriers and enablers of men's behaviors and attitudes regarding accessing HCT and ART in public health centers, with scope for in-depth probing. Focus groups and interviews were audio-recorded, translated, and transcribed verbatim. Transcripts were read and discussed by all fieldwork researchers to develop a thematic coding framework. Findings were coded by the researchers according to the developed thematic framework, using NVivo8, a software program for qualitative analysis. Researchers remained open to themes emerging from the data, developing additional codes rather than forcing data into existing codes. This allowed for previously unidentified codes and themes to emerge.
RESULTS
Key findings regarding barriers to HCT and ART as reported by male participants across field sites are presented. Quoted statements made by specific men serve as typical examples of statements made by participants across all locations.
All study participants knew where to get tested or treated for HIV.
Across study sites, public sector clinics were broadly perceived as being women's spaces. Commonly, men said they felt self-conscious and uncomfortable at public clinics because it was unusual to find young men there for reasons other than HIV, and other people would assume any man at the clinic would be HIV positive. Negative participant experiences at public sector clinics included being shouted at and judged by health professionals and confidentiality violations. This resulted in the avoidance of public clinics for HCT and ART, and participants seeking health services in other communities and in private health care, where anonymity was more likely.
Masculine identity was closely associated with the pride of appearing as strong, with fear associated with being viewed as weak by others: “We were raised with the mentality that a man … is this strong person so when people see a weakness I will be afraid because I won’t be seen as a man and I will be called a woman… Other men will say you are a woman and must wear panties” (rural male, 25–35 years, Gert Sibande, Mpumalanga).
Men placed great emphasis upon what people think about them—their “pride” and “status”—and were concerned about being perceived as weak when seeking services at clinics—“men in our age group have a sense of pride… when he is seen going to the clinic to receive medication, he will be viewed differently. So men …. will never go to a clinic” (urban male, 18–24 years, Gert Sibande, Mpumalanga).
Most men regarded illness as synonymous with weakness. The impact of “pride” on men's health-seeking behavior ranged from refusing to wear eye glasses when with friends, to avoiding HCT, to reluctance to admitting being ill, and to avoiding medical treatment until seriously ill. “Nobody fears being sick (more) than a male person, we are more terrified of being sick than our female counterparts. So if I have to take medication, it's the same as giving in” (admitting illness) (urban male, 18–24 years, Gert Sibande, Mpumalanga).
Men's fears regarding HCT and ART were expressed in strong terms, such as “terrified,” “paranoid,” and “very scared.” Many of these fears were directly related to perceived threats to masculine identity norms, such as the fear of needing to change their lifestyle as a result of an HIV-positive test result, the reputational risk of being seen at a clinic by other community members, and the fear of being gossiped about and being rejected by peers, partners, and family. These potential experiences were described as “being exposed” and having one's “reputation destroyed.”
For some men, HCT was construed as a loss of dignity and inconsistent with normative masculine norms: “if you go to test as a man, you think you have lost your dignity…and other people…. will laugh at me, people will be talking about me” (peri-urban male, 18–34 years, West Rand, Gauteng).
Several men expressed reticence regarding being friends with someone who is HIV positive because they feared others would assume they were also infected saying “both of us are dying”; “friends of a criminal.” They also thought it would be awkward to stay friends because they could not joke around with someone who is HIV positive, and that person would be “side-lined.”
Secrecy regarding taking ART was said to be necessary because of other people's beliefs that the need to take ART reflected prior unsafe sexual behaviors, which in turn implied that their current sexual partners were at risk of acquiring HIV: “We are embarrassed, we think that other people are going to say I am loose that is why I am taking them (ART), I am dirty or naughty so you are useless and that means you don't condomise” (rural male, 18–34 years, Gert Sibande, Mpumalanga).
Men said they were more likely to test after having what they regarded as risky sex (unprotected sex, sex with multiple partners) if they heard a rumor that a previous partner is HIV positive, or suspected their partner or ex-partner had “cheated.” Some men said they would test if they found out their current or previous partner was HIV positive. Several men said they either had tested or would do so if they had unsafe sex with someone they regarded as “questionable” (eg, sex worker, someone met at a local tavern) or if the condom broke.
A few participants thought that men would be more likely to test when they feel they have nothing to worry about, as a result of having few if any potential opportunities for HIV exposure. Men who test were described as “fine” or “relatively good.”
Alcohol was commonly cited as an important reason for men to avoid initiating ART because ART was viewed as a barrier to continuing to drink at will. Many men who receive ART used alcohol to deal with their HIV status: “Instead of taking the meds… if he was a heavy drinker—then they start drinking more than before” (urban male, 18–24 years, Gert Sibande, Mpumalanga).
A recurrent theme was that it was better not to know your HIV status and to wait until you are ill before seeking help, because “a person is killed by the stress of knowing.”
The most common reason provided by men for testing and seeking treatment was experiencing a persistent health problem: “It is unusual for one to just go and get tested, they are prompted by something” (urban male, 24 years, HIV-positive, Gert Sibande, Mpumalanga). Most HIV-positive men interviewed only tested after developing a health problem.
There were several reports of men stopping ART after experiencing improved health and because they were unwilling take treatment indefinitely. Some men stated that traditional healing practices influence late initiation of ART and nonadherence because traditional medicine is taken when one is ill, and stopped when one is cured. Several men reported having experienced male family or friends commencing ART at late stages of HIV disease and dying shortly thereafter.
Commonly cited factors that reduced fears of HCT and possible treatment were exposure to training about HIV and AIDS, knowing someone living with HIV, partner requests to get tested, and advice and support from trusted friends.
Commonly, men said that fear-based messaging was ineffective in increasing their willingness to test and treat because fear-based messaging increased stigma and fear through the use of “blood—red colours,” “black ninjas—goggas (insects),” and “posters of sick people.” They stated a preference for advertisements that are humorous because these facilitate interpersonal discussions.
DISCUSSION
This study focused on identifying self-reported cross-regional behaviors, attitudes, and beliefs of South African men in 4 provinces regarding HCT and ART that were amenable to a national communication campaign. The results reiterated findings from other studies4–8 concerning the fears men have in accessing public health services for HCT and ART, linked to concepts of masculine pride, strength, respectability, maintaining a reputation as a “real man,” and concerns regarding being perceived as having engaged in unsafe sexual practices and exposing sexual partners to HIV. Most participants expressed fears of stigma and rejection by the community if seen attending public health centers, suggesting that one area of increasing male uptake for HCT and ART would be providing male-friendly17 or male-only18 service delivery structures.
The influence of traditional healing protocols19–21 was apparent in several statements concerning stopping ART once health was restored, resulting in relapse and, in several reported cases, death. This phenomenon suggests that education of men and traditional health practitioners regarding chronic—versus curative—treatment is required.
This study also confirmed previous studies8,12,13 that many men delay HCT and commencing ART until compelled to do so because of persistent health problems, and that some men feared the loss of emotional control that they expected to occur as a result of knowing their HIV status. This anticipated loss of emotional control—often expressed as a feared need to change lifestyle once diagnosed with HIV—was of sufficient magnitude for many participants to prevent them from getting tested for HIV.
The “fear of knowing” was considered by the authors to be a core concern for most men who were reluctant to get tested, and most amenable to a communication campaign. Consequently, a national communication campaign was developed to promote HCT and ART (if needed) among men. The campaign used a creative treatment focusing on the central concept of fear of change after an HIV test. Two public service advertisements—a man testing HIV negative and a man testing HIV positive—were developed. The style of the narrative is humorous, with a man's fears externalized by rapid changes in his physical surroundings (friends, family, clothes, furniture, and other objects) after the test result, followed by an equally rapid reversal of these changes. The slogan is “Positive or Negative, you are still the same person.” The message of the advertisement concludes that, other than the use of condoms (for those tested HIV-negative), and condoms and ART (for those tested HIV-positive), “nothing much changes” after a test result. The desired impact is to allay men's fears of lifestyle and identity changes post-diagnosis through highlighting that fears are not based in reality.
The attainment of the UNAIDS's 90-90-90 targets16 will require policy and programmatic attention to identified barriers that inhibit South African men's willingness and ability to get tested for HIV, and—where necessary—commence ART. One remedial component would include evidence-based social media campaigns to address the identified beliefs and fears of men concerning these services.
Footnotes
CADRE is currently a subrecipient of the Centre for Communication Impact NPC. The subagreement is funded by the United States Agency for International Development under Cooperative Agreement No. AIDS-674-A-14-00008.
The authors have no conflicts of interests to disclose.
REFERENCES
- 1.South African National Department of Health. Joint Review of HIV, TB and PMTCT Programmes in South Africa: Main Report. Pretoria, South Africa: National Department of Health; 2014. [Google Scholar]
- 2.Johnson S, Kincaid DL, Figueroa ME, et al. The Third National HIV Communication Survey, 2012. Pretoria, South Africa: Johns Hopkins Health and Education South Africa (JHHESA); 2013. [Google Scholar]
- 3.Shisana O, Rehle T, Simbayi LC, et al. South African National HIV Prevalence , Incidence and Behaviour Survey 2012 Cape Town, South Africa: HSRC Press; 2014. [Google Scholar]
- 4.Radingwana TM. Factors Encouraging or Discouraging Men in the Informal Sector to Attend HIV Counselling and Testing (HCT) in South Africa: A Case Study of Pretoria. Pretoria, South Africa: University of South Africa; Available at: http://sciences588.rssing.com, Article 361, 2014. [Google Scholar]
- 5.Mills EJ, Beyrer C, Birungi J, et al. Engaging men in prevention and care for HIV/AIDS in Africa. PLoS Med. 2012;9:e1001167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Musheke M, Ntalasha H, Gari S, et al. A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in Sub-Saharan Africa. BMC Public Health. 2013;13:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ingle SM, May M, Uebel K, et al. Differences in access and patient outcomes across antiretroviral treatment clinics in the Free State province: a prospective cohort study. S Afr Med J. 2010;100:675–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.May M, Boulle B, Phiri S, et al. Prognosis of HIV-1 infected patients starting antiretroviral therapy in sub-Saharan Africa: a collaborative analysis of scaleup programmes. Lancet. 2010;376:449–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cornell M, McIntyre J, Myer L. Men and antiretroviral therapy in Africa: our blind spot. Trop Med Int Health. 2011;16:828–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Myburgh H. The clinic as a gendered space: masculinities, health seeking behaviour and HIV & AIDS. Consultancy Africa Intelligence HIV and AIDS Unit. 2011;1–5. [Google Scholar]
- 11.Babalola S, Van Lith LM, Mallalieu EC, et al. A framework for health communication across the HIV treatment continuum. J Acquir Immune Defic Syndr. 2017;74(suppl 1):S5–S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mfecane S. Exploring Masculinities in the Context of ARV Use: A Study of Men Living With HIV in a South African village. [Unpublished Ph.D. thesis] Johannesburg, South Africa: University of Witwatersrand; 2010. [Google Scholar]
- 13.Mburu G, Ram M, Siu G, et al. Intersectionality of HIV stigma and masculinity in eastern Uganda: implications for involving men in HIV programmes. BMC Public Health. 2014;14:1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Do M, Figueroa ME, Lawrence-Kincaid D. HIV testing among young people aged 16-24 in South Africa: impact of mass media communication programs. AIDS Behav. 2016;29:2033–2044. [DOI] [PubMed] [Google Scholar]
- 15.Audet CM, Blevins M, Chire YM, et al. Engagement of men in antenatal care services: increased HIV testing and treatment uptake in a community participatory action program in Mozambique. AIDS Behav. 2016;20:2090–2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.UNAIDS. 90-90-90:An Ambitious Treatment Target to Help End the AIDS Epidemic. Geneva, Switzerland: Joint United National Programme on HIV/AIDS (UNAIDS); 2014. [Google Scholar]
- 17.Betron M. Men engage partners visit a male-friendly health clinic in Tanzania. 2016. Available at: http://menengage.org. Accessed September 21, 2016.
- 18.Green A. Man to man, sexual health needs are better met at male-only clinics. 2015. Available at: http://bhekisisa.org. Accessed September 21, 2016.
- 19.Audet CM, Blevins M, Moon TD, et al. HIV/AIDS-related attitudes and practices among traditional healers in Zambezi Province, Mozambique. J Altern Complement Med. 2012;18:12: 1133–1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peltzer K, Mngqundaniso N, Petros G. HIV/AIDS/STI/TB knowledge, attitudes and practices among lay health workers and nurses in KwaZulu-Natal, South Africa. Africa J Nurs Midwifery. 2005;7:17–34. [Google Scholar]
- 21.Walwyn D, Maitshotlo B. The role of South African traditional health practitioners in the treatment of HIV/AIDS: a study of their practices and use of herbal medicines. South Afr J HIV Med. 2010;11:11–17. [Google Scholar]


