Introduction
Metformin is an oral antidiabetic drug used for treatment of Type 2 diabetes mellitus (T2DM).[1] It acts by decreasing gluconeogenesis in the liver and absorption of glucose from the gastrointestinal system, in addition to increasing the peripheral utilization of glucose.[02] Metformin is excreted unchanged through the renal route. Severe side effects are noted in patients with renal and/or hepatic dysfunction. These may vary from severe lactic acidosis which can be life threatening, to cardiac arrhythmias.[03]
We present a case of a patient who presented with recurrent atrial fibrillation with repeated administration of metformin. He developed lactic acidosis in the absence of renal or hepatic dysfunction and developed the arrhythmia, which promptly resolved metformin withdrawal.
Presentation
A 68-year-old patient was seen in our clinic for atrial fibrillation (AF). His past medical history was pertinent for hypertension, T2DM, anxiety disorder, coronary heart disease and hyperlipidemia. Past surgical history was positive for coronary artery by-pass graft (CABG). Current medications include lisinopril, atorvastatin, glimipride, sitagliptin, metoprolol, and warfarin.
At presentation, his BP was 120/74 mmgHg, Heart Rate 61 beats/min, and respiratory rate was 14 breaths/min. His physical examination was unremarkable. An electrocardiogram revealed a normal sinus rhythm (NSR). The patient had a comprehensive metabolic panel which was essentially within normal limits ([Table 1]).
Table 1. Laboratory Values.
| Labs | Pre Metformin | During Metformin | After stopping metformin |
|---|---|---|---|
| Na mmol/L | 138 | 140 | 139 |
| K mmol/L | 4.1 | 4 | 3.9 |
| Cr mg/dL | 0.9 | 1 | 1 |
| BUN mg/dL | 24 | 30 | 32 |
| Gluc mg/dL | 120 | 118 | 124 |
| Chloride mmol/L | 105 | 106 | 102 |
| CO2 mmol/L | 24 | 24 | 25 |
| LDH mcmol/L | 220 | 320 | 184 |
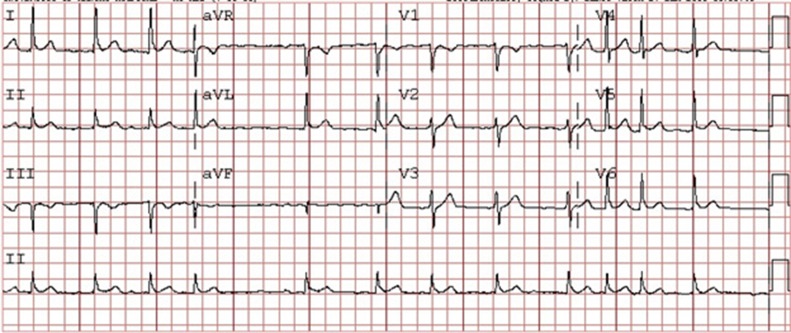
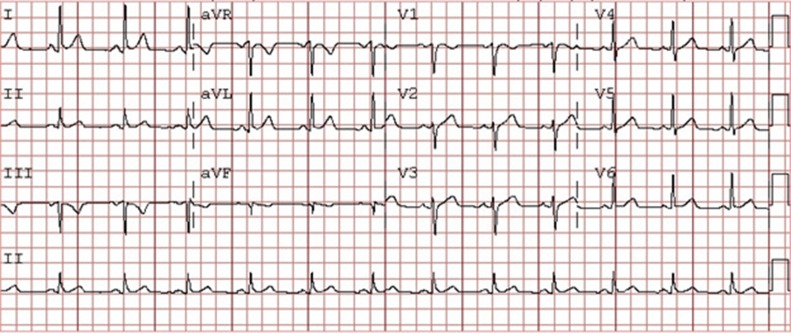
On his follow-up visit to his primary physician, his sitaglipitin was discontinued and metformin was initiated. After being on it for approximately seventy two hours, the patient reported irregular heartbeats and presented to the emergency room. He was noted to be in atrial fibrillation at the time. The patient reported a similar episode in the past when he was on metformin, which resolved when he discontinued the medication. During this episode, the patient was treated for atrial fibrillation and the metformin was stopped. The patient converted to NSR upon discontinuation of the medication after 48 hours. After the rhythm was normalized, he was rechallenged with metformin. After approximately 48 hours, he developed AF ([Figure 1]). Again, after withdrawal of metformin, the rhythm reverted to NSR ([Figure 2]).
Figure 1. ECG of the patient in atrial fibrillation on metformin.
Figure 2. ECG of the patient when converted to sinus rhythm after with-holding metformin.
Discussion
This present case illustrates how metformin induced AF each time after repeated challenges to the patient. On lab data analysis, the renal and hepatic indices were within normal limits. Interestingly, the bicarbonate level was noted to be lower when challenged with metformin, and lactate levels were higher during the challenge. This suggested the patient had problems metabolizing metformin despite normal hepatic and renal function and developedlactic acidosis during metformin administration, which might have led to the initiation of AF.
Metformin has been used as a first line agent for treatment of diabetes mellitus along with lifestyle changes.[04] It is not uncommon to see renal or hepatic dysfunction in patients with diabetes, and this dysfunction may lead to more incidents of lactic acidosis. Lactic acidosis associated with metformin has been linked to various side effects, including cardiac arrhythmias.[03,05] Studies on animal models have shown that metformin can cause greater dispersion of the QT interval at higher concentrations and could be responsible for arrhythmogenesis.[06] This is the first reported human case of AF related to metformin use. We hypothesize that lactic acidosis related to metformin use could have potentially set the AF triggers in motion and have resulted in substrate changes that perpetuated the arrhythmia.
Conclusions
Our patient showed recurrence of atrial fibrillation when re-challenged with the same medication and resolution on withdrawal of the same medication. Lactic acidosis is amongst the most rare but significant side effects of metformin and the acidic milieu as a result of lactic acidosis could make the heart, particularly the atria more prone to arrhythmias.
References
- 1.Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998 Sep 12;352 (9131):854–65. [PubMed] [Google Scholar]
- 2.Kirpichnikov Dmitri, McFarlane Samy I, Sowers James R. Metformin: an update. Ann. Intern. Med. 2002 Jul 02;137 (1):25–33. doi: 10.7326/0003-4819-137-1-200207020-00009. [DOI] [PubMed] [Google Scholar]
- 3.Chang Chin-Tung, Chen Yung-Chang, Fang Ji-Tseng, Huang Chiu-Ching. Metformin-associated lactic acidosis: case reports and literature review. J. Nephrol. 2002 Sep 24;15 (4):398–402. [PubMed] [Google Scholar]
- 4.Nathan David M, Buse John B, Davidson Mayer B, Ferrannini Ele, Holman Rury R, Sherwin Robert, Zinman Bernard. Management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: update regarding thiazolidinediones: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2008 Jan;31 (1):173–5. doi: 10.2337/dc08-9016. [DOI] [PubMed] [Google Scholar]
- 5.Heaney D, Majid A, Junor B. Bicarbonate haemodialysis as a treatment of metformin overdose. Nephrol. Dial. Transplant. 1997 May;12 (5):1046–7. doi: 10.1093/ndt/12.5.1046. [DOI] [PubMed] [Google Scholar]
- 6.Costa Eunice Cristina da Silva, Gonçalves Antonio Ari, Areas Miguel Arcanjo, Morgabel Rafael Gustavo Birochi. Effects of metformin on QT and QTc interval dispersion of diabetic rats. Arq. Bras. Cardiol. 2008 Apr;90 (4):232–8. doi: 10.1590/s0066-782x2008000400004. [DOI] [PubMed] [Google Scholar]