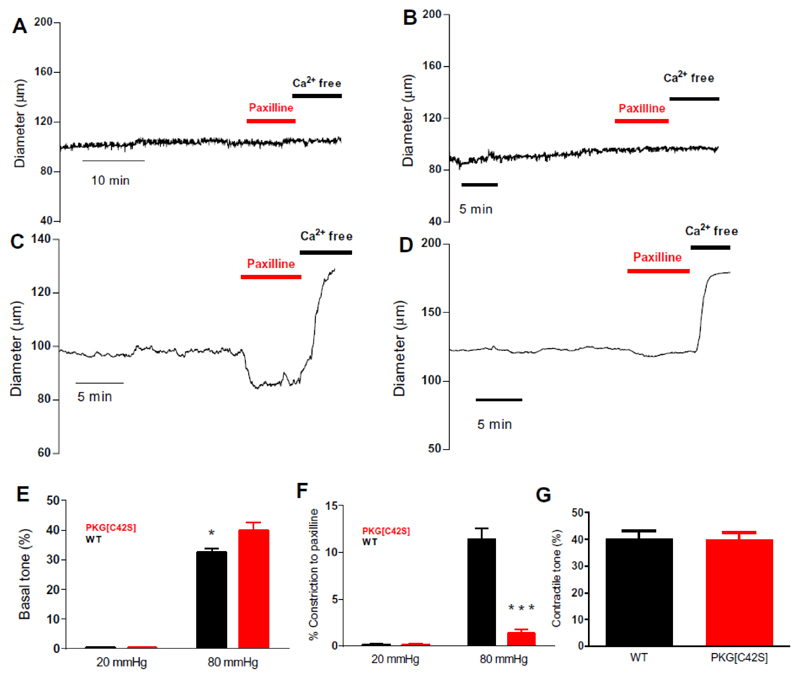
Figure 1. Intravascular pressure activates oxidizable PKG, which engages BK channels to oppose tone development.
A and B: Representative diameter traces from WT (A) and PKG[C42S]KI (B) mesenteric arteries pressurized to 20 mmHg. C and D: Representative diameter trace from WT (C) and PKG[C42S]KI (D) mesenteric arteries pressurized to 80 mmHg. E: Pressure-induced constriction in PKG[C42S]KI and WT arteries measured at 20 and 80 mmHg. Percent constriction of PKG[C42S]KI arteries (39.8% ± 2.5%, n = 20 arteries from 12 mice) was significantly greater than WT arteries (32.4% ± 1.2%, n = 27 arteries from 19 mice) at 80 mmHg intraluminal pressure. P=0.014, Mann-Whitney U test. Absolute active diameters: WT: 108.4 ± 3.3μm; PKG[C42S]KI: 99.8 ± 6.7μm. Absolute passive diameters: WT: 161.1 ± 4.7μm; PKG[C42S]KI: 161.2 ± 5.9μm. F: Response to paxilline in PKG[C42S]KI and WT arteries measured at 20 and 80 mmHg. Percent constriction (relative to passive diameter) in response to paxilline in WT arteries (11.4% ± 1.8%, n = 6 arteries from 6 mice) was significantly greater than in PKG[C42S]KI arteries (1.3% ± 0.6%, n = 5 arteries from 5 mice) at 80 mmHg intraluminal pressure. P = 0.002, unpaired t-test. G: Degree of pressure-induced constriction in untreated arteries from PKG[C42S]KI mice (39.8% ± 2.5%, n = 20 arteries from 12 mice) was not significantly different from that in paxilline (Pax)-treated arteries from WT mice (40.1% ± 3%, n = 6 arteries from 6 mice).