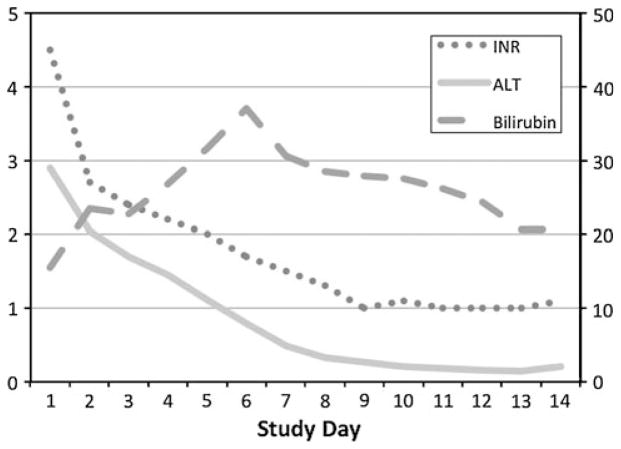
Fig. 2.
A patient with ALF due to hepatic ischemia from an unrecognized cardiomyopathy. A 24-year-old previously healthy Caucasian male presented with a two-week history of unexplained nausea, vomiting, abdominal pain, and jaundice. At admission, his serum AST was 2,962 IU/l, ALT 2,902 IU/l, total bilirubin 15 mg/dl, and INR 4.5. In addition, he had acute kidney injury with a serum creatinine of 4.4 mg/dl and a phosphate level of 6.6 mg/dl. Evaluation for hepatitis A, B, and C, autoimmune hepatitis, and toxic liver injury was negative and a liver ultrasound demonstrated no biliary tract disease. At enrollment, he had grade 2 encephalopathy and was started on renal replacement therapy on hospital day 2. A surface echocardiogram revealed severe biventricular heart failure with an ejection fraction of <10%. Because of hypotension refractory to inotropes, an aortic balloon pump was placed on hospital day #4 followed by a left ventricular assist device on day #5 and his liver and kidney function gradually improved over the following month. At discharge on hospital day #68, his ALT was 74 IU/l and bilirubin 2.1 mg/dl. Eventually he underwent heart transplantation and his explant revealed evidence of a diffuse idiopathic cardiomyopathy. The patient is currently alive and well nine years after presentation with normal cardiac and hepatic function. (Serum ALT reported in units of 1,000 IU/l)