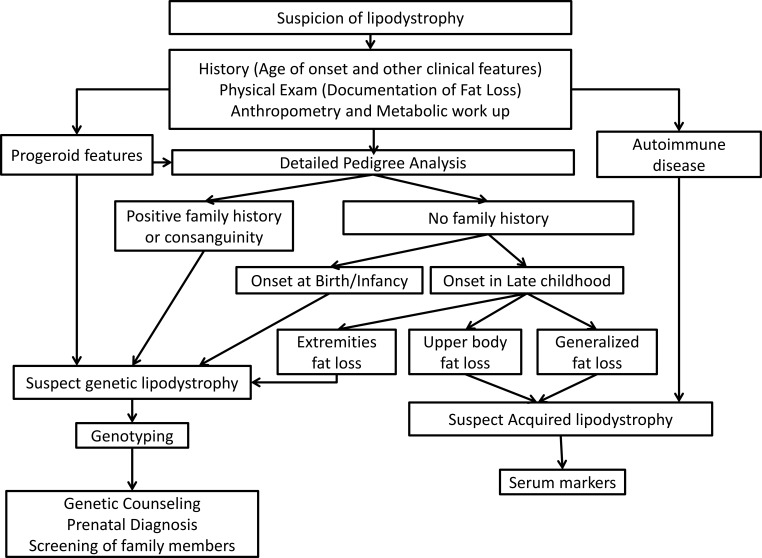
Figure 2.
Diagnostic approach to lipodystrophy syndromes. Lipodystrophy should be suspected in patients with regional or generalized lack of adipose tissue. History should assess age of onset of fat loss and comorbidities. Physical examination should determine distribution of sc fat loss and presence of prominent muscles, phlebomegaly, acanthosis nigricans, hepatomegaly, xanthomas, and acromegaloid or progeroid appearance. All patients should undergo a metabolic workup for insulin resistance, diabetes, dyslipidemia, and fatty liver disease. Conventional anthropometry including skinfold thickness measurements, ± dual energy x-ray absorptiometry, and whole-body magnetic resonance imaging (if available) should be performed to confirm the pattern of fat loss. Common genetic lipodystrophies include CGL, FPLD, and progeroid lipodystrophies. They require genotyping to confirm the diagnosis, followed by genetic counseling and screening of family members. Patients with progeroid lipodystrophies have progeroid features like bird-like facies, high-pitched voice, skin atrophy and pigmentation, alopecia, and nail dysplasia. Patients with FPLD have fat loss of the extremities typically occurring around puberty and can have a positive family history. Patients with CGL have near-complete lack of fat starting at birth or infancy. Acquired lipodystrophies have fat loss typically in late childhood. Patients with AGL have generalized loss of sc fat and often have associated autoimmune diseases. Patients with APL have cranio-caudal fat loss affecting the face, neck, shoulders, arms, and upper trunk, and most patients have low serum C3 levels.