Abstract
Technological advancements in past decades have led to the development of integrative analytical approaches to lipidomics, such as liquid chromatography-mass spectrometry (LC/MS), and information about biogenic lipids is rapidly accumulating. Although several cohort-based studies have been conducted on the composition of urinary lipidome, the data on urinary lipids cross-classified by sex, age, and body mass index (BMI) are insufficient to screen for various abnormalities. To promote the development of urinary lipid metabolome-based diagnostic assay, we analyzed 60 urine samples from healthy white adults (young (c.a., 30 years) and old (c.a., 60 years) men/women) using LC/MS. Women had a higher urinary concentration of omega-3 12-lipoxygenase (LOX)-generated oxylipins with anti-inflammatory activity compared to men. In addition, young women showed increased abundance of poly-unsaturated fatty acids (PUFAs) and cytochrome P450 (P450)-produced oxylipins with anti-hypertensive activity compared with young men, whereas elderly women exhibited higher concentration of 5-LOX-generated anti-inflammatory oxylipins than elderly men. There were no significant differences in urinary oxylipin levels between young and old subjects or between subjects with low and high BMI. Our findings suggest that sex, but neither ages nor BMI could be a confounding factor for measuring the composition of urinary lipid metabolites in the healthy population. The information showed contribute to the development of reliable biomarker findings from urine.
Introduction
Metabolomics is a relatively recent research area focused on the systemic profiling of small-molecule metabolites. Lipidomics is a lipid-targeting subarea of metabolomics that involves comprehensive analyses of pathways and interactions of cellular lipids in biological systems. Recent technological developments in mass spectrometry (MS) and chromatography have considerably advanced the application of lipid metabolic profiling in complex biological samples [1]. Because the structure of lipid molecules, in contrast to that of genome-encoded proteins, cannot be studied via direct manipulation of the respective genes, lipidomics is now considered to be one of the most important and rapidly developing research areas.
Owing to their considerable structural diversity, lipids are important players in a variety of complex physiological processes, where they execute important functions, acting as cellular membrane components, signaling mediators, energy reserve molecules, and endocrine regulators [2–4]. The so-called lipid mediators are a group of regulatory molecules produced in response to extracellular stimuli that bind to their cognate receptors and transmit signals to target cells; their deregulation has been linked to various pathological conditions such as inflammation, atherosclerosis, and diabetes [5–7]. Lipid mediators include polyunsaturated fatty acids (PUFAs), lysophosphatidic acid, and their derivatives. It is believed that many regulatory activities of PUFAs are mediated by their oxidation products, oxylipins [8], which are produced and activated by several enzymes such as cytochrome P450 (P450), cyclooxygenases (COX), and lipoxygenases (LOX). Oxylipins have been mostly associated with the initiation and resolution of inflammation and vascular function. The kidneys have the highest levels of P450, COX, and LOX enzymes after the liver; these enzymatic pathways play a pivotal role in kidney function and renal disease [9–11]. The kidneys are essential to the urinary system and also play a role in systemic homeostasis. As urine production is regulated by oxylipins produced by the three major oxygenases, which respond to systemic conditions, the urinary oxylipin profile may reflect renal enzymatic activity as well as systemic status [12].
As an important and easily accessible biological fluid, urine has been the subject of detailed chemical analyses for more than 100 years. Even today, urine analysis is routinely performed using dipstick tests that can readily measure urinary glucose, bilirubin, ketone bodies, nitrates, leukocyte esterase, specific gravity, hemoglobin, urobilinogen, and protein. More detailed urinalysis can be also used to study a variety of renal conditions, including bladder and kidney cancer [13, 14]. However, some problems remain to be solved in urinary lipid-based diagnostics. Until recently, gas chromatography coupled with MS was the primary lipid analysis used for low-molecular-weight and low-polarity molecules, which usually require chemical derivatization. Several disease- and/or drug- related metabolic abnormalities can be detected in urine; however, little information is available on the urinary lipid composition in healthy subjects on a regular diet, and the normal variation in urinary lipid content has not been determined, which restricts the diagnostic potential of lipid profiling in urine samples despite its clinical significance.
To overcome these obstacles, we have attempted to characterize the human urine metabolome in healthy subjects. In this study, we performed cross-classification of urinary lipids by sex, age, and body mass index (BMI) in a healthy population after normal overnight fasting using liquid chromatography coupled with MS (LC/MS).
Materials and Methods
Collection and preparation of human urine
Urine samples from healthy white adults were purchased from PromedDX (Norton, MA). The samples were collected after written informed consent was obtained from all subjects. These were collected using the blood donor history questionnaires prepared by the AABB to screen for disease risk factors [15]. Therefore, all of these subjects are considered as Normal Healthy donors outlined by AABB. The ethics committee of the National Institute of Health Sciences authorized PromedDX as a validated provider of urine samples and exempted us from the committee’s approval for use of the purchased urine samples. All subjects declared healthy at the recruitment, and their urine was collected the next morning after fasting for 14 h from 60 individuals divided into four groups (n = 15): young men (25–33 years old), elderly men (55–64 years old), young women (25–34 years old), and elderly women (55–63 years old) (Table 1 and S1 Table). Fresh urine from each individual was collected into 15-ml test tubes, immediately frozen, and stored at -80°C. The samples were shipped from PromedDX on dry ice, thawed on ice after arrival, divided into small aliquots, and stored at -80°C until lipid extraction. Together with urine, fresh blood was simultaneously collected from same individuals, and the metabolites profiles in their plasma and serum are already published in our previous paper [16, 17]. There are no outliers in their serum creatinine levels [17], a classical biomarker for kidney function, suggesting their renal functions are normal.
Table 1. Demographic characteristics of the study population.
| GROUP (number) | AGE±Std | BMI±Std |
|---|---|---|
| YOUNG MEN (n = 15) | 29.0±2.4 | 26.2±5.6 |
| ELDERLY MEN (n = 15) | 59.0±2.57 | 24.5±4.7 |
| MEN (n = 30) | 44.0±15.1 | 25.1±5.2 |
| YOUNG WOMEN (n = 15) | 28.0±3.3 | 35.4±8.8 |
| ELDERLY WOMEN (n = 15) | 59.0±2.3 | 32.7±4.5 |
| WOMEN (n = 30) | 44.5±15.6 | 33.5±7.3 |
| HIGH (>30) BMI male (n = 7) | 32.0±16.2 | 33.1±1.9 |
| HIGH (>30) BMI female (n = 21) | 34.0±15.1 | 36.1±6.1 |
| HIGH (>30) BMI (n = 28) | 55.0±15.15 | 34.0±15.4 |
| LOW (<30) BMI male (n = 23) | 55.0±14.7 | 23.0±3.2 |
| LOW (<30) BMI female (n = 9) | 57.5±16.0 | 27.5±1.4 |
| LOW (<30) BMI (n = 32) | 35.36±5.73 | 25.3±3.3 |
| TOTAL (n = 60) | 44.5±15.3 | 29.2±7.7 |
Urine samples were collected from 60 individuals divided in four groups: young men, elderly men, young women, and elderly women (n = 15 per group), and also stratified by BMI, high (> 30) and low (< 30). The data on age and BMI are presented as the median ±STD. BMI, body mass index.
Chemicals
Unless otherwise indicated, all reagents were of MS analytical grade. LC/MS grade methanol, acetonitrile, water, and chloroform were purchased from Wako Pure Chemical, Ltd. (Nihonbashi, Tokyo). 1,2-dipalmitoyl d6-3-sn glycerophosphatidylcholine (16:0/16:0 PC-d6) and 13C-labeled tripalmitin (tripalmitin-1,1,1-13C3) were purchased from Larodan Malmo (Solna, Sweden). Phospholipid, PUFA, and other oxylipin internal standards (ISs) were purchased from Cayman (Ann Arbor, MI).
Sample preparation for MS analysis
Urine (200 μl) was added to 1,300 μl of methanol containing ISs used for normalization and evaluation of extraction efficacy. The following ISs were utilized: 16:0/16:0 PC-d6 (33.3 μM), tripalmitin-1,1,1-13C3 (3.3 μM), deuterated PGE2-d4 (33 pg/μl), and deuterated LTB4-d4 (33 pg/μl). The samples were centrifuged at 15,000 rpm for 3 min at 4°C to precipitate insoluble matter, and 1,440 μl of the supernatant was diluted 9.9-fold using Milli-Q water adjusted to pH 3.0 with 1N HCl and subjected to solid-phase extraction using Sep-Pak Vac. RC (500-mg) C18 cartridges (Waters, Milford, MA). The samples were then eluted sequentially with methyl formate and methanol. Lipid metabolites in the methanol fractions were measured by ultra-performance liquid chromatography/time-of-flight mass spectrometry (UPLC-TOFMS; LCT Premier XE; Waters Micro-mass; Waters) for analysis of phospholipids, sphingolipids, and neutral lipids [16]. PUFAs and their oxidation products (oxylipins) in the methyl formate fraction were measured by UPLC/MS/MS using a 5500QTRAP quadrupole-linear ion trap hybrid mass spectrometer (AB Sciex, Framingham, MA) interfaced with an ACQUITY UPLC System (Waters). Transitions were determined for all individual PUFAs and oxylipins using MRM mode (further information in S2 Table). Because tetranor-prostaglandin D metabolite (tPGDM) and tetranor-prostaglandin E metabolite (tPGEM) are constitutional isomers with indistinguishable precursor and product ion mass and the same retention time (S2 Table), it was not possible to distinguish them using our LC/MS/MS method. The recovery of analytes after extraction is summarized in S3 Table.
Calibration curve
The external calibration curves were constructed by spiking the sample buffer (n = 3) with ten different concentrations (0.01 or 0.04–400 or 1000 nM) of analytes. Analyte concentrations are calculated as X (nM) to substitute [(IS normalized analyte area)/(extraction recovery)] for Y in polynomial expressions. The calibration data, including the polynomial expression of the approximate curve, calibration range, and correlation coefficient are all summarized in S3 Table.
Data processing
LC-TOFMS data were processed using the 2DICAL software package (Mitsui Knowledge Industry Co. Ltd., Tokyo, Japan) as described by Ono et al. [18]. Extracted ion peaks were subjected to identification of lipid molecules by comparing ion features, including RT, m/z, preferred adducts, and in-source fragments, in the experimental samples with those in the reference library of lipid molecule entries, as described previously [16]. The peak height of the detected lipid molecules was corrected to that of deuterated PC as an IS in each sample. The corrected value for each lipid was then normalized to the corresponding creatinine levels in each urine sample (S4 and S5 Tables).
UPLC/MS/MS data on PUFAs and oxylipins were processed using MultiQuant™ Software (Version 2.1; AB Sciex). The integrated peak area of the detected lipid molecules was corrected to that of deuterated LTB4-d4 as an IS in each sample. The concentration in the correction-applied samples was determined by using the calibration curve and by adjusting the extraction efficiency as described above. The concentration of each lipid was then normalized to the corresponding creatinine levels in each urine sample and expressed as μmol analyte /mmol creatinine (S6 and S7 Tables) as described in the Human Metabolome Database (http://www.hmdb.ca/).
ELISA
For urine volume normalization, the creatinine level in the urine of each subject was evaluated by enzyme-linked immunosorbent assay (TransGenic Inc., Kobe, Japan). Urine (10 μl) was diluted with 190 μl reaction buffer. The diluted sample was centrifuged at 1,500 rpm, and 70μl of the supernatant was transferred to a 96 well plate. After addition of 70 μl of reaction solution, the plate was incubated at RT for 1 h. After washing of the plate, chromogenic substrate solution (100 μl) was added to each well and incubated for 10 min. The absorption at 490 nm was analyzed using a microplate reader. Each plate comprised a calibration set and solvent blanks. (S5 and S7 Tables)
Statistical analysis
Statistical analyses were performed in the R statistical environment (http://r-project.org/). Metabolite levels among the four groups were compared by the Mann-Whitney test, and differences were considered statistically significant at p<0.05. To adjust for multiple comparisons, the candidate compounds were narrowed down based on a false-discovery-rate (FDR) adjusted q<0.05.
Results
Lipid profiles in urine from healthy individuals
Exact mass measurement using electrospray ionization mass spectrometry (ESI-TOFMS) in the simultaneous negative and positive mode resulted in the identification of different phospholipids in the methanol fractions from human urine. There were at least 220 negative and 180 positive detectable ion peaks in human urine; however, only 14 phospholipids were identified. Among them, relative quantification was performed for two phosphatidylcholines (PCs), one sphingomyelin (SM), one phosphatidylinositol (PI), and three ceramides (Cer)s (S4 Table). Similar to most studies on urinary metabolites using LC/MS [19, 20], we did not detected phosphatidylethanolamine, phosphatidylserine, and neutral lipids. The strongest signals belonged to SM (d18:1/16:0), PC (16:0/18:2), and PC (16:0/18:1) (S1 Fig), and the levels of these molecules did not significantly vary according to sex, age, or BMI (S9 Table).
To quantify the lipids in the methyl formate fraction, the triple quadrupole LC/MS system was operated under the multiple reaction monitoring (MRM) mode using electrospray ionization in the negative ion mode. Of the 46 metabolites scanned in this target lipidomic analysis (S2 Table), four PUFAs and 25 oxylipins were observed at detectable and quantifiable levels in human urine. Similar to other studies [21], 9-hydroxyoctadecadienoic acid (HODE), 9-oxooctadecadienoic acid (KODE), 12- hydroxyeicosatetraenoic acid (HETE), docosahexaenoic acid (DHA), arachidonic acid (AA), and prostaglandin (PG) derivatives were detected at relatively high levels among the monitored ions (S6 Table).
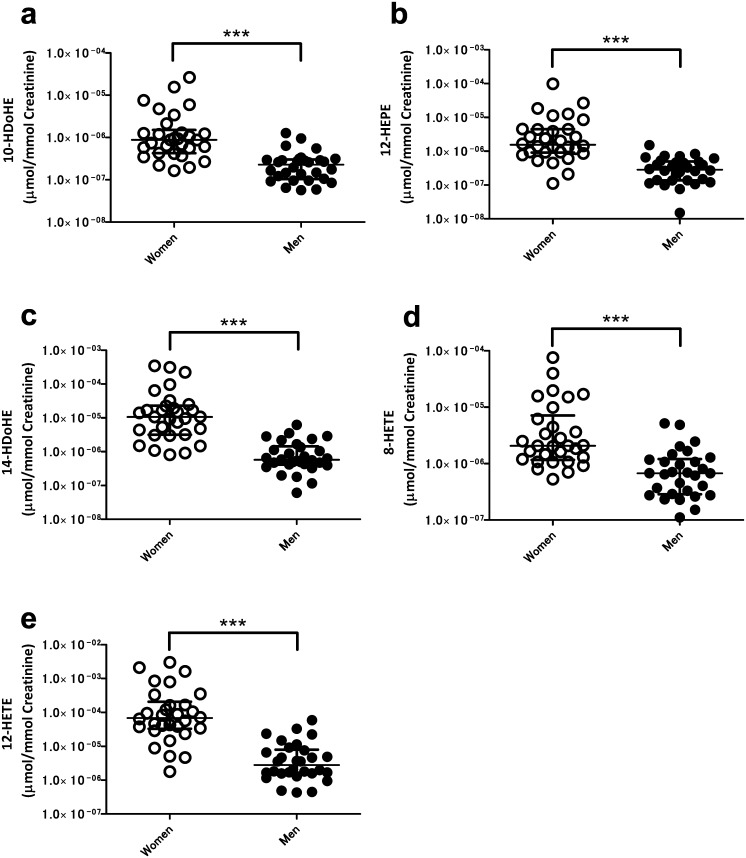
Higher urinary content of 12-LOX-produced oxylipins in female than men
To access impacts of physiological backgrounds on urinary lipid levels, we initially examined sex-related variations. Female urine contained high concentrations of three ω-3 oxylipins known to have anti-inflammatory and vasodilatory activities [22] [23] (Table 2 and S8 Table). Regardless of the double bond position, three 12-LOX-produced oxylipins were significantly enriched in female compared to male urine. The levels of 10-hydroxyldocosahexaenoic acid (HDoHE) (Fig 1a), 12- hydroxyeicosapentaenoic acid (HEPE) (Fig 1b), and 14-HDoHE (Fig 1c) were significantly higher in female urine. In agreement with previous reports [24], the levels of the urinary ω-6 fatty acid derivatives 8-HETE (Fig 1d) and 12-HETE (Fig 1e) were also significantly different between men and women.
Table 2. Sex-related oxylipins.
| Compound | Δ | Precursor | Pathway | Tendency | Ratio | P | Q | Effect |
|---|---|---|---|---|---|---|---|---|
| 10-HDoHE | ω3 | DHA | - | Women>Men | 3.8 | *** | $ $ $ | Anti-inflammation/ vasodilation |
| 12-HEPE | ω3 | EPA | 12-LOX | Women>Men | 5.4 | *** | $ $ $ | Anti-inflammation/ vasodilation |
| 14-HDoHE | ω3 | DHA | 12-LOX | Women>Men | 18.6 | *** | $ $ $ | Anti-inflammation/ vasodilation |
| 8-HETE | ω6 | AA | P450 | Women>Men | 3.1 | *** | $ $ $ | Inflammation/ vasodilation |
| 12-HETE | ω6 | AA | 12-LOX | Women>Men | 24.2 | *** | $ $ $ | Inflammation/ vasodilation |
Δ: The first double bond.
-: non-enzymatic.
Ratio represents the median ratio of the value in women to that in men.
***p < 0.001 by the Mann-Whitney U-test.
$ $ $q<0.001 by Benjamini-Hochberg procedure for FDR.
Fig 1. The association of urinary lipids with sex.
Women had higher concentrations of 10-HDoHE (a), 12-HEPE (b), 14-HDoHE (c), 8-HETE (d) and 12-HETE (e) than men. Open circles and closed circles show women and men subjects, respectively. The center bars show median and interquartile values normalized to respective creatinine levels; ***p < 0.001, by the Mann-Whitney U-test.
Higher urinary anti-hypertensive oxylipin levels in women than in men of young age
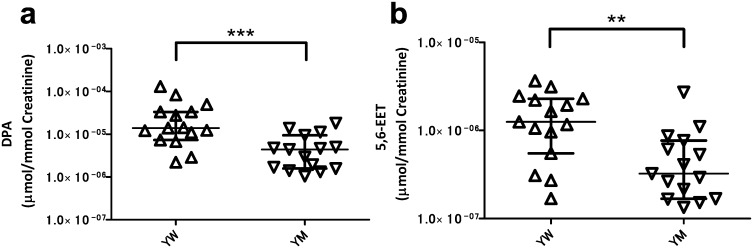
We identified a difference in the levels of several urinary oxylipins specific to young women (Table 3 and S8 Table). Young women showed high concentrations of five compounds with anti-hypertensive activities in their urine. Thus, compared to young men, young women had approximately 3–4 fold higher content of three PUFAs including AA, Docosapentaenoic acid (DPA) (Fig 2a), and Eicosapentaenoic acid (EPA). Three epoxyeicosatrienoic acids (EETs), which are P450 metabolites of AA [11], and included 11,12-EET, 14,15-EET, and 5,6-EET (Fig 2b) were also present in higher level in young women. DPA, EPA, and those EETs are anti-hypertensive mediators [25]. 15-HETE, a major AA metabolite [26], was also present at higher levels in the urine of young women.
Table 3. Young women- related oxylipins.
| Compound | Δ | Precursor | Pathway | Tendency | Ratio | P | Q | Effect |
|---|---|---|---|---|---|---|---|---|
| DPA | ω3 | ALA | PUFA | YW>YM | 3.2 | *** | $ $ | Anti-hypertensive |
| EPA | ω3 | ALA | PUFA | YW>YM | 3.5 | ** | $ | Anti-hypertensive |
| AA | ω6 | - | PUFA | YW>YM | 5.1 | * | $ | |
| 11,12-EET | ω6 | AA | P450 | YW>YM | 2.4 | * | $ | Anti-hypertensive |
| 14-15-EET | ω6 | AA | P450/- | YW>YM | 3.0 | ** | $ | Anti-hypertensive |
| 5,6-EET | ω6 | AA | P450 | YW>YM | 3.9 | ** | $ | Anti-hypertensive |
| 15-HETE | ω6 | AA | - | YW>YM | 2.9 | ** | $ | inflammation |
Δ: The first double bond.
-: non-enzymatic.
YW: young women.
YM: young men.
The ratio represents the median ratio the values in young women to those in young men. ALA: linokenic acid.
*p < 0.05,
**p < 0.01,
***p < 0.001 by the Mann-Whitney U-test.
$q<0.05,
$ $q<0.01 by Benjamini-Hochberg procedure for FDR.
Fig 2. The gender-related urinary oxylipins in young age.
Young women had higher concentration of DPA and 5,6-EET than young men (a and b). Open triangles and open inverted triangles show young women (YW) and young men (YM), respectively. The center bars show median and interquartile values normalized to the respective creatinine level. **p < 0.01, ***p < 0.001 by the Mann-Whitney U-test.
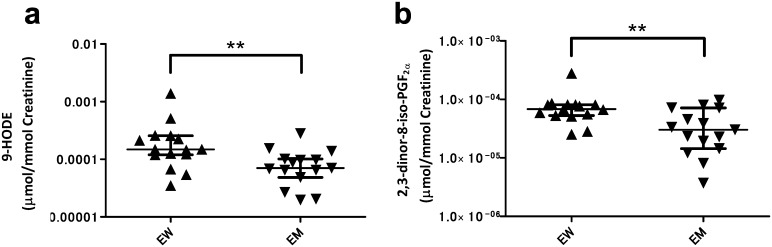
Higher urinary anti-inflammatory 5-LOX-pathway oxylipin levels in women than in men of elderly age
We next assessed the association of urinary lipid levels with elderly women (Table 4). Three metabolites, 9-HOTrE (hydroxyoctadecatrienoic acid), 9-KODE (oxooctadecadienoic acid,) and 9-HODE (hydroxyoctadecadienoic acid) (Fig 3a), which belong to 5-LOX pathway oxylipins [27] and putative oxidative stress markers, showed approximately 2-fold higher levels in elderly women than in elderly men. The level of 2,3-dinor-8-iso-PGF2α, a non-enzymatic AA metabolite and an oxidative stress marker [28], was even greater in elderly women, too (Fig 3b).
Table 4. Elderly women-related oxylipins.
| Compound | Δ | Precursor | Pathway | Tendency | Ratio | P | Q | Effect |
|---|---|---|---|---|---|---|---|---|
| 9-HOTrE | ω3 | ALA | 5-LOX | EW>EM | 2.2 | * | $ | Unknown |
| EW>YW | 0.3 | ** | $ | |||||
| 9-HODE | ω6 | LA | 5-LOX | EW>EM | 2.1 | ** | $ | Oxidative stress marker |
| 9-KODE | ω6 | LA | 5-LOX | EW>EM | 2.7 | ** | $ | Oxidative stress marker |
| 2,3-d-8-i-PGF2α | ω6 | AA | - | EW>EM | 2.2 | ** | $ | Oxidative stress marker |
2,3-d-8-i-PGF2α 2,3-dinor-8-iso- PGF2α.
Δ: the first double bond.
-: non-enzymatic.
EW: elderly women.
EM: elderly men.
Ratio represents the median ratio of elderly women to elderly men.
ALA: linolenic acid.
*p< 0.05,
**p< 0.01 by the Mann-Whitney U-test.
$q<0.05 by Benjamini-Hochberg procedure for FDR.
Fig 3. The gender-related urinary oxylipins in elderly age.
Elderly women had higher concentration of 9-HODE and 2,3-dinor-8-iso-PGF2α than other groups (a and b). Closed triangles, and closed inverted triangles show elderly women (EW) and elderly men (EM), respectively. The center bars represent median area values normalized to respective creatinine level. **p < 0.01 by the Mann-Whitney U-test.
No difference in urinary oxypilin levels between ages and BMIs
Urinaly oxylipin levels were compared between the young and elderly subjects of both sex. As shown in S8 Table, there were no oxypilins showing age-related difference within women and men groups. We also assessed the association of BMI and with urinary lipid concentration. Comparing subjects with lower BMI (< 30) and those with higher BMI (> 30), none of the oxypilins showed significant association with BMI (S8 Table).
Discussion
Our primary objective was to assess differences in urinary lipid levels between groups of healthy subjects classified by demographic variables of sex, age, and BMI to provide reference ranges for urinary lipidomics. Although there have been several reports on the association of urinary lipids with dietary control, disease status, and/or drug administration [29], this is the first report on cross-classification of urinary lipid content by age, sex, and BMI in healthy individuals after physiological fasting. Our results demonstrate that sex significantly impacted the measurement of urinary lipid metabolite levels in the healthy population. We previously performed serum and plasma lipid profiling in the same population investigated in the present study [16]; however, sex-related differences in the urinary oxylipins did not show a correspondence with those in serum/plasma oxylipins that we previously reported [16, 17]. In the present study, none of the analytes exhibit significant differences according to age or BMI, but 16 analytes showed sex differences in urine. Therefore, in measurement of urinary lipids, attention should be paid to the sex differences in at least these 16 analytes.
Oxylipins might be produced by the kidney because 12-HETE in the blood stream was not directly secreted into the urine in a previous study [30]. In the present study, oxylipins generated from ω-3 fatty acids had notably higher levels in female urine, which may be explained by the previous finding that the ω-3 conversion efficiency from linolenic acid (ALA) to longer-chain PUFAs is greater in women than in men [31]. Accordingly, anti-inflammatory and vasodilatory oxylipins had significantly higher concentrations in female urine than in male urine. 10-HdoHE, 12-HEPE, and 14-HDoHE are examples of potentially anti-inflammatory ω-3 fatty acids [32, 33]. Although the mechanisms underlying the observed sex differences remain unclear, our results suggest that 12-LOX is more active in women, accounting for the sex difference in oxylipin levels.
A recent study in spontaneously hypertensive rats revealed stronger renal vasodilator effects of AA, which could be accounted for by increased renal vascular sensitivity to EETs and K+ channel activation, leading to hyperpolarization and relaxation [25]. EETs are closely involved in the production of progesterone [34, 35], which may explain the difference observed between young and elderly women. There are no data on activation of EET synthesis by estrogen; however, dihydrotestosterone was previously shown to decrease EET levels [36], providing a possible reason why young women had higher urinary concentrations of EETs. Three oxylipins abundant in elderly women are regulated by the 5-LOX pathway [37]. 2,3-dinor-8-iso-PGF2α is more abundant in human urine than its precursor, 8-iso- PGF2α [38]. These oxidative stress markers might be particularly abundant in the urine of elderly women because of their comparatively higher BMI.
The unique oxylipin profile observed in urine can be attributed to the specific function that the kidneys perform by concentrating certain metabolites from blood. As the differential activity of renal enzymes is likely to be responsible for the differences in urinary oxylipins observed between the groups, urinary lipidome profiling could be an attractive approach for monitoring renal conditions and/or functional performance, especially considering the relative stability of urinary oxylipins [39]. These benefits could be used to enhance diagnostic confidence, precision, and reliability. The findings of this study, i.e, that urinary lipid metabolite levels in the healthy population vary across sexes, have implications for understanding the biochemical changes in urine associated with renal physiology and would contribute to the advancement of urine-based diagnostic strategies.
Supporting Information
(TIFF)
(XLSX)
(XLSX)
(XLSX)
(XLSX)
(XLSX)
(XLSX)
(XLSX)
(XLSX)
(XLSX)
Acknowledgments
The authors thank Ms. Masayo Urata for helpful assistance in sample preparation and Ms. Chie Sudo for secretarial assistance and support.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported in part by “Accelerating regulatory science initiative” from the Ministry of Health, Labour, and Welfare and in part by Grants from Japan Agency for Medical Research and development, AMED(YS). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Zhao YY, Vaziri ND, Lin RC. Lipidomics: new insight into kidney disease. Advances in clinical chemistry. 2015;68:153–75. Epub 2015/04/11. 10.1016/bs.acc.2014.11.002 [DOI] [PubMed] [Google Scholar]
- 2.Lee H, Kim H. Membrane topology of transmembrane proteins: determinants and experimental tools. Biochem Biophys Res Commun. 2014;453(2):268–76. Epub 2014/06/19. 10.1016/j.bbrc.2014.05.111 [DOI] [PubMed] [Google Scholar]
- 3.Shao S, Yang Y, Yuan G, Zhang M, Yu X. Signaling molecules involved in lipid-induced pancreatic beta-cell dysfunction. DNA and cell biology. 2013;32(2):41–9. Epub 2013/01/26. 10.1089/dna.2012.1874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buckley ML, Ramji DP. The influence of dysfunctional signaling and lipid homeostasis in mediating the inflammatory responses during atherosclerosis. Biochimica et biophysica acta. 2015;1852(7):1498–510. Epub 2015/04/19. 10.1016/j.bbadis.2015.04.011 [DOI] [PubMed] [Google Scholar]
- 5.Kasumov T, Li L, Li M, Gulshan K, Kirwan JP, Liu X, et al. Ceramide as a mediator of non-alcoholic Fatty liver disease and associated atherosclerosis. PloS one. 2015;10(5):e0126910 Epub 2015/05/21. 10.1371/journal.pone.0126910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hao CM, Breyer MD. Physiologic and pathophysiologic roles of lipid mediators in the kidney. Kidney international. 2007;71(11):1105–15. 10.1038/sj.ki.5002192 [DOI] [PubMed] [Google Scholar]
- 7.Tessaro FH, Ayala TS, Martins JO. Lipid mediators are critical in resolving inflammation: a review of the emerging roles of eicosanoids in diabetes mellitus. BioMed research international. 2015;2015:568408 Epub 2015/04/14. 10.1155/2015/568408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bruins MJ, Dane AD, Strassburg K, Vreeken RJ, Newman JW, Salem N Jr., et al. Plasma oxylipin profiling identifies polyunsaturated vicinal diols as responsive to arachidonic acid and docosahexaenoic acid intake in growing piglets. Journal of lipid research. 2013;54(6):1598–607. Epub 2013/04/02. 10.1194/jlr.M034918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simmons DL, Botting RM, Hla T. Cyclooxygenase isozymes: the biology of prostaglandin synthesis and inhibition. Pharmacol Rev. 2004;56(3):387–437. 10.1124/pr.56.3.3 [DOI] [PubMed] [Google Scholar]
- 10.Dobrian AD, Lieb DC, Cole BK, Taylor-Fishwick DA, Chakrabarti SK, Nadler JL. Functional and pathological roles of the 12- and 15-lipoxygenases. Prog Lipid Res. 2011;50(1):115–31. 10.1016/j.plipres.2010.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Imig JD, Falck JR, Inscho EW. Contribution of cytochrome P450 epoxygenase and hydroxylase pathways to afferent arteriolar autoregulatory responsiveness. British journal of pharmacology. 1999;127(6):1399–405. Epub 1999/08/24. 10.1038/sj.bjp.0702662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsalik EL, Willig LK, Rice BJ, van Velkinburgh JC, Mohney RP, McDunn JE, et al. Renal systems biology of patients with systemic inflammatory response syndrome. Kidney international. 2015. Epub 2015/05/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pasikanti KK, Esuvaranathan K, Hong Y, Ho PC, Mahendran R, Raman Nee Mani L, et al. Urinary metabotyping of bladder cancer using two-dimensional gas chromatography time-of-flight mass spectrometry. Journal of proteome research. 2013;12(9):3865–73. Epub 2013/07/28. 10.1021/pr4000448 [DOI] [PubMed] [Google Scholar]
- 14.Gil AM, de Pinho PG, Monteiro MS, Duarte IF. NMR metabolomics of renal cancer: an overview. Bioanalysis. 2015. Epub 2015/09/24. [DOI] [PubMed] [Google Scholar]
- 15.Full-Length Blood Donor History Questionnaire, Version 1.3. AABB. 2008. http://www.aabb.org/tm/questionnaires/Documents/dhq/v1-3/Full-LengthDonorHistoryQuestionnairev1.3.pdf
- 16.Ishikawa M, Maekawa K, Saito K, Senoo Y, Urata M, Murayama M, et al. Plasma and serum lipidomics of healthy white adults shows characteristic profiles by subjects' gender and age. PloS one. 2014;9(3):e91806 10.1371/journal.pone.0091806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saito K, Maekawa K, Pappan KL, Urata M, Ishikawa M, Kumagai Y, et al. Differences in metabolite profiles between blood matrices, ages, and sexes among Caucasian individuals and their inter-individual variations. Metabolomics. 2013;10(3). [Google Scholar]
- 18.Ono M, Shitashige M, Honda K, Isobe T, Kuwabara H, Matsuzuki H, et al. Label-free quantitative proteomics using large peptide data sets generated by nanoflow liquid chromatography and mass spectrometry. Mol Cell Proteomics. 2006;5(7):1338–47. Epub 2006/03/23. 10.1074/mcp.T500039-MCP200 [DOI] [PubMed] [Google Scholar]
- 19.Bouatra S, Aziat F, Mandal R, Guo AC, Wilson MR, Knox C, et al. The human urine metabolome. PloS one. 2013;8(9):e73076 10.1371/journal.pone.0073076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fuller M, Sharp PC, Rozaklis T, Whitfield PD, Blacklock D, Hopwood JJ, et al. Urinary lipid profiling for the identification of fabry hemizygotes and heterozygotes. Clinical chemistry. 2005;51(4):688–94. 10.1373/clinchem.2004.041418 [DOI] [PubMed] [Google Scholar]
- 21.Sasaki A, Fukuda H, Shiida N, Tanaka N, Furugen A, Ogura J, et al. Determination of omega-6 and omega-3 PUFA metabolites in human urine samples using UPLC/MS/MS. Analytical and bioanalytical chemistry. 2015;407(6):1625–39. 10.1007/s00216-014-8412-5 [DOI] [PubMed] [Google Scholar]
- 22.Flachs P, Ruhl R, Hensler M, Janovska P, Zouhar P, Kus V, et al. Synergistic induction of lipid catabolism and anti-inflammatory lipids in white fat of dietary obese mice in response to calorie restriction and n-3 fatty acids. Diabetologia. 2011;54(10):2626–38. Epub 2011/07/23. 10.1007/s00125-011-2233-2 [DOI] [PubMed] [Google Scholar]
- 23.Cunningham FM, Woollard PM, Camp RD. Proinflammatory properties of unsaturated fatty acids and their monohydroxy metabolites. Prostaglandins. 1985;30(3):497–509. Epub 1985/09/01. [DOI] [PubMed] [Google Scholar]
- 24.Suzuki N, Hishinuma T, Saga T, Sato J, Toyota T, Goto J, et al. Determination of urinary 12(S)-hydroxyeicosatetraenoic acid by liquid chromatography-tandem mass spectrometry with column-switching technique: sex difference in healthy volunteers and patients with diabetes mellitus. Journal of chromatography B, Analytical technologies in the biomedical and life sciences. 2003;783(2):383–9. Epub 2002/12/17. [DOI] [PubMed] [Google Scholar]
- 25.Imig JD. Epoxyeicosatrienoic acids, hypertension, and kidney injury. Hypertension. 2015;65(3):476–82. 10.1161/HYPERTENSIONAHA.114.03585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kumlin M, Hamberg M, Granstrom E, Bjorck T, Dahlen B, Matsuda H, et al. 15(S)-hydroxyeicosatetraenoic acid is the major arachidonic acid metabolite in human bronchi: association with airway epithelium. Archives of biochemistry and biophysics. 1990;282(2):254–62. Epub 1990/11/01. [DOI] [PubMed] [Google Scholar]
- 27.Klawitter J, Zafar I, Klawitter J, Pennington AT, Klepacki J, Gitomer BY, et al. Effects of lovastatin treatment on the metabolic distributions in the Han:SPRD rat model of polycystic kidney disease. BMC Nephrol. 2013;14:165 Epub 2013/08/02. 10.1186/1471-2369-14-165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang H, Il’yasova D, Sztaray J, Young SP, Wang F, Millington DS. Quantification of the Oxidative Damage Biomarker 2,3-Dinor-8-Isoprostaglandin-F2α in Human Urine Using Liquid Chromatography-Tandem Mass Spectrometry. Analytical biochemistry. 2010;399(2):302–4. 10.1016/j.ab.2009.12.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fu J, Schoeman JC, Harms AC, van Wietmarschen HA, Vreeken RJ, Berger R, et al. Metabolomics profiling of the free and total oxidised lipids in urine by LC-MS/MS: application in patients with rheumatoid arthritis. Analytical and bioanalytical chemistry. 2016. Epub 2016/07/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clouet P, Niot I, Bouchard P, Gree R, Lellouche JP, Beaucourt JP, et al. Distribution of tritium labeled 12(S) hydroxy-eicosatetraenoic acid (12-HETE) in the rat. Prostaglandins. 1991;42(1):39–45. Epub 1991/07/01. [DOI] [PubMed] [Google Scholar]
- 31.Burdge GC, Calder PC. Conversion of alpha-linolenic acid to longer-chain polyunsaturated fatty acids in human adults. Reproduction, nutrition, development. 2005;45(5):581–97. Epub 2005/09/29. 10.1051/rnd:2005047 [DOI] [PubMed] [Google Scholar]
- 32.McDaniel JC, Massey K, Nicolaou A. Fish oil supplementation alters levels of lipid mediators of inflammation in microenvironment of acute human wounds. Wound Repair Regen. 2011;19(2):189–200. 10.1111/j.1524-475X.2010.00659.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Serhan CN, Yang R, Martinod K, Kasuga K, Pillai PS, Porter TF, et al. Maresins: novel macrophage mediators with potent antiinflammatory and proresolving actions. J Exp Med. 2009;206(1):15–23. 10.1084/jem.20081880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nakagawa K, Holla VR, Wei Y, Wang WH, Gatica A, Wei S, et al. Salt-sensitive hypertension is associated with dysfunctional Cyp4a10 gene and kidney epithelial sodium channel. The Journal of clinical investigation. 2006;116(6):1696–702. Epub 2006/05/13. 10.1172/JCI27546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zosmer A, Elder MG, Sullivan MH. The production of progesterone and 5,6-epoxyeicosatrienoic acid by human granulosa cells. The Journal of steroid biochemistry and molecular biology. 2002;81(4–5):369–76. Epub 2002/10/04. [DOI] [PubMed] [Google Scholar]
- 36.Garcia V, Cheng J, Weidenhammer A, Ding Y, Wu CC, Zhang F, et al. Androgen-induced hypertension in angiotensinogen deficient mice: role of 20-HETE and EETS. Prostaglandins & other lipid mediators. 2015;116–117: 124–30. Epub 2014/12/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stachowska E, Dziedziejko V, Safranow K, Jakubowska K, Olszewska M, Machalinski B, et al. Effect of conjugated linoleic acids on the activity and mRNA expression of 5- and 15-lipoxygenases in human macrophages. Journal of agricultural and food chemistry. 2007;55(13):5335–42. Epub 2007/06/07. 10.1021/jf0701077 [DOI] [PubMed] [Google Scholar]
- 38.Chiabrando C, Valagussa A, Rivalta C, Durand T, Guy A, Zuccato E, et al. Identification and measurement of endogenous beta-oxidation metabolites of 8-epi-Prostaglandin F2alpha. The Journal of biological chemistry. 1999;274(3):1313–9. Epub 1999/01/09. [DOI] [PubMed] [Google Scholar]
- 39.Levison BS, Zhang R, Wang Z, Fu X, DiDonato JA, Hazen SL. Quantification of fatty acid oxidation products using online high-performance liquid chromatography tandem mass spectrometry. Free Radic Biol Med. 2013;59:2–13. Epub 2013/03/19. 10.1016/j.freeradbiomed.2013.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIFF)
(XLSX)
(XLSX)
(XLSX)
(XLSX)
(XLSX)
(XLSX)
(XLSX)
(XLSX)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.