Abstract
Background
Studies have shown that patients admitted to hospitals on weekends and after-hours experience worse outcome than those admitted on weekdays and daytime hours. Although admissions of patients to intensive care units (ICUs) occur 24 hours a day, not all critical care units maintain the same level of staffing during nighttime, weekends, and holidays. This raises concerns in view of evidence showing that the organizational structure of an ICU influences the outcome of critically ill patients. The objective of this study is to evaluate the effects of day and time of admission to ICU on patients’ outcome.
Methods
A single-center, prospective, observational study was conducted among all consecutive admissions to ICU in a community teaching hospital during a 4-month period.
Results
A total of 282 patients were admitted during the study period. Their mean age was 59.5 years (median 59, range 17–96), and the majority were male (157, 55.7%). Mean Acute Physiology and Chronic Health Evaluation (APACHE)-II score was 18.9 (median 33, range 1–45), and mean ICU length of stay was 3.1 days (median 2, range 1–19). Of the patients, 104 patients (36.9%) were admitted during weekends and 178 (63.1%) during weekdays. A total of 122 patients (43.3%) were admitted after-hours, constituting 68.5% of all admissions during weekdays. Fifty-six patients (19.9%) were admitted during daytime hours, representing 31.5% of all weekday admissions. Forty-five patients (15.9%) died in ICU. Compared to patients admitted on weekends, those admitted on weekdays had increased ICU mortality (operating room (OR)=0.437; 95% confidence interval=0.2054–0.9196; p=0.0293).
Conclusion
Admissions to ICU during weekends were not independently associated with increased mortality. A linear relationship between weekdays and after-hours admissions to ICU with mortality was observed at our institution.
Keywords: intensive care unit, weekdays, weekends, after-hours, outcome
Identification of factors that may influence patients’ outcome at the institutional level is crucial for quality control purposes and benchmarking. Studies examining hospital outcome of patients admitted to intensive care units (ICUs) have suggested an increased mortality in those admitted after-hours and/or weekends (1–6). Provided that an adequate staffing and services are maintained, the timing of ICU admission should not be associated with mortality. However, only sparse data are available on the relationship between the time and day of admission and mortality in ICU, and the few published reports yielded a contradictory information, perhaps because of differences in case mixes, staffing levels, and technology available among different ICUs. These studies have mainly focused on whether the absence of on-site intensivists after-hours significantly increases the mortality of patients admitted to ICU. The Leapfrog Group ICU Standard suggests that intensivists should be present in the ICU during the daytime hours, but they are not required to be present during off-hours provided that pages are returned at least 95% of the time within 5 min and arrangements are made for a qualified healthcare professional to reach the patient within 5 min. Since critically ill patients are at a high risk of adverse outcomes, necessary staffing, diagnostic studies, and therapeutic procedures ideally should be available at all times. However, costs pressures and market realities may lead to decreased staffing during the weekends and night shifts, which may contribute to poor outcomes in patients admitted to ICU (7). An increased risk of death associated with care during different times of the day or different days of the week may reflect inconsistencies in the availability or quality of care, which is a major safety issue that must be addressed. On the contrary, patients admitted in the after-hours and weekends may be intrinsically at higher risk for death by virtue of a different case-mix, increased severity of illness, or some other unmeasured factors as compared with patients admitted during the usual daytime hours and weekdays. A number of factors have been suggested to influence after-hours and weekends admission effects not limited to reduced nursing and other healthcare workers staffing, closed versus open ICU models, experience and availability of intensivists, and access to treatments and procedures in the after-hours and weekends (4, 6, 8–10). Some studies have shown that the availability of 24-hour ICU coverage by trained intensivists does not decrease the mortality of patients in ICU (11, 12), while other reports have suggested better outcomes in critically ill patients admitted to closed ICUs (13, 14). As the focus of critical care worldwide is to improve care for critically ill patients, continued studies of hospital and ICU organizational and structural factors to improve outcomes for patients are warranted. The objective of this study is to determine the effects of admission time and day on patients’ outcome in the ICU in a community, inner-city hospital with a relatively uniform staffing and availability of diagnostic and therapeutic options.
Materials and methods
Study design and patient population
The study has a prospective, observational design. It was conducted in a general, university-affiliated, community inner-city hospital located in Brooklyn, New York. The hospital has a total of 346 beds, distributed among general internal medicine, general surgery, obstetrics/gynecology, psychiatry, and pediatrics wards. As per institutional policy, patients requiring mechanical ventilation and/or vasoactive therapy should be admitted either to ICU or step-down unit (SDU). The ICU in our hospital is a medical-surgical ICU, a closed unit composed of 12 beds with an annual admission average of more than 600 patients. During daytime, the nursing:patient ratio in the ICU is 1:2, and it is maintained irrespective of the day of the week. It drops to 1:3 during night shifts. Respiratory therapists and pharmacists are available in-house at all times. Allied healthcare professionals such as medical students, nutritionists, and social workers staff the ICU only during weekdays (8 a.m. to 4 p.m.). The critical care medicine (CCM) service is constituted by five board-certified intensivists, who provide 16 hours a day in-house coverage that includes weekends and holidays (8 a.m. to 12 a.m.). The ICU attending intensivist guides bedside patients’ rounds during daytime, supervises invasive procedures, writes notes on every patient on daily basis, and is available for consultations at all times. A second, shorter round undergoes at 4 p.m., when the after-hours attending intensivist takes sign-out about the status of all patients in the ICU. Intensivists are available to guide patient care by phone from 12 a.m. until 8 a.m., and to come to ICU as needed. Internal Medicine residents staffed the ICU at a constant level, 24 hours a day/7 days a week. A third-year, senior medical resident evaluates all ICU consultations, and the CCM attending on-duty is required to assess and/or discuss every patient for whom a consultation is requested. The CCM team receives notification and approves all the admissions to the ICU. From 7 a.m. to 7 p.m. (Sundays through Fridays), a third-year resident and a second-year resident are present in ICU, whereas a second-year resident and a first-year resident staff the ICU from 7 p.m. to 7 a.m. On Saturdays, a third-year resident and a second-year resident cover ICU for 24 hours. There are no standard definitions of ‘weekdays’, ‘weekends’, or ‘after-hours’ for intensive care practice in the United States, and previous publications have not used a consistent definition. For the purpose of this study, weekdays admissions were those from Mondays through Fridays, and they comprised daytime admissions (8 a.m. to 4 p.m.) and nighttime admissions (4 p.m. to 12 a.m., Mondays through Thursdays). Weekends admissions were defined as admissions to ICU from Fridays to Mondays (4 p.m. to 8 a.m.). After-hours admissions were those arriving to ICU between 4 p.m. and 8 a.m., from Mondays through Fridays, and were divided as nighttime admissions (4 p.m. to 12 a.m., Mondays through Thursdays) and late-night admissions (12 a.m. to 8 a.m., Tuesdays through Fridays).
All adult patients admitted to the ICU during the study period were enrolled in the cohort. In patients readmitted to the ICU during the same hospital stay, only data from the first admission were analyzed. We excluded patients admitted to SDU, since this treatment area could not be considered as a standard ICU. Each day, the number of ICU admissions was recorded. Variables such as age, gender, patients’ location before arrival to ICU, Acute Physiology and Chronic Health Evaluation (APACHE)-II score on admission to ICU, time and day of the week of arrival to ICU, ICU length of stay (LOS), and outcome at ICU discharge were prospectively measured and retrospectively analyzed. The primary endpoint in this study was ICU mortality. Using the t-test and analysis of variance statistical methodology, outcomes at different admission times and days were examined on a three-group comparison of weekdays, after-hours, and weekends admissions. Electronic medical records were reviewed, and clinical information was abstracted for each patient. After waiving the needs for informed consent, Institutional Review Board approved the study.
Results
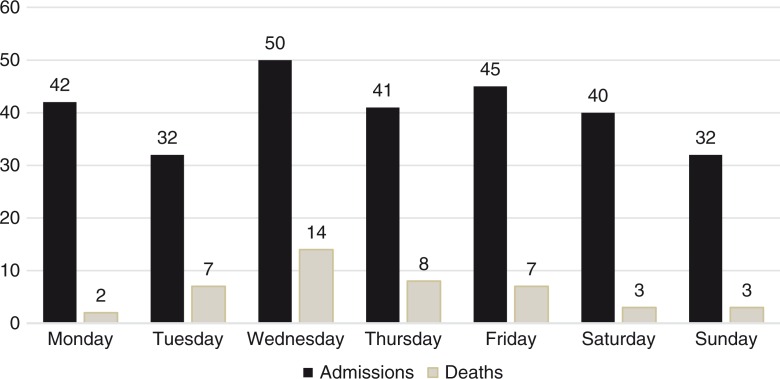
A total of 282 patients were admitted to ICU during the study period. From those, 10 patients (3.5%) were readmitted to ICU after being transferred to hospital wards. One hundred seventy-eight patients (63.1%) were admitted during weekdays and 104 (36.9%) on the weekends. Of the total admissions, 122 patients (43.3%) were admitted after-hours: 67 patients (54.9%) were admitted during nighttime and 55 (45.1%) during late-night hours. Fifty-six patients (19.9%) were admitted during daytime hours. Overall, the mean age was 59.5 years (median 59, range 17–96), and the majority of patients were male (157, 55.7%). Two hundred patients (71%) were admitted from the emergency department (ED), 55 (19.5%) were transferred from the hospital wards, 14 (4.9%) were admitted from operating rooms/post-anesthesia care unit (OR/PACU), and 13 (4.6%) were transferred from SDU. Most common days of admissions to ICU were Wednesdays (50, 17.7%), Fridays (45, 16%), Mondays (42, 14.8%), and Saturdays (40, 14.1%). Overall, the mean APACHE-II score was 18.9 (median 33, range 1–45). The mean APACHE-II score of patients admitted during the daytime hours was 20.3 (median 19, range 6–45; SD=9.12), and for those admitted during the nighttime and late-night hours, it was 18.3 (median 17, range 3–39; SD=8.87) and 20.3 (median 20, range 1–41; SD=9.72), respectively. There was no statistically significant difference between APACHE-II scores of patients admitted during daytime, after-hours, and late-night hours (p=0.37). The mean APACHE-II score of patients admitted during weekends was 17.4 (median 17, range 2–38). No significant statistical difference resulted from the comparison of APACHE-II scores of patients admitted on weekdays and weekends (p=0.12). A total of 1,160 ICU days were utilized during the study period. The mean ICU LOS was 3.1 days (median 2, range 1–19). Patients admitted during the weekdays required a total of 579 ICU days (mean 3.3, median 2, range 1–19), while those admitted during the weekends and after-hours utilized 302 days (mean 2.9, median 2, range 1–12) and 279 days (mean 3.4, median 2, range 1–19), respectively. Forty-five patients (15.9%) expired in ICU. Their mean age was 65.1 years (median 65, range 30–95), with a mean APACHE-II score of 25.8 (median 26, range 10–45). Fifteen of those patients (33.3%) were transferred to ICU from other units, most commonly from Medicine wards (8, 53.3%). Thirty-five of those patients who died (77.8%) were admitted during the weekdays: 13 (28.9%) were admitted during daytime hours (cumulative mortality=0.2321), 9 (20%) during nighttime hours (cumulative mortality=0.1343), and 13 (28.9%) during late-night hours (cumulative mortality=0.2363; OR=1.3742; 95% confidence interval (CI)=0.6342–2.9776; p=0.42). Patients admitted during daytime hours had increased ICU mortality compared with those admitted after-hours (RR=1.28). Ten patients (22.2%) admitted during the weekends expired while receiving treatment in ICU (OR=0.437; 95% CI=0.2054–0.9196; p=0.0293). The relationship between days of admission and mortality is shown in Table 1 and Fig. 1. Patients who expired consumed a total of 125 ICU days (10.8% of the total of ICU days; mean 2.8 days, median 2, range 1–13). Patients expired more frequently when they were admitted on Wednesdays (14, 31.1%), Thursdays (8, 17.8%), Tuesdays (7, 15.7%), and Fridays (7, 15.7%). Table 2 shows the relationship between the number of admissions, APACHE-II scores, and mortality.
Table 1.
Relationship between day and time of admission and mortality
| Admission time | Mortality | Survive | Total | Cumulative mortality | |
|---|---|---|---|---|---|
| Weekdays | Daytime | 13 | 43 | 56 | 0.2321 |
| Night-time | 9 | 58 | 67 | 0.1343 | |
| Late-night | 13 | 42 | 55 | 0.2363 | |
| After-hour (Night-time + Late-night) |
22 | 100 | 122 | 0.1803 | |
| Weekends | 10 | 94 | 104 | 0.0961 | |
Fig. 1.
Graphic relationship between days of admission and mortality.
Table 2.
Relationship between the number of admissions, APACHE-II scores, and mortality
| Weekdays (178, 63.1%) | |||||
|---|---|---|---|---|---|
| Daytime | Nighttime | Late-night | Weekends | Total | |
| Number of admissions | 56 (19.9%) | 67 (54.9%) | 55 (45.1%) | 104 (36.9%) | 282 |
| Mean APACHE-II scores | 20.3 | 18.3 | 20.3 | 17.4 | 18.9 |
| Mortality (%) | 13 (28.9%) | 9 (20%) | 13 (23.6%) | 10 (22.2%) | 45 (15.9%) |
Discussion
This study examined the characteristics and outcome of critically ill patients admitted to ICU during weekdays, after-hours, and weekends. This is the first study related to the timing of admission to ICU and its relationship with patients’ outcome guided in the New York City Health and Hospitals Corporation, the largest municipal healthcare system in the United States. It is also one of the very few studies conducted in the United States exploring the relationship between the day and time of admission to ICU with patients’ outcome. Our patients’ demographics are homogeneous to those described in other reports (1, 3, 15–17), and so was their ICU LOS (1, 15, 16, 18). There was no statistically significant difference between the LOS of patients admitted during weekdays, weekends, or after-hours. However, patients admitted during weekdays utilized more ICU days than those admitted during weekends and after-hours (49.9% vs. 26% vs. 24.1% of the total of ICU days, respectively), probably as a result of the increased number of admissions during weekdays. Not surprisingly, and similar to other large studies (1, 16, 19), the majority of patients were admitted from the ED. Although urgencies of critically ill patients may be the same, their priorities can be different. Equally important is the pertinent triage of these critically ill patients to appropriate locations within the hospital, which includes not only ICU but also SDU, palliative and terminal care units. Since our institution does not have a dedicated palliative care unit, and because of our institutional policy of not allowing patients requiring mechanical ventilation and/or vasopressors on medical wards, the authors suspect that some of these patients may have been incidentally admitted to ICU under such circumstances. The severity of illness of these patients was assessed using the APACHE-II score system. APACHE-II scores in our cohort are comparable to that of other studies (5, 19). There were no statistically significant differences between APACHE-II scores of patients admitted during the weekdays, weekends, and after-hours.
The overall, observed unadjusted ICU mortality (15.9%) in our cohort is related to that found in other similar studies (2–4, 17, 20), although it is lower than that in other reports (5, 16). The observed mortality of patients admitted during weekends falls into the range of 11.1–38.3% previously reported in other studies (1, 4, 15, 17, 19, 21). However, our results failed to support the linear relationship between admissions to ICU during weekends and excess mortality, as suggested in other publications (1, 2, 4, 5, 8, 15, 17, 18, 22). The adverse effects of weekend care, or ‘weekend effect’, resulting from inadequate staffing and support systems are likely to be more pronounced in community hospitals than in tertiary care center ICUs. Although our institution is a member of the New York City public hospitals system, a relatively uniform and balanced staffing as well as diagnostic and therapeutic modalities is maintained 24 hours a day/7 days a week. This may possibly explain the diminished expression of the ‘weekend effect’ in the outcome of patients admitted during weekends at our institution. In our cohort, and congruent to published data (16, 19, 23), admissions to ICU during weekends were not independently associated with increased mortality. We may speculate that the decreased mortality observed among patients admitted during weekends was probably related to the fact that these patients were ‘less sick’ than those admitted during weekdays, and that the number of weekends admissions was lower than that of weekdays admissions. Furthermore, there are no administrative activities, and family meetings are decreased to minimum on weekends, which may had led to a more focused patient care.
On the contrary, the observed mortality of patients admitted to ICU on weekdays and after-hours was significantly higher than that found in other reviews (3, 8, 15–17, 19, 22). It is important to emphasize that the proportion of patients in our cohort admitted during weekdays and after-hours was higher than that previously reported in other similar studies (3, 15, 16, 19, 23). Although more patients were admitted during weekdays than on weekends, we do not have an accurate explanation for the observed higher mortality rate of weekday admissions. Similar to other communications (3, 20), and contradicting data from other studies showing no differences in mortality between daytime and nighttime admissions (4, 19), our results showed an observed increased mortality among patients admitted during daytime. Balancing patients’ needs for critical care with the available critical care resources is a great challenge. We hypothesized that the frequent, decreased beds availability in the SDU at our institution may have led to an increased mortality resulting from ICU overcrowding, as a consequence of admitting ‘very ill’ and/or poor prognosis patients to ICU that otherwise might have been admitted to SDU. However, we are not convinced that it completely explains the differences in the observed mortality between weekdays, weekends, and after-hours admissions. Physicians and nursing staff evaluations and treatments of patients admitted to ICU during daytime shifts could be delayed more than those admitted during after-hours shifts. Nursing workloads might be heavier relative to the nurse:patient ratio because of the higher volume of medical orders, invasive procedures, and patients transportation for diagnostic tests outside the ICU. We also suspect that the predominantly diurnal organization of the ICU at our institution (patients’ rounds, higher volume of medical orders, administrative and teaching responsibilities, interactions with patients’ families, etc.) may have played a non-negligible and unquantifiable role that could have interfered with patients management and indirectly impinged on the quality of care. Furthermore, because of the large amount of invasive procedures and diagnostic interventions during the daytime, the work overload could be a source of diverted attention and energies contributing unintentionally to higher mortality. As in other studies (19, 20), we observed an increased mortality in patients transferred to ICU from hospital wards. Similar to other large cohorts (2, 4, 5, 8, 15), we have also observed an increased mortality in patients admitted after-hours, especially in those admitted during late-night hours. These findings contradict data from previous studies (3, 16, 20, 23). Available information in the medical literature has shown mixed results related to differences in mortality between daytime and night-time admissions to ICU, based on the presence or absence of an in-house intensivist during after-hours. Laupland et al. (2) reported an excess mortality in patients admitted to ICU during nighttime when no intensivist was in-house, pairing data published by Meynaar et al. (24) under similar circumstances. However, two other reports showed no increased mortality for nighttime admissions even in the absence of an in-house intensivist after-hours (4, 19). It may be reasonable to assume that, because of lower staffing levels and possible suboptimal processes of care, after-hours admissions to ICU could be associated with adverse outcomes. It is widely acknowledged by critical care nursing organizations globally that staffing and workforce issues are important to ICU patients’ outcomes. Time constraints related to a reduced nurse:patient ratio may increase the likelihood of mistakes by creating a stressful environment that adversely affects the quality of care. Therefore, it has been postulated that high nurse staffing numbers are associated with lower ICU mortality (25). Some meta-analyses have suggested that, in closed ICUs, the presence of high-intensity intensivists staffing, 24 hours a day/7 days a week, would help in ensuring consistency of care and improved outcomes (3, 23, 26–28). We conjecture that the decreased nursing:patient ratio during after-hours at our institution as well as the absence of an in-house intensivist after midnight may had contributed to poorer outcomes in patients admitted during late-night hours. Although the availability of an in-house intensivist during late-night hours may not necessarily reduce the mortality in ICU, it may have other benefits including an effect on the quality of end-of-life as well as in the appropriate triage of critically ill patients with a more rational allocation of ICU resources. As in many other institutions, our ICU is staffed with residents during late-night hours. Staffing models including nighttime use of medical residents to cover ICU appear to be safe and effective with no increase in ICU mortality (29). Nonetheless, some concerns have been raised regarding the experience of the covering physicians and its possible influence on patients’ outcome. A Canadian study found that nearly 50% of physicians who provide overnight staffing have less than 3 months of ICU experience (30). Protocolized ICUs and tele-ICUs have been proposed as alternatives to 24/7 intensivist coverage. In one study, protocolized ICU care driven by intensivist rounding during daytime was associated with the same morbidity and mortality as 24-hour in-house intensivist coverage (31). Although an unrecognized confounding variable may explain the observed increased mortality risk associated with weekdays and after-hours admissions to ICU, the possibilities that this may be related to inconsistencies in provision of care within or outside ICU are compelling and warrant further investigation.
This study has few potential limitations. First, it is important to note that there is no general consensus on what defines ‘after-hours’, ‘late-night’, or weekend care, and definitions have varied among several studies. Second, it was conducted in a single institution, and, therefore, our findings may not be applicable to other ICUs with varying staffing models. Third, despite the large number of consecutive patients enrolled, the study may have been underpowered and a larger sample size obtained by extending the study period would perhaps have revealed additional significant differences. Fourth, our study is focused in the ICU environment, and the authors did not have completed and detailed data on care provided on hospital wards or ED before patients arrived to ICU. Another, not less important limitation, is that our results may have been influenced by the lack of risk adjustment with different measured variables. However, we postulate that the data presented in this study provide interesting insights on the timing of admission to ICU and its relationship with patients’ outcome.
Conclusion
We found that weekend admissions to ICU were not associated with increased mortality, as opposed to admissions to ICU during weekdays and after-hours. Our results may have important implications for organization of ICU services. Further investigations are warranted to examine whether changes in process of care may reduce the excess mortality related to weekdays and after-hours admissions to ICU.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.Barnett MJ, Kaboli PJ, Sirio CA, Rosenthal GE. Day of the week of intensive care unit admission and patient outcomes: A multisite regional evaluation. Med Care. 2002;40(6):530–9. doi: 10.1097/00005650-200206000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Laupland KB, Shahpari R, Kirkpatrick AW, Stelfox HT. Hospital mortality among adults admitted to and discharged from intensive care on weekends and evenings. J Crit Care. 2008;23(3):317–24. doi: 10.1016/j.jcrc.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Luyt CE, Combes A, Aegerter P, Guidet B, Troulliet JL, Gilbert C, et al. Mortality among patients admitted to intensive care units during weekday day shifts compared with ‘off’ hours. Crit Care Med. 2007;35(1):3–11. doi: 10.1097/01.CCM.0000249832.36518.11. [DOI] [PubMed] [Google Scholar]
- 4.Uusaro A, Kari A, Ruokonen E. The effects of ICU admission and discharge times on mortality in Finland. Intensive Care Med. 2003;29(12):2144–8. doi: 10.1007/s00134-003-2035-1. [DOI] [PubMed] [Google Scholar]
- 5.Wunsch H, Mapstone J, Brady T, Hanks R, Rowan K. Hospital mortality associated with a day and time of admission to intensive care units. Intensive Care Med. 2004;30(5):895–901. doi: 10.1007/s00134-004-2170-3. [DOI] [PubMed] [Google Scholar]
- 6.Kuijsten HA, Brinkman S, Meynaar IA, Spronk PE, van der Spoel JI, Bosman RJ, et al. Hospital mortality is associated with ICU admission time. Intensive Care Med. 2010;36(10):1765–71. doi: 10.1007/s00134-010-1918-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tanio C. Weekend work: Balancing competing interests. J Gen Intern Med. 1999;14(1):66–7. doi: 10.1046/j.1525-1497.1999.00284.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cavallazi R, Marik PE, Hirani A, Pachinburavan M, Vasu TS, Leiby BE. Association between time of admission to the ICU and mortality: A systematic review and metaanalysis. Chest. 2010;138(1):68–75. doi: 10.1378/chest.09-3018. [DOI] [PubMed] [Google Scholar]
- 9.Obel N, Schierbeck J, Pedersen L, Storgaard M, Pedersen C, Sorensen HT, et al. Mortality after discharge from the intensive care unit during the early weekend period: A population-based cohort study in Denmark. Acta Anaesthesiol Scand. 2007;51(9):1225–30. doi: 10.1111/j.1399-6576.2007.01431.x. [DOI] [PubMed] [Google Scholar]
- 10.Duke DJ, Green JV, Briedis JH. Night-shift discharge from the intensive care unit increases the mortality-risk of ICU survivors. Anaesth Intensive Care. 2004;32(5):697–701. doi: 10.1177/0310057X0403200517. [DOI] [PubMed] [Google Scholar]
- 11.Wilcox ME, Chong CA, Niven DJ, Rubenfeld GD, Rowan KM, Wunsch H, et al. Do intensivist staffing patterns influence hospital mortality following ICU admission? A systematic review and meta-analyses. Crit Care Med. 2013;41(10):2253–74. doi: 10.1097/CCM.0b013e318292313a. [DOI] [PubMed] [Google Scholar]
- 12.Checkley W, Martin GS, Brown SM, Chang SY, Dabbagh O, Fremont RD, et al. Structure, process, and annual ICU mortality across 69 centers: United States Critical Illness and Injury Trials Group Critical Illness Outcomes Study. Crit Care Med. 2014;42(2):344–56. doi: 10.1097/CCM.0b013e3182a275d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hackner D, Shufelt CL, Balfe DD, Lewis MI, Elsayegh A, Braunstein GD, et al. Do faculty intensivists have better outcomes when caring for patients directly in a closed ICU versus consulting in an open ICU? Hosp Pract (1995) 2009;37(1):40–50. doi: 10.3810/hp.2009.12.253. [DOI] [PubMed] [Google Scholar]
- 14.Van der Sluis FJ, Slagt C, Liebman B, Beute J, Mulder JW, Engel AF. The impact of open versus closed format ICU admission practice on the outcome of high risk surgical patients: A cohort analysis. BMC Surg. 2011;11:18. doi: 10.1186/1471-2482-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhonagiri D, Pilcher DV, Bailey MJ. Increased mortality associated with after-hours and weekend admission to the intensive care unit: A retrospective analysis. Med J Aust. 2011;194(6):287–92. doi: 10.5694/j.1326-5377.2011.tb02976.x. [DOI] [PubMed] [Google Scholar]
- 16.Laupland KB, Misset B, Souweine B, Tabah A, Azoulay E, Goldgran-Toledano D, et al. Mortality associated with timing of admission to and discharge from ICU: A retrospective cohort study. BMC Health Serv Res. 2011;11:321. doi: 10.1186/1472-6963-11-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ensminger SA, Morales IJ, Peters SG, Keegan MT, Finkielman JD, Lymp JF, et al. The hospital mortality of patients admitted to the ICU on weekends. Chest. 2004;126(4):1292–8. doi: 10.1378/chest.126.4.1292. [DOI] [PubMed] [Google Scholar]
- 18.Vest-Hansen B, Riis AH, Sorensen HT, Christiansen CF. Out-of-hours and weekend admissions to Danish medical departments: Admission rate and 30-day mortality for 20 common medical conditions. BMJ Open. 2015;5:e006731. doi: 10.1136/bmjopen-2014-006731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sheu CC, Tsai JR, Hung JY, Yang CJ, Hung HC, Chong IW, et al. Admission time and outcome of patients in a medical intensive care unit. Kaohsiung J Med Sci. 2007;23(8):395–404. doi: 10.1016/S0257-5655(07)70003-2. [DOI] [PubMed] [Google Scholar]
- 20.Morales I, Peters SG, Afessa B. Hospital mortality rate and length of stay in patients admitted at night to the intensive care unit. Crit Care Med. 2003;31(3):858–63. doi: 10.1097/01.CCM.0000055378.31408.26. [DOI] [PubMed] [Google Scholar]
- 21.Lee KK, Ng I, Ang BT. Outcome of severe head injured patients admitted to intensive care during weekday shifts compared to nights and weekends. Ann Acad Med Singapore. 2008;37(5):390–6. [PubMed] [Google Scholar]
- 22.Abella A, Hermosa C, Enciso V, Torrejon I, Molina R, Diaz M, et al. Effect of the timing of admission upon patient prognosis in the intensive care unit: On-hours versus off-hours. Med Intensiva. 2016;40(1):26–32. doi: 10.1016/j.medin.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 23.Arabi Y, Alshimemeri A, Taher S. Weekend and weeknight admissions have the same outcome of weekday admissions to an intensive care unit with onsite intensivist coverage. Crit Care Med. 2006;34(3):605–11. doi: 10.1097/01.ccm.0000203947.60552.dd. [DOI] [PubMed] [Google Scholar]
- 24.Meynaar IA, van der Spoel JI, Rommes JH, van Spreuwel-Verheijen M, Bosman RJ, Spronk PE. Off hour admission to an intensivist-led ICU is not associated with increased mortality. Crit Care. 2009;13(3):R84. doi: 10.1186/cc7904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: Systematic review and meta-analysis. Med Care. 2007;45(12):1195–204. doi: 10.1097/MLR.0b013e3181468ca3. [DOI] [PubMed] [Google Scholar]
- 26.Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: A systematic review. JAMA. 2002;288(17):2151–62. doi: 10.1001/jama.288.17.2151. [DOI] [PubMed] [Google Scholar]
- 27.Wallace DJ, Angus DC, Barnato AE, Kramer AA, Kahn JM. Nighttime intensivist staffing and mortality among critically ill patients. N Engl J Med. 2012;366(22):2093–101. doi: 10.1056/NEJMsa1201918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blunt MC, Burchett KR. Out-of-hours consultant cover and case-mix-adjusted mortality in intensive care. Lancet. 2000;356(9231):735–6. doi: 10.1016/S0140-6736(00)02634-9. [DOI] [PubMed] [Google Scholar]
- 29.Gershengorn HB, Wunsch H, Wahab R, Leaf DE, Brodie D, Li G, et al. Impact of nonphysician staffing on outcomes in a medical ICU. Chest. 2011;139(6):1347–53. doi: 10.1378/chest.10-2648. [DOI] [PubMed] [Google Scholar]
- 30.Parshuram CS, Kirpalani H, Mehta S, Granton J, Cook D, et al. In-house, overnight physician staffing: A cross-sectional survey of Canadian adult and pediatric intensive care units. Crit Care Med. 2006;34(6):1674–8. doi: 10.1097/01.CCM.0000218808.13189.E7. [DOI] [PubMed] [Google Scholar]
- 31.Handman D, Bank M, Safford M. 24-hour in-house intensivists versus protocolized care in a surgical intensive care unit. Crit Care Med. 2004;32:A30. [Google Scholar]