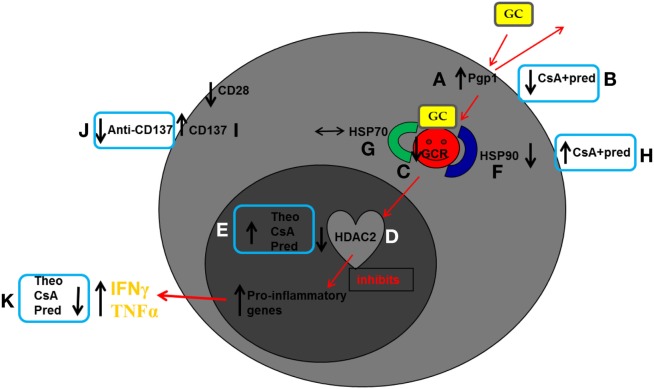
Figure 2.
Schematic diagram summarizing reported findings in peripheral blood CD8+CD28null natural killer T-like (NKT-like) cells in chronic obstructive pulmonary disease (COPD). Glucocorticoids enter cells by overcoming membrane drug efflux pump P-glycoprotein-1 (Pgp1) and binding to the glucocorticoid receptor (GCR) in the cytoplasm. GCR must be bound to the molecular chaperones heat shock protein (Hsp)70 and Hsp90 to acquire a high-affinity steroid binding conformation, and traffic to the nucleus where engagement of histone deacetylases (HDACs), particularly HDAC2, results in reduction of pro-inflammatory gene activation. In COPD compared with age-matched healthy control subjects: (A) Pgp1+ NKT-like cells are increased in COPD, reducing intracellular levels of GC. Expression of GCR (C), Hsp90 (F), and HDAC2 (D) are decreased in CD8+CD28null NKT-like cells (no change in Hsp70) (G) reducing steroid effectiveness. (I) The percentage of steroid resistant CD8+CD28nullCD137+ NKT-like cells is increased. Possible therapeutic targeting to overcome steroid resistance CD8+CD28null NKT-like cells in COPD: (B) Pgp1 is synergistically decreased in the presence of 2.5 ng/ml cyclosporine A (CsA) and 1µM prednisolone (pred). (H) Hsp90 expression is increased in the presence of 2.5 ng/ml CsA and 1µM pred. (E) HDAC2 expression is increased in the presence of 5 mg/ml theophylline, 2.5 ng/ml CsA, and 1µM pred. (J) Blocking CD137 expression with anti-CD137 antibody. (K) This targeting results in decreased IFNγ and TNFα pro-inflammatory cytokine expression.