Abstract
Purpose of the Study:
This study examines how certified nursing assistants (CNAs) balancing family caregiving roles—child care (double-duty child caregivers), elder care (double-duty elder caregivers), and both child and elder care (triple-duty caregivers)—utilize health care services relative to nonfamily caregiving counterparts (formal-only caregivers).
Design and Methods:
A sample of 884 CNAs from the Work, Family and Health Study was drawn on to assess the number of acute care (i.e., emergency room or urgent care facility) and other health care (i.e., outpatient treatment or counseling) visits made during the past 6 months.
Results:
Double-duty elder and triple-duty caregivers had higher acute care utilization rates than formal-only caregivers. CNAs with and without family caregiving roles had similar rates of other health care visits.
Implications:
CNAs providing informal care for older adults have higher acute care visit rates. Given the increasing need for family caregivers and the vital importance of the health of the nursing workforce for the health of others, future research on how double- and triple-duty caregivers maintain their health amidst constant caregiving should be a priority.
Key words: Combined caregiving roles, Family caregivers, Formal caregivers, Acute care, Health care visits
Certified nursing assistants (CNAs) constitute an essential occupation in the health care sector (Sweet, Pitt-Catsouphes, Besen, Hovhannisyan, & Pasha, 2010). According to the Bureau of Labor Statistics (BLS), these health care employees are considered primary caregivers and provide basic care for patients in hospitals and residents of long-term care facilities, such as nursing homes. Given their engagement in hands-on care and more frequent contact with patients than other nursing staff, CNAs are generally highly active, balance heavy workloads, and perform physically demanding tasks (Bureau of Labor Statistics [BLS], 2014). Consequently, CNAs are at significant risk of on-the-job injuries, with nonfatal injury and illness rates in the 98th and 99th percentile for all occupations in 2007 (Bureau of Labor Statistics [BLS], 2014; Khatutsky, Wiener, Anderson, & Porell, 2012; Sweet et al., 2010). Despite such risks, CNA employment is expected to grow 21% from 2012 to 2022 to keep pace with accelerated population aging and the need for long-term care (Bureau of Labor Statistics [BLS], 2014). The health care industry has thus been tasked with meeting an increasing demand for services, coupled with retaining and accommodating an aging workforce susceptible to injury and illness (Harrington & Heidkamp, 2013).
In addition to challenging an under-resourced health care system, rapid populating aging has led to a concurrent, unprecedented need for family caregivers (Harrington & Heidkamp, 2013; St-Amant et al., 2014). Prior research suggests that adults who combine paid, formal caregiving in the health care sector with unpaid, informal caregiving in their “off” time are increasingly prevalent in the health care industry (Boumans & Dorant, 2014; DePasquale et al., 2014; Ward-Griffin et al., 2015). In the literature, the occupation of informal caregiving roles for dependent children (i.e., double-duty child caregiving) or adult relatives (i.e., double-duty elder caregiving) by practicing health care professionals is called double-duty caregiving whereas the occupation of informal caregiving roles for sandwiched care recipients, or dependent children and adult relatives, among such professionals is considered triple-duty caregiving. Double- and triple-duty caregiving are relevant for the health care industry for complementary reasons. First, double- and triple-duty caregiving are associated with a range of health-related problems, including extreme physical and emotional exhaustion, physical and mental fatigue, strain, stress, anxiety, and psychological distress (Boumans & Dorant, 2014; DePasquale et al., 2014; Scott, Hwang & Rogers, 2006; Ward-Griffin, Brown, Vandervoort, McNair, & Dashnay, 2005). Double- and triple-duty caregivers also have an increased risk of compassion fatigue, a condition specific to caregiving that negatively affects well-being as a result of direct, prolonged exposure, and over identification with care recipients’ suffering (Ward-Griffin, St-Amant, & Brown, 2011). Further, as double-duty elder caregivers provide more hours of informal care they report a greater need to recuperate from work-related efforts and are more likely to exhibit presenteeism, or attend work while ill (Boumans & Dorant, 2014). Nurses’ presenteeism is particularly troubling given its link to more patient falls, medication errors, and health care costs as well as lower quality of care (Letvak, Ruhm, & Gupta, 2012).
Second, double- and triple-duty caregivers’ health and work–life balance affects care recipients’ well-being. For instance, a previous study found that the likelihood of making medication-related, charting, or transcription mistakes at work was more than doubled for hospital staff nurses occupying an informal elder care role (i.e., double-duty elder caregivers) compared to nonfamily caregiving counterparts (Scott et al., 2006). The authors attributed poorer work performance to sleep deprivation, as double-duty elder caregivers also reported the shortest average sleep duration on work days. Indeed, prior research indicates that sleep deprivation among nurses, a significant and prevalent occupational health issue in the nursing profession, adversely impacts health, judgment, and performance, leading to errors and accidents that jeopardize patient safety (Surani, Murphy, & Shah, 2007). Additionally, double- and triple-duty caregivers experience more work–family conflict than nonfamily caregiving counterparts (Boumans & Dorant, 2014; DePasquale et al., 2014). Nurses’ work–family conflict is linked to lower job satisfaction (Cortese, Colombo, & Ghislieri, 2010), greater job stress (Farhadi, Sharifian, Feili, & Shokrpour, 2013), emotional exhaustion (Leineweber et al., 2014), poorer psychological health (Rantanen et al., 2013), and physical pain (Kim et al., 2013). These same outcomes, in turn, are associated with poorer work performance (Wang & Tsai, 2014) and occupational mistakes (Pani & Chariker, 2004). Thus, double- and triple-duty caregivers’ work–family conflict may hinder their ability to provide quality care.
Collectively, findings from prior double- and triple-duty caregiving research demonstrate a need for health-promoting behaviors among this population not only for the preservation of their own health, but for care recipients’ health as well. To date, however, no studies have examined a critical aspect of double- and triple-duty caregiver health—use of health care services. Therefore, the objective of this study was to conduct an exploratory investigation of health care utilization among CNAs working in nursing homes in the United States, the majority of whom occupy double- and triple-duty caregiving roles, by addressing the following questions:
1. How do double- and triple-caregiving role occupancy, compared to formal-only caregiving (i.e., CNAs without family caregiving obligations), relate to health care utilization?
2. What factors are associated with CNAs’ health care utilization?
3. Are double-and triple-duty caregiving role occupancy uniquely associated with health care utilization beyond the effects of other factors?
Theoretical Framework
Given our proposed exploration of factors associated with CNAs’ health care utilization, we draw on the Andersen and Newman (1973) Behavioral Model of Health Services Use to inform variable selection. The Andersen and Newman model views health care utilization as an individual behavior resulting from three sets of contextual factors: (a) predisposing; factors that exist prior to illness onset, (b) enabling; the means by which health care services can be accessed when needed, and (c) need; perceived or clinician-evaluated health status and functioning. The Andersen and Newman model has previously been tested in family caregiving research to identify predictors of health care utilization, but has never been applied to CNAs occupying different family caregiving roles. Our study therefore provides the first empirical test of the model with this population.
Design and Methods
Study Design
This study is part of a multidisciplinary research initiative by the Work, Family and Health Network (WFHN), an organization formed by the National Institutes of Health (NIH) and the Centers for Disease Control and Prevention (CDC), to enhance understanding of the ways in which workplace practices and policies affect work, family, and health outcomes among employees working in different industries (see Bray et al., 2013; King et al., 2012).
Research Site
The WFHN mailed letters to several large health care companies to recruit partners for research participation. Potential partners were asked a standard set of questions to ensure fulfillment of minimum requirements for study participation. These requirements included basic information about the company (e.g., number of employees working in the United States), its background (e.g., competing initiatives), employees (e.g., demographics), and relationship with management (e.g., willingness to participate). The WFHN ultimately became corporate partners with a long-term health and specialized care company managing 56 worksites in New England. With guidance from the company’s Vice President of Development, the WFHN selected 30 nursing home facilities for study participation. Inclusion criteria for consideration included size (< 30 nursing staff), how recently the site was acquired (if relevant), stable management structure (i.e., minimal turnover), location in a nonisolated setting, and no other research participation. None of the facilities declined participation and one facility was excluded for participation in competing initiatives.
Sample
Eligible employees worked at least 22.5hr per week in direct care on day or evening shifts. Nightshift workers were excluded given the logistical challenges of scheduling in-person interviews as well as fundamental differences between day and nightshift workers (e.g., nightshift employees work on skeleton crews while residents are sleeping). Of 1,783 eligible employees, 1,524 (85%) enrolled in the Work, Family and Health Study (WFHS), 1,025 of whom were CNAs and comprise the focus of this study.
Procedures
Trained field interviewers administered computer-assisted personal interviews at a private location in the workplace. Employees provided information about sociodemographics, family relationships, work environment, health, and health behaviors. Interviews averaged 60min and employees received compensation for their time. Detailed information regarding the WFHS protocol is described elsewhere (Bray et al., 2013; King et al., 2012).
Measures
Outcomes
Health care utilization was operationalized as the number of acute care and other health care visits CNAs reported making for personal reasons/themselves in the past 6 months. Specifically, acute care pertained to emergency room or urgent care treatment facility visits for health treatment (range = 0–15, M = 0.37, SD = 0.93) whereas other health care visits reflected the receipt of outpatient treatment or counseling from health care professionals (range = 0–76, M = 1.49, SD = 5.27).
Predictors
We categorized CNAs into four mutually exclusive groups based on family caregiving role occupancy (DePasquale et al., 2014, 2015; Scott et al., 2006; Tement & Korunka, 2015). Double-duty child caregivers had children 18 years of age or younger living with them for at least 4 days per week. Double-duty elder caregivers provided care (i.e., assistance with shopping, medical care, or financial/budget planning) for at least 3hr per week in the past 6 months to an adult relative, regardless of residential proximity. Triple-duty caregivers were identified through endorsement of both child and adult care criteria. Formal-only caregivers did not indicate any family caregiving obligations and constituted the reference group.
To test the Andersen and Newman model (1973), we identified multiple indicators of predisposing, enabling, and need factors that may affect CNAs’ health care utilization. Classification of contextual factors was guided by the model and a review of its application in family caregiving studies (e.g., Bergman, Haley, & Small, 2011; Bookwala et al., 2004; Cox, 1997; Cox, 1999; Herrera, Lee, Palos, & Torres-Vigil, 2008; Kosloski & Montgomery, 1994; Robinson, Buckwalter, & Reed, 2005; Toseland, McCallion, Gerber, & Banks, 2002). The model components and respective variables are summarized and presented in Table 1.
Table 1.
Certified Nursing Assistants’ Characteristics by Family Caregiving Role Occupancy
| Conditions | Overall (n = 884) | Formal-only care (n = 317) | Double-duty child care (n = 302) | Double-duty elder care (n = 138) | Triple-duty care (n = 127) |
|---|---|---|---|---|---|
| Predisposing characteristics | |||||
| Age | 36.75 (13) | 39.24 (15)c,t | 33.55 (9) | 40.33 (14) | 34.26 (9) |
| Female | 0.91 | 0.87c,t | 0.95 | 0.90 | 0.95 |
| White | 0.66 | 0.68 | 0.66 | 0.70 | 0.61 |
| Some college or more | 0.47 | 0.51 | 0.43 | 0.47 | 0.45 |
| Cohabiting or married | 0.58 | 0.52c,t | 0.65 | 0.51 | 0.65 |
| Hours worked per week | 36.36 (7) | 36.59 (7) | 36.01 (6) | 36.91 (6) | 36.04 (8) |
| Enabling characteristics | |||||
| $34,999 or less | 0.44 | 0.41 | 0.49 | 0.35 | 0.50 |
| $35,000–59,999 | 0.40 | 0.41 | 0.37 | 0.49 | 0.39 |
| More than $60,000 | 0.16 | 0.19 | 0.14 | 0.17 | 0.12 |
| Eligible, employer health insurance | 0.40 | 0.29c,t | 0.52 | 0.30 | 0.51 |
| Enrolled, employer health insurance | 0.49 | 0.60c,t | 0.37 | 0.64 | 0.33 |
| Need characteristics | |||||
| High blood pressure | 0.22 | 0.23 | 0.21 | 0.26 | 0.20 |
| Cancer | 0.04 | 0.04 | 0.03 | 0.04 | 0.03 |
| Diabetes | 0.08 | 0.08 | 0.07 | 0.11 | 0.09 |
| Psychological distress | 12.33 (5) | 11.63 (4)e,t | 12.19 (4) | 12.88 (5) | 13.78 (5) |
| Psychological job demands | 3.75 (0.7) | 3.59 (0.7)c,e,t | 3.79 (0.7) | 3.90 (0.7) | 3.92 (0.8) |
| Work-related injury | 0.22 | 0.20 | 0.18 | 0.26 | 0.28 |
| Sleep duration | 6.09 (1) | 6.27 (1)c | 5.95 (1) | 6.16 (2) | 5.92 (1) |
| Body mass index | 29.59 (7) | 29.73 (7) | 28.85 (7) | 30.61 (7) | 29.86 (7) |
| Smoker | 0.32 | 0.27c | 0.38 | 0.30 | 0.32 |
| Disabled child | 0.10 | — | 0.18 | — | 0.28 |
Notes: Means (and standard deviations) or proportions are shown. Annual household income is shown as a categorical variable for the purposes of this table only. ANOVAs with Tukey post-hoc comparison tests were conducted to identify mean differences across groups, with formal-only care as the reference group. Subscript letters denote significant differences between formal-only caregivers and family caregiving groups: c = double-duty child care, e = double-duty elder care, t = triple-duty care.
Predisposing
We examined the following predisposing factors: age (in years), gender (0 = male, 1 = female), race/ethnicity (0 = non-Hispanic White, 1 = White), educational attainment (0 = high school degree or less, 1 = some college or more), marital status (0 = single, 1 = cohabiting or married), and average number of hours worked per week.
Enabling
We included the enabling factors of annual household income and health insurance status, as both variables are considered caregiver resources in accessing health care services (Hinrichsen & Ramirez, 1992; Toseland et al., 2002). Annual household income was measured on an ordinal scale ranging from 1 (less than $4,999) to 13 ($60,000 or more). For health care insurance status, we created dichotomous variables to represent CNAs ineligible for employer health insurance (reference group), eligible but not enrolled, or eligible and enrolled.
Need
Given that chronic health condition status is positively associated with family caregivers’ health care utilization (Baumgarten et al., 1997; Perlick et al., 2005), we included self-reported clinical diagnoses of high blood pressure, cancer, and diabetes under the “ever been told” question stem (0 = no, 1 = yes). We also examined indicators of psychological well-being, as previous studies have highlighted their importance in predicting service utilization (Bergman et al., 2011; Bookwala et al., 2004; Cox, 1997; Perlick et al., 2005; Schubert et al., 2008; Son et al., 2007). Specifically, we assessed nonspecific psychological distress and psychological job demands (Williams, 2013). Psychological distress was measured with the Kessler-6 scale (Kessler et al., 2003) which includes six items (e.g., “How much of the time did you feel hopeless?”) pertaining to the past 30 days (α = 0.84); response options ranged from none of the time (1) to all of the time (5). We summed item responses to compute a composite distress score; higher scores reflect greater distress. Karasek et al.’s (1998) Job Content Questionnaire measured psychological job demands (α = 0.59). CNAs rated their level of agreement with three items (e.g., “My job requires very fast work”) on a 5-point scale (1 = strongly agree, 5 = strongly disagree). We reverse-coded all items so that higher scores reflect greater job demands and averaged responses. Additionally, we incorporated work-related injuries in the past 6 months (0 = no, 1 = yes), average sleep duration, body mass index (BMI), and current smoker status (0 = no, 1 = yes), each of which may exacerbate or contribute to the development of health problems. Further, because the severity of child health problems or disability is positively related to parents’ health care utilization (Damiani, Rosenbaum, Swinton, & Russell, 2004), we accounted for dependent children with developmental disabilities, physical health problems, or long-term, serious mental health problems.
Analytic Strategy
To ensure a consistent sample across analyses, we excluded participants with missing data on any of the aforementioned measures (n = 141), thereby resulting in a final analytic sample of 884 CNAs. As commonly found in health care utilization literature, acute care and other health care visits represented non-negative integer count variables characterized by non-normal distributions and overdispersion (i.e., skewed and clustered at zero). We therefore modeled our outcomes with negative binomial regressions (Hilbe, 2007). We accounted for clustering of CNAs within nursing homes by obtaining robust standard errors via the repeated statement (Huber-White correction) in the PROC GENMOD procedure in SAS 9.4. We estimate two separate models per outcome. Model 1 addresses Research Question (RQ) 1 by examining health care utilization among double- and triple-duty caregivers relative to formal-only caregivers. Model 2 addresses RQ2 and RQ3 by adding predisposing, enabling, and need predictors. We report incident rate ratios (IRR) for all models.
Results
Descriptive Analyses
Table 1 presents sample characteristics by family caregiving role occupancy. ANOVA analyses indicate that family caregiving role occupancy is related to age, gender, marital status, health insurance status, psychological distress and job demands, sleep duration, and smoker status. Specifically, the formal-only caregiving group, on average, was older, included fewer females and cohabiting or married CNAs, and reported higher enrollment in employer health insurance than the double-duty child and triple-duty caregiving groups. Additionally, the formal-only caregiving group, on average, reported longer sleep duration as well as included fewer smokers relative to the double-duty child caregiving group, and had lower psychological distress scores than the double-duty elder and triple-duty caregiving groups. The formal-only caregiving group also reported lower psychological job demands, on average, than each double- and triple-duty caregiving group.
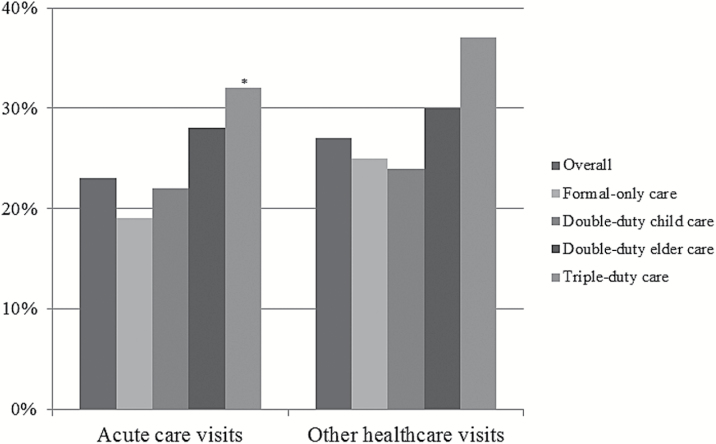
Figure 1 provides a graphical depiction of the prevalence of health care utilization among CNAs. Overall, 23% and 27% of CNAs made at least one acute care and other health care visit in the past 6 months, respectively. Formal-only caregivers had the lowest prevalence of acute care utilization (19%) whereas triple-duty caregivers had the highest (32%); this difference was statistically significant (p < .05). Further, the prevalence of other health care visits was lowest among double-duty child caregivers (24%) and highest for triple-duty caregivers (37%).
Figure 1.
Prevalence of acute care and other health care visits among certified nursing assistants. Figure depicts the proportion of certified nursing assistants who made one or more acute care and other healthcare visits in the past six months overall and by family caregiving role occupancy. ANOVAs with Tukey post-hoc comparison tests were conducted to identify differences across groups, with formal-only care as the reference group. Statistically significant group differences denoted as *p < .05, **p < .01, ***p < .001.
Multivariate Analyses
RQ1: Double- and Triple-Duty Caregiving
In Model 1, double-duty elder and triple-duty caregiving were associated with higher acute care visit rates than Formal-only caregiving (Table 2). Specifically, acute care visit rates were 2.12 and 2.40 times greater for double-duty elder and triple-duty caregivers, respectively. Double- and triple-duty caregiving roles did not predict other health care visits.
Table 2.
Incident Rate Ratios From Negative Binomial Regression Models Predicting Health Care Utilization Visit Rates Among Certified Nursing Assistants
| Acute care visits | Other health care visits | |||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |
| IRR (SE) (95% CI) | IRR (SE) (95% CI) | IRR (SE) (95% CI) | IRR (SE) (95% CI) | |
| Double-duty child care | 1.34 (0.20) (0.91–1.98) | 1.14 (0.23) (0.72–1.80) | 0.65 (0.26) (0.39–1.08)† | 0.77 (0.26) (0.46–1.29) |
| Double-duty elder care | 2.12 (0.27) (1.25–3.61)** | 1.91 (0.27) (1.11–3.27)* | 0.79 (0.35) (0.40–1.57) | 1.03 (0.30) (0.57–1.85) |
| Triple-duty care | 2.40 (0.19) (1.65–3.50)*** | 1.77 (0.25) (1.09–2.88)* | 1.46 (0.23) [0.93–2.29)† | 1.51 (0.27) (0.90–2.54) |
| Predisposing characteristics | ||||
| Age | 0.98 (0.01) (0.97–1.00)† | 1.00 (0.01) (0.98–1.01) | ||
| Female | 1.36 (0.29) (0.76–2.42) | 0.96 (0.25) (0.58–1.58) | ||
| White | 0.86 (0.18) (0.61–1.22) | 1.42 (0.22) (0.93–2.17) | ||
| Some college or more | 1.18 (0.18) (0.82–1.69] | 1.31 (0.17) (0.94–1.82) | ||
| Cohabiting or married | 0.89 (0.21) (0.59–1.36) | 1.59 (0.17) (1.13–2.24)** | ||
| Hours worked per week | 1.00 (0.01) (0.98–1.02) | 0.99 (0.02) (0.95–1.02) | ||
| Enabling characteristics | ||||
| Income | 0.98 (0.03) (0.93–1.04) | 0.94 (0.03) (0.88–1.01)† | ||
| Eligible, health insuranceb | 1.17 (0.17) (0.83–1.64) | 1.00 (0.18) (0.70–1.44) | ||
| Enrolled, health insuranceb | 0.94 (0.19) (0.65–1.36) | 0.82 (0.21) (0.54–1.25) | ||
| Need characteristics | ||||
| High blood pressure | 1.10 (0.17) (0.78–1.54) | 1.51 (0.17) (1.08–2.10)* | ||
| Cancer | 2.23 (0.27) (1.31–3.78)** | 4.82 (0.60) (1.48–15.71)** | ||
| Diabetes | 1.20 (0.26) (0.73–1.98) | 0.77 (0.32) (0.41–1.44) | ||
| Psychological distress | 1.02 (0.02) (0.98–1.05) | 1.05 (0.02) (1.01–1.09)* | ||
| Psychological job demands | 1.40 (0.08) (1.20–1.64)*** | 1.38 (0.13) (1.08–1.77)* | ||
| Work-related injurya | 1.48 (0.23) (0.94–2.33)† | 1.85 (0.25) (1.13–3.02)* | ||
| Sleep duration | 1.02 (0.07) (0.89–1.17) | 0.93 (0.07) (0.81–1.07) | ||
| Body mass index | 1.01 (0.01) (0.99–1.03) | 1.01 (0.01) (0.98–1.04) | ||
| Current smoker | 1.26 (0.17) (0.91–1.75) | 0.84 (0.20) (0.56–1.24) | ||
| Disabled child | 1.14 (0.25) (0.70–1.88) | 1.92 (0.33) (1.00–3.68)* | ||
| Overdispersion parameter | 2.30 (0.37) (1.69–3.15) | 1.81 (0.31) (1.29–2.54) | 7.88 (0.66) (6.68–9.29) | 6.64 (0.58) (5.60–7.88) |
| N | 884 | |||
Notes: IRR = incident rate ratio. The overdispersion parameter (or alpha) for each model has a 95% confidence interval that does not include zero, indicating that the negative binomial regression model is more appropriate than the Poisson. An estimate greater than zero suggests overdispersion. All continuous variables are centered.
aWork-related injury is a dichotomous indicator referring to the past 6 months.
bHealth insurance refers to employer health insurance.
†p ≤. 10, *p ≤ .05, **p ≤ .01, ***p ≤ .001.
RQ2: Contextual Factors
Among predisposing factors, only marital status was associated with health care utilization, such that cohabiting or married CNAs had higher rates of other health care visits. With regard to enabling factors, neither health insurance status nor income predicted health care utilization. Across outcomes, however, the need factors of self-reported cancer diagnosis and psychological job demands predicted higher visit rates. Further, the need factors of self-reported high blood pressure, psychological distress, work-related injury, and living with a disabled child were linked to higher rates of other health care visits.
RQ3: Unique Relationships
Although attenuated, the associations between double-duty elder and triple-duty caregiving and acute care visits persisted after adding predisposing, enabling, and need factors in Model 2. Double-duty elder and triple-duty caregivers had 91% and 77% higher visit rates, respectively. Double- and triple-duty caregiving role occupancy remained nonsignificant predictors of other health care visits.
Discussion
Greater understanding of work–family pressures is a key action step for the health care sector as it reforms workplace practices to keep pace with population aging (Harrington & Heidkamp, 2013; Sweet et al., 2010). Double- and triple-duty caregiving constitute significant, yet overlooked, work–family pressures experienced by a growing number of health care workers. Although prior research has highlighted the adverse effects of double- and triple-duty caregiving (Boumans & Dorant, 2014; DePasquale et al. 2015; Scott et al., 2006), we are unaware of any studies that assess health care utilization among this population. Thus, our study is the first to empirically test the Andersen and Newman (1973) model as a scientific framework for understanding the role of contextual factors in acute care and other health care visit rates among CNAs simultaneously occupying family caregiving roles.
In addressing RQ1, we found that double-duty elder and triple-duty caregivers had higher rates of acute care utilization than formal-only caregivers; conversely, double- and triple-duty caregivers and formal-only caregivers had similar rates of other health care visits. RQ2 aimed to identify factors associated with CNAs’ health care utilization. Guided by the Andersen and Newman (1973) model and its previous applications in family caregiving research, we organized factors that may affect CNAs’ health care utilization into predisposing, enabling, and need characteristics. Overall, predisposing and enabling factors had few effects on health care utilization. Instead, the need component represented the only set of determining variables associated with CNAs’ acute care utilization and was most pertinent for other health care visits. Although it has been suggested that predisposing and enabling factors may be as important as need factors in predicting family caregivers’ health care utilization (Toseland et al., 2002), our findings are congruent with a number of family caregiving studies that demonstrate the significance of need variables (Bergman et al., 2011; Bookwala et al., 2004; Cox, 1997). Further, need factors may be a more salient contextual factor for CNAs than family caregivers because of their professional status. That is, predisposing and enabling factors may not have the same impact given CNAs’ specialized health care training or expertise, knowledge of available health care service options, familiarity in navigating the health care system, and health care connections (Ward-Griffin et al., 2005). Our results are also consistent with prior literature in that the significance of variables measuring contextual factors generally differed depending on the type of health care service under consideration (Toseland et al., 2002).
With regard to RQ3, double- and triple-duty caregiving role occupancy were uniquely related to acute care utilization beyond the effects of contextual factors. One possible explanation for our findings is that, despite the negative health effects of double-duty elder and triple-duty caregiving (Boumans & Dorant, 2014; DePasquale et al., 2014; Scott et al., 2006; Ward-Griffin et al., 2005) and likely high need for health care services among this population, providing informal care for older adults constitutes a barrier to more routine health care utilization. A similar notion was proposed by Baumgarten et al. (1997) after finding that use of physician services was no greater for dementia caregivers than noncaregivers even though caregivers had poorer overall health. Baumgarten et al. hypothesized that commitment of time and energy to informal elder care prevented caregivers from addressing their own health concerns. Indeed, qualitative research suggests that health care professionals informally caring for adult relatives are typically responsible for a wide range of activities, such as providing hands-on care, making care-related decisions, delegating tasks, overseeing professional care, and advocating for care recipients (Giles & Hall, 2014; St-Amant et al., 2014; Ward-Griffin et al., 2005). These responsibilities, all of which are completed in addition to formal caregiving, detract from time and energy otherwise allotted to maintaining one’s own health. Further, as care recipient needs grow more complex, double- and triple-duty caregivers’ care provision likely intensifies. If double- and triple-duty caregivers forgo or postpone their own health needs to fulfill increasing informal care demands, they may exacerbate preexisting illnesses or work-related injuries and amplify stress vulnerability. Consequently, critical need factors may prompt double-duty elder and triple-duty caregivers to seek health care services at a point in which acute care is necessary.
Two other explanations adapted from Baumgarten et al. (1997), selection bias and self-reliance, facilitate interpretation of results from this study. First, CNAs’ health care utilization patterns may reflect selection forces. For example, 27% of CNAs in the WFHS sample made at least one other health care visit in the past 6 months whereas, according to the 2012 National Health Interview Survey (NHIS), approximately 80% of individuals 18 years or older made at least one visit in the past year (Blackwell, Lucas, & Clarke, 2014). In addition to being relatively younger than NHIS participants, CNAs in the WFHS are all employed. Employment implies that CNAs are capable of successfully adopting as well as maintaining a physically and psychologically demanding work role. Individuals who frequently require health care services or are in poor health likely do not select into a formal caregiving occupation; if they do, they may be more likely to exit the role. Relatedly, selection forces may be particularly applicable to double- and triple-duty caregivers in that they must be in good health to balance multiple caregiving role occupancy and fulfill accompanying role demands. Second, formal caregiving may enhance self-reliance and reduce perceived need or desire for health care services. As health professionals, CNAs may rely on their own training or expertise to address personal health concerns or engage in self-care tactics that would otherwise prompt lay persons to make nonemergency health care visits. The additional responsibilities associated with providing informal care to adult relatives, however, may motivate double-duty elder and triple-duty caregiving CNAs to seek health care services when health problems are serious or exceed their abilities, two health scenarios that likely require acute care.
Moreover, adult care recipients’ unpredictable care needs (Hessel & Keck, 2009) and familial pressure (Ward-Griffin et al., 2005) may affect health care utilization patterns. In anticipation of changes in adult relatives’ health, CNAs may be hesitant to ask for or make work accommodations to manage their own health needs during the work day. Rather, they may reserve these options for unexpected care recipient events to avoid exhausting safeguards and sacrificing earnings. Although speculative, this explanation implies that double-duty elder and triple-duty caregivers resort to acute care for their own health purposes, are strategic in their use of workplace supports, and exhibit presenteeism. Additionally, double-duty elder and triple-duty caregivers may feel that they cannot plan or partake in routine health care visits for themselves as others are relying on them to prioritize informal care. Indeed, qualitative evidence indicates that double-duty elder caregivers prioritize care recipients’ needs and place unrealistic expectations upon themselves to be a model family member (Giles & Hall, 2014; Ward-Griffin, 2004; Ward-Griffin et al., 2005). Therefore, acute care may represent a convenient health care service that permits double- and triple-duty caregivers more control amidst uncertainty arising from family caregiving roles.
Limitations and Future Directions
This study has several limitations. First, the cross-sectional design precludes causal ordering and exploration of the dynamic qualities of the constructs examined. Second, health care utilization measures were based on subjective, retrospective reports that may be subject to recall bias. Third, CNAs worked in health care facilities in New England, thereby limiting generalizability. Finally, we conducted a secondary analysis of existing data not specifically designed to study caregiving. Though the data lacked ideal information regarding caregiving intensity, it enabled us to construct proxy measures of family caregiving role occupancy consistent with prior research (DePasquale et al., 2014; DePasquale et al., 2015; Scott et al., 2006; Tement & Korunka, 2015). Still, it should be acknowledged that this approach operationalizes child and adult care differently. Specifically, the child care measure does not assess actual care provision; instead, dependency is implied by age (i.e., under 18) and cohabitation. However, the average age of children (6.51 and 7.85 for double-duty child and triple-duty caregivers, respectively) supports the notion that child care recipients in the WFHS sample were dependent. Conversely, adult care specifies criteria for care provision; this criteria is more stringent than the 1hr time commitment required in prior double-duty care research (Gottlieb, Kelloway, & Martin-Matthews, 1996; Ward-Griffin, 2004). It should also be noted that, although we use the term double-duty elder care, this measure may encompass care for adult relatives other than aging parents, such as spouses or siblings in midlife. Nonetheless, a sample drawn from a working population is advantageous in that it may be more representative of double- and triple-duty caregivers than a sample selected for a certain threshold of care or care recipient illness (DePasquale et al., 2014; DePasquale et al., 2015). Additionally, although family caregiving experiences likely vary within the WFHS sample, the employment role is constant. Thus, family caregiving role occupancy distinguishes double- and triple-duty caregiving CNAs from formal-only caregivers.
The aforementioned limitations should not outweigh the contributions and knowledge gained from this study. We bring attention to and advance understanding of a unique and understudied population. Traditionally, researchers have studied formal and informal caregiving separately instead of considering the implications of their intersection (Ward-Griffin et al., 2015). Understandably, then, previous studies on double- and triple-duty caregiving comprise a small, limited body of research characterized by qualitative evidence, relatively small samples of registered nurses or health professionals working outside of the United States, and a sole focus on double-duty elder care (Boumans & Dorant, 2014; Giles & Hall, 2014; Ross, Rideout, & Carson, 1996; Rutman, 1996; Scott et al., 2006; St-Amant et al., 2014; Ward-Griffin, 2004; Ward-Griffin et al., 2005; Ward-Griffin et al., 2011; Ward-Griffin et al., 2015). We contribute to this existing literature by focusing on a large CNA population working in nursing homes in the United States, accounting for different informal caregiving roles, and providing novel empirical evidence regarding health care utilization, an outcome not previously examined among double- and triple-duty caregivers. An additional strength is our extension of the application of the Andersen and Newman (1973) framework.
Thus, our investigation serves as an essential baseline and lays the groundwork for prospective explorations of health care utilization among double- and triple-duty caregivers. It is important that our findings be viewed as an initial step toward identifying the prevalence and predisposing, enabling, and need correlates of health care utilization among double- and triple-duty caregivers, and that they be replicated with more representative samples, longitudinal research designs, and further expansion of the Andersen and Newman (1973) model. For instance, only one care recipient characteristic (i.e., child disability) was available when applying the model to WFHS data. Future studies employing the Andersen and Newman framework should integrate care recipients’ predisposing, enabling, and need characteristics to examine how each contributes to caregiver health care utilization. Similarly, integration of other subcomponents of individual determinants, such as attitudes or beliefs about health care utilization, and inclusion of societal determinants (e.g., health system resources) may enhance the model’s explanatory power (Andersen & Newman, 1973). Moreover, whereas this study simultaneously examined contextual factors, longitudinal studies can test the causal ordering of relationships hypothesized within the model (Andersen, 1995). In addition to model expansions, prospective research assessing health behavior engagement, self-care strategies, and other types of health care services is warranted. Further, because health care utilization may be delayed until an urgent health problem arises, data on the timing of and reasoning for health care visits will be particularly informative. As important, studies that acquire information regarding caregiving intensity as well as health information about or from care recipients can be used to examine concordance between care recipient events and caregiver health care utilization. Qualitative studies in which double- and triple-duty caregivers discuss perceived barriers, facilitators, and life or health events in relation to health care utilization may complement such efforts. Lastly, the availability, use, and relevance of workplace practices, programs, and policies for double- and triple-duty caregivers’ health care needs represent a pivotal direction for future research.
Conclusion
Independent of predisposing, enabling, and need factors specified in the Andersen and Newman (1973) framework, double-duty elder and triple-duty caregivers had higher acute care visit rates than formal-only caregivers. Given that their welfare is critically important for the well-being of others, additional research on how double- and triple-duty caregivers maintain their health amidst the challenges of constant caregiving is necessary.
Funding
This research was conducted as part of the Work, Family and Health Network (www.WorkFamilyHealthNetwork.org), which is funded by a cooperative agreement through the National Institutes of Health and the Centers for Disease Control and Prevention: Eunice Kennedy Shriver National Institute of Child Health and Human Development (U01HD051217, U01HD051218, U01HD051256, U01HD051276), National Institute on Aging (U01AG027669), Office of Behavioral and Social Sciences Research, and National Institute for Occupational Safety and Health (U01OH008788, U01HD059773). Grants from the William T. Grant Foundation, Alfred P Sloan Foundation, and the Administration for Children and Families have provided additional funding.
Acknowledgements
The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of these institutes and offices. Special acknowledgement goes to Extramural Staff Science Collaborator, Rosalind Berkowitz King, PhD, and Lynne Casper, PhD, for design of the original Workplace, Family, Health and Well-Being Network Initiative. We also wish to express our gratitude to the worksites, employers, and employees who participated in this research.
References
- Andersen R., & Newman J. F (1973). Societal and individual determinants of medical care utilization in the United States. The Milbank Memorial Fund Quarterly, 51, 95–124. doi:10.1111/j.1468-0009.2005.00428.x [PubMed] [Google Scholar]
- Andersen R. M. (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, 36, 1–10. doi:10.2307/2137284 [PubMed] [Google Scholar]
- Baumgarten M. Battista R. N. Infante-Rivard C. Hanley J. A. Becker R. Bilker W. B., & Gauthier S (1997). Use of physician services among family caregivers of elderly persons with dementia. Journal of Clinical Epidemiology, 50, 1265–1272. doi:10.1016/S0895-4356(97)00168-6 [DOI] [PubMed] [Google Scholar]
- Bergman E. J. Haley W. E., & Small B. J (2011). Who uses bereavement services? An examination of service use by bereaved dementia caregivers. Aging & Mental Health, 15, 531–40. doi: 10.1080/13607863.2010.543661 [DOI] [PubMed] [Google Scholar]
- Blackwell D. L. Lucas J. W., & Clarke T. C (2014). Summary health statistics for US adults: National Health Interview Survey, 2012. Vital and Health Statistics, 10, 1–161. [PubMed] [Google Scholar]
- Bookwala J. Zdaniuk B. Burton L. Lind B. Jackson S., & Schulz R (2004). Concurrent and long-term predictors of older adults’ use of community-based long-term care services: The Caregiver Health Effects Study. Journal of Aging and Health, 16, 88–115. doi:10.1177/0898264303260448 [DOI] [PubMed] [Google Scholar]
- Boumans N. P. G., & Dorant E (2014). Double-duty caregivers: Healthcare professionals juggling employment and informal caregiving. A survey on personal health and work experiences. Journal of Advanced Nursing, 70, 1604–1615. doi:10.1111/jan.12320 [DOI] [PubMed] [Google Scholar]
- Bray J. W. Kelly E. L. Hammer L. B. Almeida D. M. Dearing J. W. King R. B., & Buxton O. M (2013). An integrative, multilevel, and transdisciplinary research approach to challenges of work, family, and health. Research Triangle Park, NC: RTI Press. [PubMed] [Google Scholar]
- Bureau of Labor Statistics (2014). Occupational Outlook Handbook, 2014–15 Edition. Nursing Assistants and Orderlies. Retrieved from http://www.bls.gov/ooh/healthcare/nursing-assistants.htm. [Google Scholar]
- Cortese C. G. Colombo L., & Ghislieri C (2010). Determinants of nurses’ job satisfaction: The role of work-family conflict, job demand, emotional charge and social support. Journal of Nursing Management, 18, 35–43. doi:10.1111/j.1365-2834.2009.01064.x [DOI] [PubMed] [Google Scholar]
- Cox C. (1997). Findings from a statewide program of respite care: A comparison of service users, stoppers, and nonusers. The Gerontologist, 37, 511–517. doi:10.1093/geront/37.4.511 [DOI] [PubMed] [Google Scholar]
- Cox C. (1999). Service needs and use: A further look at the experiences of African American and white caregivers seeking Alzheimer’s assistance. American Journal of Alzheimer's Disease and Other Dementias, 14, 93–101. doi:10.1177/153331759901400202 [Google Scholar]
- Damiani G. Rosenbaum P. Swinton M., & Russell D (2004). Frequency and determinants of formal respite service use among caregivers of children with cerebral palsy in Ontario. Child: Care, Health & Development, 30, 77–86. doi:10.1111/j.1365-2214.2004.00391.x [DOI] [PubMed] [Google Scholar]
- DePasquale N. Davis K. D. Zarit S. H. K., Moen P. Hammer L. B., & Almeida D. M (2014). Combining formal and informal caregiving roles: The psychosocial stressors of double-and triple-duty caregiving. doi:10.1093/geronb/gbu139 [DOI] [PMC free article] [PubMed]
- DePasquale N. Polenick C. A. Davis K. D. Moen P. Hammer L. B., & Almeida D. M (2015). The psychosocial implications of managing work and family caregiving roles: Gender differences among information technology professionals. doi:10.1177/0192513X15584680. [DOI] [PMC free article] [PubMed]
- Farhadi P. Sharifian R. Feili A., & Shokrpour N (2013). The effects of supervisors’ supportive role, job stress, and work-family conflicts on the nurses’ attitudes. The Health Care Manager, 32, 107–122. doi:10.1097/HCM.0b013e31828ef5e7 [DOI] [PubMed] [Google Scholar]
- Giles T. M., & Hall K. L (2014). Qualitative systematic review: The unique experiences of the nurse-family member when a loved one is admitted with a critical illness. Journal of Advanced Nursing, 70, 1451–1464. doi:10.1111/jan.12331. [DOI] [PubMed] [Google Scholar]
- Gottlieb B. H. Kelloway E. K., & Martin-Matthews A (1996). Predictors of work-family conflict, stress, and job satisfaction among nurses. Canadian Journal of Nursing Research, 28, 99–117. doi:10.1002/nur.20133 [PubMed] [Google Scholar]
- Harrington L., & Heidkamp M (2013). The aging workforce: Challenges for the healthcare industry workforce. New Brunswick, NJ: NTAR Leadership Center, Rutgers University. [Google Scholar]
- Herrera A. P. Lee J. Palos G., & Torres-Vigil I (2008). Cultural influences in the patterns of long-term care use among Mexican American family caregivers. Journal of Applied Gerontology, 27, 141–165. doi:10.1177/0733464807310682. [Google Scholar]
- Hessel P., & Keck W (2009). State of the art report: How caring for an adult person affects employment? Retrieved from http://www.equalsoc.org/264.
- Hilbe J.M. (2007). Negative binomial regression. New York: Cambridge University Press. [Google Scholar]
- Hinrichsen G. A., & Ramirez M (1992). Black and white dementia caregivers: A comparison of their adaptation, adjustment, and service utilization. The Gerontologist, 32, 375–381. doi:10.1093/geront/32.3.375. [DOI] [PubMed] [Google Scholar]
- Kessler R. C. Barker P. R. Colpe L. J. Epstein J. F. Gfroerer J. C. Hiripi E. … Zaslavsky A. M (2003). Screening for serious mental illness in the general population. Archives of General Psychiatry, 60, 184–189. doi:10.1001/archpsyc.60.2.184 [DOI] [PubMed] [Google Scholar]
- Kim S. S. Okechukwu C. A. Buxton O. M. Dennerlein J. T. Boden L. I. Hashimoto D. M., & Sorensen G (2013). Association between work-family conflict and musculoskeletal pain among hospital patient care workers. American Journal of Industrial Medicine, 56, 488–495. doi:10.1002/ajim.22120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King R. B. Karuntzos G. Casper L. M. Moen P. Davis K. D. Berkman L., …Kossek E. E (2012). Work-family balance issues and work-leave policies. In Gatchel R. J., Schultz I. Z. (Eds.), Handbook of occupational health and wellness. New York: Springer. [Google Scholar]
- Khatutsky G. Wiener J. M. Anderson W. L., & Porell F. W (2012). Work-related injuries among certified nursing assistants working in US nursing homes. Research Triangle Park, NC: RTI Press. [Google Scholar]
- Kosloski K., & Montgomery R. J. V (1994). Investigating patterns of service use by families providing care for dependent elders. Journal of Aging and Health, 6, 17–37. doi:10.1177/089826439400600102 [DOI] [PubMed] [Google Scholar]
- Leineweber C. Westerlund H. Chungkham H. S. Lindqvist R. Runesdotter S., & Tishelman C (2014). Nurses’ practice environment and work-family conflict in relation to burn out: A multilevel modelling approach. PLoS One, 9, e96991. doi:10.1371/journal.pone.0096991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letvak S. A. Ruhm C. J., & Gupta S. N (2012). Nurses’ presenteeism and its effects on self-reported quality of care and costs. American Journal of Nursing, 112, 30–38. doi:10.1097/01.NAJ.0000411176.15696f9 [DOI] [PubMed] [Google Scholar]
- Pani J. R., & Chariker J. H (2004). The psychology of error in relation to medical practice. Journal of Surgical Oncology, 88, 130–142. doi:10.1002/jso.20123. [DOI] [PubMed] [Google Scholar]
- Perlick D. A. Hohenstein J. M. Clarkin J. F. Kaczynski R., & Rosenheck R. A (2005). Use of mental health and primary care services by caregivers of patients with bipolar disorder: a preliminary study. Bipolar Disorders, 7, 126–135. doi:10.1111/j.1399-5618.2004.00172.x [DOI] [PubMed] [Google Scholar]
- Rantanen J. Mauno S. Kinnunen U. & Tement S (2013). Patterns of conflict and enrichment in work-family balance: A three-dimensional typology. Work & Stress, 27, 141–163. doi:10.1080/02678373.2013.791074 [Google Scholar]
- Robinson K. M. Buckwalter K. C., & Reed D (2005). Predictors of use of services among dementia caregivers. Western Journal of Nursing Research, 27, 126–140. doi:10.1177/0193945904272453 [DOI] [PubMed] [Google Scholar]
- Ross M.M. Rideout E., & Carson M (1996). Nurses’ work: Balancing personal and professional caregiving careers. Canadian Journal of Nursing Research, 26, 43–59. [PubMed] [Google Scholar]
- Rutman D. (1996). Caregiving as women’s work: Women’s experiences of powerfulness and powerlessness as caregivers. Qualitative Health Research, 6, 90–111. doi:10.1177/104973239600600106 [Google Scholar]
- Schubert C. C. Boustani M. Callahan C. M. Perkins A. J. Hiu S., & Hedrie H. C (2008). Acute care utilization by dementia caregivers within urban primary care practices. Journal of General Internal Medicine, 23, 1736–1740. doi:10.1007/s11606-008-0711-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott L. D. Hwang W.-T., & Rogers A. E (2006). The impact of multiple care giving roles on fatigue, stress, and work performance among hospital staff nurses. Journal of Nursing Administration, 36, 86–95. doi:10.1097/00005110-200602000-00007 [DOI] [PubMed] [Google Scholar]
- Son J. Erno A. Shea D.G. Femia E.E. Zarit S.H., & Stephens M.A.P (2007). The caregiver stress process and health outcomes. Journal of Aging and Health, 19, 871–887. doi:10.1177/0898264307308568. [DOI] [PubMed] [Google Scholar]
- St-Amant O. Ward-Griffin C. Brown J. B. Martin-Matthews A. Sutherland N. Keefe J., & Kerr M. S (2014). Professionalizing familial care: Examining nurses’ unpaid family care work. Advances in Nursing Science, 27, 117–131. doi:10.1097/ans.0000000000000023 [DOI] [PubMed] [Google Scholar]
- Surani S. Murphy J., & Shah A (2007). Sleepy nurses: Are we willing to accept the challenge today? Nursing Administration Quarterly, 31, 146–151. doi:10.1097/01.NAQ.0000264863.94958.40 [DOI] [PubMed] [Google Scholar]
- Sweet S. Pitt-Catsouphes M. Besen E. Hovhannisyan S., & Pasha F (2010). Talent pressures and the aging workforce: Responsive action steps for the health care and social assistance sector. Boston: Sloan Center on Aging & Work, Boston College. [Google Scholar]
- Tement S., & Korunka C (2015). The moderating impact of types of caregiving on job demands, resources, and their relation to work-to-family conflict and enrichment. Journal of Family Issues, 36, 31–55. doi:10.1177/0192513X13483971. [Google Scholar]
- Toseland R. W. McCallion P. Gerber T., & Banks S (2002). Predictors of health and human services use by persons with dementia and their family caregivers. Social Science & Medicine, 55, 1255–1266. doi:10.1016/S0277-9536(01)00240-4. [DOI] [PubMed] [Google Scholar]
- Wang M.-L., & Tsai L.-J (2014). Work-family conflict and job performance in nurses: The moderating effects of social support. Journal of Nursing Research, 22, 200–207. doi:10.1097/jnr.0000000000000040 [DOI] [PubMed] [Google Scholar]
- Ward-Griffin C. (2004). Nurses as caregivers of elderly relatives: Negotiating personal and professional boundaries. Canadian Journal of Nursing Research, 36, 92–114. [PubMed] [Google Scholar]
- Ward-Griffin C. Brown J. B. Vandervoort A. McNair S., & Dashnay I (2005). Double-duty caregiving: Women in the health professions. Canadian Journal of Aging, 24, 379–394, doi:10.1353/cja.2006.0015 [Google Scholar]
- Ward-Griffin C. St-Amant O., & Brown J. B (2011). Compassion fatigue within double duty caregiving: Nurse-daughters caring for elderly parents. Online Journal of Issues in Nursing, 16. [DOI] [PubMed] [Google Scholar]
- Ward-Griffin C. Brown J. B. St-Amant O. Sutherland N. Martin-Matthews A. Keefe J., & Kerr M (2015). Nurses negotiating professional-familial care boundaries: Striving for balance within double duty caregiving. Journal of Family Nursing, 21, 57–85. doi:10.1177/1074840714562645 [DOI] [PubMed] [Google Scholar]
- Williams J. A. (2013). Pain, productivity at work, and future medical expenditures: The role of supportive workplaces (Order No. 3564410). Retrieved from ProQuest Dissertations & Theses Full Text. (1412729535). [Google Scholar]